Chapter: Medicine Study Notes : Respiratory
Chronic Obstructive Pulmonary Disease (COPD)
Chronic Obstructive Pulmonary Disease (COPD)
·
= Increase resistance to air flow
due to partial or complete obstruction at any level
·
= Permanent or minimally
reversible obstruction of expiratory airflow caused by chronic bronchitis,
emphysema or both
·
Lung Function results:
o FEV1/FVC ratio < 70% with a concave expiratory loop
o RV
secondary to air trapping
o ¯DL CO due
to loss of parenchyma
o Severity:
§ Mild: FEV1 > 50% predicted
§ Moderate: FEV1 35 – 49% predicted
§ Severe: FEV1 < 35% predicted
·
Chest Xray:
o Emphysema: absent peripheral vessels, hypertranslucency, flattened
diaphragm, bullous change
o Bronchitis: thickened bronchial walls (especially end on)
·
Abnormalities in gas exchange:
·
Treatment:
o Only smoking cessation and long term oxygen alters the natural course
o No evidence that daily bronchodilators are beneficial in asymptomatic
patients
o 20% benefit from oral corticosteroids. Should be used primarily for
exacerbations. Inhaled steroids show no significant benefit
·
Management of an exacerbation:
o Exclude differentials: PE, LVF, pneumothorax, hyperventilation
o Is there an infective component: Upper or Lower RTI
o Are there complications of COPD:
§ Cor pulmonale/pulmonary hypertension (look for signs of RH failure)
§ Polycythaemia secondary to chronic hypoxia
§ Low body weight/osteoporosis (from steroids and acidosis)
o Investigations:
§ FBC (is Hb or WBC ), U & E, Glucose
§ ECG
§ If Sats < 92% then ABG
§ CXR
§ Sputum microscopy, culture and sensitivity
§ Peak flow is asthmatic component
§ Spirometry when resolved
§ Echo if cor pulmonale or LVF suspected
o Treatment:
§ O2 with goal of saturation 90 – 92% (beware CO2
narcosis)
§ Broncho dilation: Combivent
§ Antibiotics: Usually oral. Augmentin, erythromycin, etc. Commonly H
Influenzae or M Catarrhalis
§ Steroids: 30 – 40 mg/day, stepping down over around 2 weeks
Chronic Bronchitis
·
= Persistent cough with sputum
for at least 3 months in 2 consecutive years
·
Follows prolonged exposure of the
tracheobronchial trees to non-specific irritants ®
hypersecretion of mucus and structural changes
·
Types:
o Simple chronic bronchitis: no airway obstruction
o Chronic asthmatic bronchitis: intermittent bronchospasm and wheezing
o Chronic obstructive bronchitis: heavy smokers with chronic airways
obstruction, usually with emphysema. Sputum
will be clear/white, only occasionally will be infected (yellow/green)
o [Cf Chronic infective bronchitis with green sputum Þ
bronchiectasis]
·
Pathogenesis:
o Chronic irritation (eg inhaled substances such as smoking) and microbiological
infections ® hyper-secretion of mucus obstructing airways. Hypertrophy of submucosal
glands in larger bronchi and hyperplasia of goblet cells in small airways.
o Infection maintains the hyper-secretion and causes acute exacerbations
·
Macroscopic appearance:
hyperaemia, swelling, mucopurulent secretions in the bronchi
·
Microscopic appearance: increased
size of mucous glands. Reid index (ratio of mucous gland layer to thickness of
epithelium to cartilage) greater than 0.4. Chronic inflammation ® metaplasia
to squamous epithelium and dysplasia. Mucous plugging, inflammation and
fibrosis. If severe ® luminal obliteration
Emphysema
·
Enlargement of air-spaces distal
to terminal bronchioles and destruction of alveolar walls without fibrosis
·
Moderate to severe emphysema is
rare in non-smokers
·
Aetiology:
o Cigarettes: usually had a 20-pack year history. Only 15 – 20% of smokers develop obstruction
o Alpha-1 antitrypsin deficiency
o Dusts: coal, gold mining, textile, cement and steel making
·
FEV1 best single indicator of
prognosis
·
Pathogenesis: Disruption in
balance of elastin synthesis: in elastolytic activity from neutrophil elastase (smoking ® neutrophils)
and ¯a1-antitrypsin (elastase inhibitor – oxidants in cigarette smoke inhibit a1-antitrypsin).
