Chapter: Medicine Study Notes : Respiratory
Asthma
Asthma
· Is chronic and obstructive, but not usually categorised with CORD
History
· Viral infections likely to trigger asthma
· Night time cough and low peak flow can be asthma, ?hay-fever, a cold or bronchitis
· Ask about:
o Living situation
o Occupation
o Allergies, any pets?
o Seasonal
o Cold air
o Irritants (eg fumes)
o Exercise
o Night cough
o History of atopy: eczema
· Classic symptoms: SOB, wheeze, cough, tightness (like in angina)
Assessment
· Always do peak flow. Not the same as FEV1, which is more accurate. FEV1 of 50% of predicted = PF of 70% predicted
· If can‟t get a wheeze on auscultation, then take a big breath and blow out fast to elicit wheeze (=Forced End Expiratory Wheeze). Also listen to heart to ensure it‟s not a cardiac cause
· Can you demonstrate reversible bronchial constriction? If peak flow (or FEV1 if spirometry available) by 15% (60 – 70 litre/min) following bronchodilator. Do best of 3 peak flows, then repeat 15 minutes (= peak response time) after >= 2 doses of a reliever
· There will be significant pathology even if mild: pseudo stratified epithelium gone, thickened basement membrane, eosinophils, hypertrophy of smooth muscle and glands, mucus
· High-risk asthmatic (markers of risk of death):
o Hospital admission in last 12 months
o Previous life threatening attack
o Repeated self-administration of high doses of reliever (eg requesting 2 or more reliever prescriptions per month)
· Precipitating factors in a life-threatening attack:
o In kids (80%) and adults (30%): viral URTI. Most commonly rhinoviruses and coronaviruses
o („common cold‟)
o Allergen exposure in a sensitised individual
o Drug sensitivity, eg aspirin
· If severe, then ?other causes: PE, pneumothorax, etc
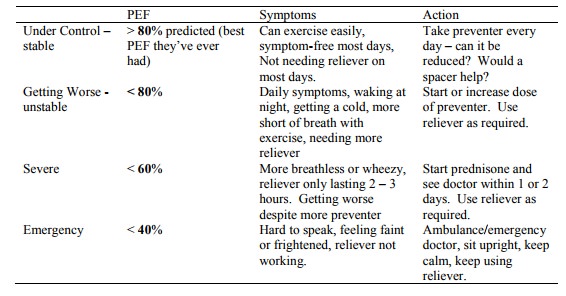
Classification of severity
· How they feel (ie breathlessness) does NOT correlate to severity (as measured by FEV1). Due to temporal adaptation – if chronically breathless, body turns off perception of breathlessness (cf don‟t hear trains if living by a railway line). Unless you MEASURE lung function, you CANNOT assess severity. However, in kids have to rely on symptoms as peak flow unreliable
· Key time to measure peak flow is when asthma is getting worse. No one will do it all the time so don‟t ask them to
Asthma in Young Children
· especially for Medication and Spacer Use
· 3rd most common reason for admission (after Bronchiolitis and URTI/Otitis media).
· Much much less common in < 1 years (NB bronchiolitis causes wheezing in young). Peak in 2 – 4 years
· Peak flow very unreliable under age 7 (and most bad asthmatics diagnosed from 2 – 5) ® have to rely on history
· History:
o Symptoms: waking at night with cough/wheeze, after exercise, how often are attacks, had time off school/kindy as a result, how long does preventer last
o Environmental factors: smokers, pets, damp, obvious triggers
o Current treatment: medicines, do the family understand the difference between reliever and preventer, assess technique and compliance, is spacer accepted by child and is it washed
· 2 patterns on history:
o Episodic (intermittent): viral URTI ® cough and wheeze. No interval symptoms
o Persistent (with exacerbations): interval symptoms (with exercise, at night), exacerbations with viral infection, interferes with everyday life
· Symptoms in a toddler:
o Cough, often worse at night
o May vomit with cough (NB exclude pertussis: cough ® choke ® vomit ® OK for an hour. In asthma, cough again straight away)
o Usually wheezy with URT infection
o Diagnosis difficult in an infant unless recurrent, strong immediate family history or evidence of atopy
· Physical findings in a toddler:
o Often normal chest exam
o If severe chronic symptoms:
§ Hyperinflated chest ( AP diameter)
§ Harrison‟s sulcus: dip in chest wall where diaphragm attaches
§ Eczema
§ Reduced growth (if severe)
o Stethoscope can be confusing
· Diagnosis:
o Cough is very common in kids (8 – 10 per year). But more during the day than at night. Won‟t slow them down when running
o Is it asthma, bronchitis, bronchiolitis?
