Chapter: Medicine and surgery: Genitourinary system
Prostate cancer - Genitourinary oncology
Prostate cancer
Definition
Adenocarcinoma of the prostate.
Prevalence
Second most common malignancy in men. Causes 11% of cancer deaths (>8000 pa).
Age
>50 years (40% > 70 years, 60% > 80 years)
Sex
Male
Geography
Varies by population (90x). Most common in Afro Caribbeans, common in Europe, rare in Orientals.
Aetiology
Predisposing factors include age, ethnicity, family history, genetic factors and diet, with a diet high in animal fat, low in vegetables showing an increased risk, but omega fatty acids (found in oily fish), selenium and vitamin E appear to be protective.
Pathophysiology
The cancer is commonly androgen-dependent, but there is no evidence that its growth is driven by a hormone imbalance in an individual. However, population studies have shown that men with higher testosterone levels appear to be at greater risk of prostate cancer.
Clinical features
Bladder outflow obstruction occurs late, when tumour has extended to the transurethral area. The tumour may cause irritative as well as obstructive symptoms, i.e. urinary urgency, frequency, nocturia, hesitancy and slow flow.
In most cases it is diagnosed either on rectal examination as the finding of an asymmetric prostate, a nodule or a hard, irregular craggy mass, often altering the median groove. Increasingly, prostate cancer is diagnosed because of the finding of a raised prostate specific antigen (PSA).
Occasionally, it may present with haematospermia, especially in older men, or as metastatic disease with an occult primary.
Macroscopy
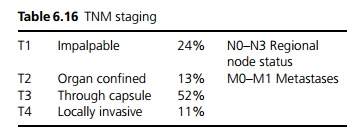
The tumours usually are in the peripheral zone of the prostate and appear as hard yellow-white gritty tissue (see Table 6.16).
Microscopy
Most are well differentiated and consist of small acini in a glandular pattern. Immunohistochemical techniques have also been developed, which can help identify whether cells are malignant and if they are of prostatic origin (e.g. if found in bone or lymph node biopsies).
Gleason score: The biopsy material is examined under a microscope and a Gleason grade 1ŌĆō5 (grade 1 being most differentiated, grade 5 the least) is assigned to the two most commonly occurring patterns of cells. These two grades are then added together to give the Gleason score (2ŌĆō10). A combined Gleason score of 2 + 3 = 5, means that there is predominantly grade 2 and 3 disease present in the biopsy.
┬Ę 2, 3, 4 ŌĆō Well differentiated, low grade.
┬Ę 5, 6, 7 ŌĆō Moderately differentiated.
┬Ę 8, 9, 10 ŌĆō Poorly differentiated, high grade.
Complications
Urinary tract infection and renal tract obstruction may occur, which can lead to renal failure.
Spread may be local or distant:
┬Ę Local spread is usually outward through the capsule.
┬Ę Lymphatic spread to pelvic and paraaortic nodes.
┬Ę Vascular spread, mainly to bone (classically sclerotic lesions), lung and liver.
Investigations
TRUS (Transrectal ultrasound) and biopsy: Needle biopsy of the outer prostate by transrectal route is more sensitive than transurethral route. The tumour may be hyper, iso- or hypo-echogenic.
Raised serum PSA: >4 ng/mL is abnormal. Benign prostatic hypertrophy, inflammation or biopsy of the prostate may also cause a raised PSA.
CT abdomen and pelvis to look for local invasion and lymph node involvement, and a bone scan to look for bony metastases.
Serum alkaline phosphatase (ALP) is usually raised when there are bony metastases.
Management
This depends on the tumour staging, grade and also on the patientŌĆÖs age and co-morbidity, as many of the treatments have significant side effects.
Organ-confined, low-grade disease:
These tumours tend to grow slowly, in older patients (>70 years) and those likely to die of co-morbidity before the cancer causes significant symptoms or metastasises, it may be reasonable to ŌĆśwatch and waitŌĆÖ.
Younger patients should have radical treatment with the intent to cure: radical prostatectomy and/or radio-therapy to the prostate and local nodes. However, radical surgery is a major operation, with a 60% incidence of impotence (compared to 16% preoperatively) and an increase in urinary incontinence. Radiotherapy can also cause complications such as acute and chronic radiation proctitis (diarrhoea, urgency, bleeding), and
impotence in 40ŌĆō50%.
Locally advanced (T3 or T4) disease:
For local symptom control TURP, radical prostatectomy or radiotherapy (external or brachytherapy) may be used, but recurrence and spread will almost certainly occur, so hormone therapy (see below) is generally advised with or without surgery.
Metastatic or high grade local disease:
Treatment is for symptoms only (palliative). The aim is to deplete the cancer of circulating androgens:
i. Bilateral orchidectomy is often declined by patients due to psychological reasons and there are now other medical alternatives.
ii. LHRH agonists are given parenterally and are equally effective as orchidectomy, the second choice is the use of oral anti-androgens, e.g. cyproterone, flutamide, or the two classes may be combined.
iii. Oestrogen therapy is less popular now, due to the excess risk of cardiovascular deaths.
iv. Chemotherapy is not as effective and is used mainly for non-responsive disease.
Throughout treatment a multidisciplinary approach is needed with regard to palliation of symptoms. Bis-phosphonates are used for bone pain and to prevent fractures. Localised radiation is used for bone pain and recently bone-targeting radioisotopes have been developed for those with multiple metastases.
Prognosis
Depends on grade, volume of primary and TNM staging; 50% present with incurable disease. If confined to prostate: 80% have 5-year survival and 60% have 10-year survival. If metastases are present: 20% have 5-year survival and 10% have 10-year survival.
Related Topics