Neutrophils also release free radicals that inhibit a1-antitrypsin
·
Types:
o Centriacinar (Centrilobular): enlargement of respiratory bronchioles,
distal alveoli are spared. (Small particles deposited here – don‟t make it
right to the end). More severe in upper lobes. Blackened. Bronchi and
bronchioles have chronic inflammation. Seen in smokers and coal workers
pneumoconiosis
o Panacinar (Panlobular): acinus is uniformly involved from respiratory
bronchiole to terminal alveoli. Seen in a1-antitrypsin deficiency (ZZ or
MZ alleles on chromosome 14) and as an extension of centrilobular emphysema in
smokers. Mean age of onset is 45 – 50 years in non-smokers and 30 – 40 in
smokers. Liver disease in 5 – 10 % of adults. Heterozygotes (MZ) predisposed to
emphysema if they smoke. Treatment same as for smoking induced
o Paraseptal (distal acinar): proximal acinus is normal, distal part
affected. Most prominent sub-pleurally and next to interlobular septi. Often
seen in cases of spontaneous pneumothorax in young people
o Irregular emphysema: acinus irregularly involved. Associated with scarring
·
Macroscopic appearance:
voluminous lungs
·
Microscopic appearance: large
abnormal airspaces, blebs and bullae.
Bronchitis and bronchiolitis
·
Clinical features:
o 60 years or older
o Prolonged history of exertional dyspnoea
o Minimal non-productive cough
o Usually have lost weight
o Use accessory muscles for respiration
o Prolonged expiration period (lungs collapse due to ¯elastin)
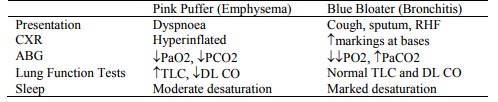
o Pink puffers: respiratory rate maintains O2. Xray: central pulmonary artery size, ¯peripheral vascular markings
o Blue bloaters: PaCO2, ¯PaO2, cyanotic, respiratory centre insensitive to CO2,
instead rely on hypoxic drive to breathe. Dangerous to give O2 ® ¯ventilatory
drive
·
Medical management:
o Bronchodilators and inhaled corticosteroids: only if reversible
obstruction
o Smoking cessation (nicotine replacement doubles quit rate)
o Antibiotics
o O2 with care
o Exercise/physio
o Attention to nutrition
Bronchiectasis
·
Chronic necrotising infection of
bronchi and bronchioles (ie a pneumonia
that doesn’t clear) ® abnormal airway dilation and destruction of bronchial walls ®
obstruction due to inflammation, ulceration and distortion
·
= Chronic infective bronchitis
·
Pathogenesis:
o Obstruction (especially during growth) due to tumour, foreign bodies,
mucous impaction (eg in cystic fibrosis and immotile cilia)
o Infection with bronchial wall weakening and atelectesis (eg in
necrotising pneumonia). Especially Tb, pertussis, MAC
·
Macroscopic appearance: affects
lower lobes, especially vertical airways and more distal bronchi. Airways may
be cylindrical, fusiform or saccular
·
Microscopic appearance: Acute –
inflammatory exudate with desquamation and ulceration of the epithelium. Chronic
– peribronchial fibrosis
·
Clinical course: foul, bloody
sputum, especially in the morning. (cf Clear
sputum in chronic bronchitis).
Repeated „bronchitis‟ with wheezing, haemoptysis, and dyspnoea. Coarse
crepitations, wheezing, and clubbing.
· Complications: obstructive ventilatory insufficiency ® dyspnoea and cyanosis. Rarely cor pulmonale, metastatic brain abscesses and amyloidosis
Related Topics