o Trial of therapy (preventative as well as relievers) and review
· Criteria for admission:
o Pulse rate > 1.5 * normal
o Respiratory rate > 70 minute
o Chest movements
o Restlessness/apathy/CNS depression or cyanosis/pallor [signs of exhaustion]
· Treatment:
o Avoid triggers: passive smoking, pets, house dust mite (dehumidifiers don‟t work), pollens, cold, exercise, damp houses, certain foods (overstated)
o Infrequent episodic asthma:
§ Consider no therapy, avoid triggers
§ If distressed with attacks: use bronchodilators + spacer only. Start during URTI phase. No preventative
o Frequent Episodic Asthma (only get it with a cold):
§ Intervals between attacks < 6 weeks
§ Bronchodilator as needed with URTIs
§ Prophylaxis:
§ Sodium cromoglycate (Vicrom + spacer). ?Evidence of poor efficacy
§ Nedocromil (Tilade + spacer)
§ Inhaled steroids: if it makes no difference then stop
· Persistent Asthma
o Male: female = 4:1
o Preventative. If mild try Vicrom or Tilade. Moderate or severe use inhaled steroids (takes 2 – 3 months for maximal effect). Titrate back once controlled
o Bronchodilators as required
o Poor control: consider dose, check inhaler device and technique, poor compliance, environmental triggers
· Other treatment options:
o Long-acting b-agonists: salmeterol (Serevent), eformoterol (Foradil, Oxis)
o Theophylline (Nuelin, Theodur): 3rd line, gut ache ® poor compliance
o If severe: alternate day oral prednisone treatment – reduced side effects (short and fat), and reasonable asthma control
· Protocol for an acute attack:
o Salbutamol dose: up to 5 years: 6 puffs via space. Over age 5: 12 puffs via space
o For severe add ipratropium (Atrovent)
o For moderate and severe, give doses at 0, 20, 40 and 60 minutes and review at 75 minutes
o Oral Steroid for all except minor attacks: 1 mg/Kg/day ® ¯relapse
Principles of management
· Asthma self-management plans are recommended as essential in the long-term treatment of adult asthma. Those with formal management plans have half the morbidity of those without them, despite the same treatment
· Also need to establish, avoid and control triggers
· Factors associated with asthma deaths:
o Long term:
§ Lack of appreciation of chronic asthma severity and risk
§ Poor compliance
§ Discontinuity of medical care
§ Under utilisation of inhaled steroids
o Fatal attack:
o Delay in seeking medical help
o Inability to recognise severity
o Over-reliance on bronchodilator
o Insufficient systemic steroid use
o Lack of written information
· If the management plan is too complicated for the patient, modify (eg just the point at which to see the doctor)
· Compliance is critical Þ ownership of treatment by the patient is fundamental – negotiate and educate
Treatment
· Status asthmaticus: severe acute asthma that does not respond to treatment.
·
Most important part is use of
inhaled corticosteroid. Patient may favour reliever (it obviously does
something – reinforce that preventer stops it happening to start with)
·
Inhaled Corticosteroids:
o Action: Anti-inflammatory and ¯hyper-reactivity
o Effect: lung function, ¯symptoms, ¯admissions (only drug to do this)
o If using a b-agonist most days then should be on an inhaled steroid
o Doses:
§ 200 to 1000 mg/day of Beclomethasone Dipropionate (BDP/Becotide) or Budesonide
(BUD/Pulmicort), or
§ 100 to 500 mg/day of Fluticasone Propionate (Flexatide - only difference is potency,
not efficacy, ?¯side effects)
§ Starting dose: if steroid naïve, better to start low and step up not
start high and step down – too hard to wind it back
§ Back titration: in stable patients back titration may be attempted. ½
dose as a one off. If cut too far too fast can rebound within a month. Stopping
treatment altogether is likely to cause a relapse
o Doses by severity:
§ Stable: inhaled steroid bd, b agonist prn. If well controlled
can take total steroid dose once a day at night rather than bd ® better
compliance
§ Unstable: inhaled steroid qid, b agonist prn. If still not
controlled then oral theophylline at night or long acting b agonist
§ Severe: systemic steroids, high dose b agonist, O2, medical
review. Bronchodilators and inhaled steroids don‟t work so well in severe
asthma as the major cause of obstruction is mucus plugging and the drugs don‟t
get through. Steroid dose: start early (takes approx 12 hours to have an
effect), 0.4 – 0.6 mg/kg/day = 40 mg for normal adult. In practice: 30 – 40
mg/day until PEF normal, then 20 mg/day for as many days again
o Side-effects: Dose dependent redistribution of fat, electrolyte disturbances,
hypertension (ie
o Cushing‟s features), stunted growth in children
·
Bronchodilator:
o Reliever. Short acting inhaled b agonist.
