Chapter: Medical Physiology: Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Physiologic Control of Glomerular Filtration and Renal Blood Flow
Physiologic Control of Glomerular Filtration and Renal Blood Flow
The determinants of GFR that are most variable and subject to physiologic control include the glomerular hydrostatic pressure and the glomerular capillary colloid osmotic pressure. These variables, in turn, are influenced by the sympathetic nervous system, hor-mones and autacoids (vasoactive substances that are released in the kidneys and act locally), and other feedback controls that are intrinsic to the kidneys.
Sympathetic Nervous System Activation Decreases GFR
Essentially all the blood vessels of the kidneys, includ-ing the afferent and the efferent arterioles, are richly innervated by sympathetic nerve fibers. Strong activa-tion of the renal sympathetic nerves can constrict the renal arterioles and decrease renal blood flow and GFR. Moderate or mild sympathetic stimulation has little influence on renal blood flow and GFR. For example, reflex activation of the sympathetic nervous system resulting from moderate decreases in pressure at the carotid sinus baroreceptors or cardiopulmonary receptors has little influence on renal blood flow or GFR.
The renal sympathetic nerves seem to be most important in reducing GFR during severe, acute dis-turbances lasting for a few minutes to a few hours, such as those elicited by the defense reaction, brain ischemia, or severe hemorrhage. In the healthy resting person, sympathetic tone appears to have little influ-ence on renal blood flow.
Hormonal and Autacoid Control of Renal Circulation
There are several hormones and autacoids that can influence GFR and renal blood flow, as summarized in Table 26–4.
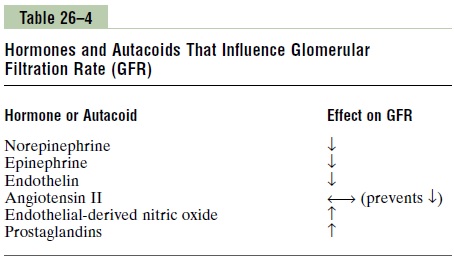
Norepinephrine, Epinephrine, and Endothelin Constrict Renal Blood Vessels and Decrease GFR. Hormones that constrictafferent and efferent arterioles, causing reductions in GFR and renal blood flow, includenorepinephrine and epinephrine released from the adrenal medulla. Ingeneral, blood levels of these hormones parallel the activity of the sympathetic nervous system; thus, nor-epinephrine and epinephrine have little influence on renal hemodynamics except under extreme conditions, such as severe hemorrhage.
Another vasoconstrictor, endothelin, is a peptide that can be released by damaged vascular endothelial cells of the kidneys as well as by other tissues. The physiologic role of this autacoid is not completely understood. However, endothelin may contribute to hemostasis (minimizing blood loss) when a blood vessel is severed, which damages the endothelium and releases this powerful vasoconstrictor. Plasma endothelin levels also are increased in certain disease states associated with vascular injury, such as toxemia of pregnancy, acute renal failure, and chronic uremia, and may contribute to renal vasoconstriction and decreased GFR in some of these pathophysiologic conditions.
Angiotensin II Constricts Efferent Arterioles. A powerfulrenal vasoconstrictor, angiotensin II, can be consid-ered a circulating hormone as well as a locally pro-duced autacoid because it is formed in the kidneys as well as in the systemic circulation. Because angiotensin II preferentially constricts efferent arteri-oles, increased angiotensin II levels raise glomerular hydrostatic pressure while reducing renal blood flow. It should be kept in mind that increased angiotensin II formation usually occurs in circumstances associ-ated with decreased arterial pressure or volume depletion, which tend to decrease GFR. In these cir-cumstances, the increased level of angiotensin II, by constricting efferent arterioles, helps prevent decreases in glomerular hydrostatic pressure and GFR; at the same time, though, the reduction in renal blood flow caused by efferent arteriolar constriction contributes to decreased flow through the peritubular capillaries, which in turn increases reabsorption of sodium and water.
Thus, increased angiotensin II levels that occur with a low-sodium diet or volume depletion help preserve GFR and maintain normal excretion of metabolic waste products such as urea and creatinine that depend on glomerular filtration for their excretion; at the same time, the angiotensin II–induced constriction of efferent arterioles increases tubular reabsorption of sodium and water, which helps restore blood volume and blood pressure. This effect of angiotensin II in helping to “autoregulate”.
Endothelial-Derived Nitric Oxide Decreases Renal Vascular Resistance and Increases GFR. An autacoid that de-creases renal vascular resistance and is released by the vascular endothelium throughout the body isendothe-lial-derived nitric oxide. A basal level of nitric oxideproduction appears to be important for maintaining vasodilation of the kidneys. This allows the kidneys to excrete normal amounts of sodium and water. There-fore, administration of drugs that inhibit this normal formation of nitric oxide increases renal vascular resistance and decreases GFR and urinary sodium excretion, eventually causing high blood pressure. In some hypertensive patients, impaired nitric oxide pro-duction could be the cause of increased renal vaso-constriction and increased blood pressure.
Prostaglandins and Bradykinin Tend to Increase GFR. Hormones and autacoids that cause vasodilation and increased renal blood flow and GFR include the prostaglandins (PGE2 and PGI2) and bradykinin. Although these vasodilators do not appear to be of major importance in regulating renal blood flow or GFR in normal conditions, they may dampen the renal vasoconstrictor effects of the sympathetic nerves or angiotensin II, especially their effects to constrict the afferent arterioles.
By opposing vasoconstriction of afferent arterioles, the prostaglandins may help prevent excessive reduc-tions in GFR and renal blood flow. Under stressful conditions, such as volume depletion or after surgery, the administration of nonsteroidal anti-inflammatory agents, such as aspirin, that inhibit prostaglandin syn-thesis may cause significant reductions in GFR.
Related Topics