o Potent and rapid bronchodilator and a relatively low toxicity. Relaxes
airway smooth muscles (plus other effects, e.g. ¯release
of mast cell mediators). Adverse effects: muscle tremour and tachycardia
common. Use as needed – not regularly – then becomes a guide to severity
o Salbutamol and terbutaline sulphate common.
o Long acting agonists for more severe asthmatics: Salmeterol and
Eformoterol (similar effect but potency). Peak effect 2 – 4
hours, duration 9 – 12 hours.
o Theophylline:
§ May have additive effect with b agonist, but risk of
side effects (including ¯K).
§ Narrow TI.
§ T½ in
heart and liver failure, viral infections, elderly, enzyme inhibitors eg:
cimitidine, erythromycin, contraceptives
§ ¯T½ in
smokers, chronic alcohol, phenytoin, carbamazepine, rifampicin, and
barbiturates
§ Given IV (very slowly) as aminophylline (too irritant for IM) for severe
attack unresponsive to nebuliser
·
Others:
o Sodium cromoglicate: non-steroidal preventer – less effective than
steroids but fewer side effects. Single dose good for prevention of exercise
induced asthma
o Anti-leukotrienes: Leukotrienes ® vascular permeability, mucus
production, ¯mucus transport, etc. Oral montelukast ® 15 % in FEV1,
¯use of b agonist. Place in therapy still uncertain
·
Follow-up (eg good liaison with
GP) following emergency admission is critical to preventing recurrence
Inhalers
·
Advantages: minimum possible
dose, highly targeted, patient controls therapy
·
Inhaled steroids ®
deposition in mouth. If not using spacer, need to rinse, gargle and spit
otherwise risk of thrush and croaky voice. At best, 10% gets to lower airways
without spacer
·
Metered dose inhalers (MDI):
o Autohaler: shake, push lever up, suck. Lower level of suck needed than
powder inhalers – but still require good suck to get lower airways deposition.
As expensive as powder inhalers. OK from age 8 upwards
o Standard MDI: (cheap, light and rapid delivery of drug, but
co-ordination difficult). From age 12 onwards. Instructions for use:
§ Shake an inhaler between each puff
§ Remove cap
§ Hold it upright and pointed backwards
§ Breath out
§ Fire during 1st 25% of long slow inhalation
§ Hold breath
§ Breath out after removing inhaler from mouth
·
Inhalers through a spacer:
o As effective as a nebuliser.
Increases LRT deposition by 4 times
o Eliminate oral deposition of steroids and lung
deposition of both preventers and relievers
o Breath-a-tech with a facemask up to 6. Remove mask as soon as you can
(stops nasal filtering – try at age 4 - 5). Need smaller spacer as they have a
small tidal volume
o Volumatic without facemask. Need to be able to mouth breath well (ie try
from age 2 – 3 onwards)
o Need to inhale within 30 seconds of a puff into the space
o One puff at a time
o But plastic spacer ® static charge ® particles stick. So wash in detergent once a week and do not rinse
bubbles off (® microfilm of detergent)
o If using a new space without washing, need to prime it (10 puffs). Don‟t do this in front of patient
·
Dry Powder Inhalers: oral
deposition. Use from age 5 up (good for
use at school when they don‟t
·
want to lug a spacer around but
their MDI technique is inadequate).
Advantages: light, quick delivery,
·
don‟t need co-ordination, CFC
free. Disadvantages: cost, require high
respiratory flow
o Accuhaler: 60 doses, easy to use, has dose meter
o Disk haler: 6 doses
o Turbohaler: easier to use than disk haler. Red mark inside indicates when its empty
Related Topics