Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Trauma
Nursing Process: The Patient Undergoing an Amputation
NURSING PROCESS: THE PATIENT
UNDERGOING AN AMPUTATION
Assessment
Before surgery, the
nurse must evaluate the neurovascular and func-tional status of the extremity
through history and physical assess-ment. If the patient has experienced a
traumatic amputation, the nurse assesses the function and condition of the
residual limb. The nurse also assesses the circulatory status and function of
the unaf-fected extremity. If infection or gangrene develops, the patient may
have associated enlarged lymph nodes, fever, and purulent drainage. A culture
is taken to determine the appropriate antibiotic therapy.
The nurse evaluates the
patient’s nutritional status and creates a plan for nutritional care, if
indicated. For wound healing, a bal-anced diet with adequate protein and
vitamins is essential.
Any concurrent health
problems (eg, dehydration, anemia, car-diac insufficiency, chronic respiratory
problems, diabetes mellitus) need to be identified and treated so that the
patient is in the best possible condition to withstand the trauma of surgery.
The use of corticosteroids, anticoagulants, vasoconstrictors, or vasodilators
may influence management and wound healing.
The nurse assesses the patient’s psychological status.
Deter-mination of the patient’s emotional reaction to amputation is es-sential
for nursing care. Grief response to a permanent alteration in body image is
normal. An adequate support system and pro-fessional counseling can help the
patient cope in the aftermath of amputation surgery.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Acute pain related to
amputation
·
Risk for disturbed sensory
perception: phantom limb pain related to amputation
·
Impaired skin integrity related
to surgical amputation
·
Disturbed body image related
to amputation of body part
·
Ineffective coping, related to
failure to accept loss of body part
·
Risk for anticipatory and/or
dysfunctional grieving related to loss of body part
·
Self-care deficit: feeding,
bathing/hygiene, dressing/grooming, or toileting, related to loss of extremity
·
Impaired physical mobility
related to loss of extremity
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications
that may develop include the following:
·
Postoperative hemorrhage
·
Infection
·
Skin breakdown
Planning and Goals
The major goals of the patient may include relief of
pain, absence of altered sensory perceptions, wound healing, acceptance of
al-tered body image, resolution of the grieving process, indepen-dence in
self-care, restoration of physical mobility, and absence of complications.
Nursing Interventions
RELIEVING PAIN
Surgical pain can be effectively controlled with opioid
analgesics, nonpharmaceutical interventions, or evacuation of the hematoma or
accumulated fluid. Pain may be incisional or may be caused by inflammation,
infection, pressure on a bony prominence, or hematoma. Muscle spasms may add to
the patient’s discomfort. Changing the patient’s position or placing a light
sandbag on the residual limb to counteract the muscle spasm may improve the
pa-tient’s level of comfort. Evaluation of the patient’s pain and re-sponses to
interventions is an important part of the nurse’s role in pain management. The
pain may be an expression of grief and alteration of body image.
MINIMIZING ALTERED SENSORY PERCEPTIONS
Amputees may experience
phantom limb pain soon after surgery or 2 to 3 months after amputation. It
occurs more frequently may in above-knee amputations. The patient describes
pain or un-usual sensations, such as numbness, tingling, or muscle cramps, as
well as a feeling that the extremity is present, crushed, cramped, or twisted
in an abnormal position. When a patient describes phantom pains or sensations,
the nurse acknowledges these feel-ings and helps the patient modify these
perceptions.
Phantom sensations
diminish over time. The pathogenesis of the phantom limb phenomenon is unknown.
Keeping the patient active helps decrease the occurrence of phantom limb pain.
Early intensive rehabilitation and stump desensitization with kneading massage
brings relief. Distraction techniques and activity are help-ful. Transcutaneous
electrical nerve stimulation (TENS), ultra-sound, or local anesthetics may
provide relief for some patients. In addition, beta-blockers may relieve dull,
burning discomfort; anti-seizure medications control stabbing and cramping
pain; and tri-cyclic antidepressants are used to improve mood and coping
ability.
PROMOTING WOUND HEALING
The residual limb must be handled gently. Whenever the dress-ing is changed, aseptic technique is required to prevent wound infection and possible osteomyelitis.
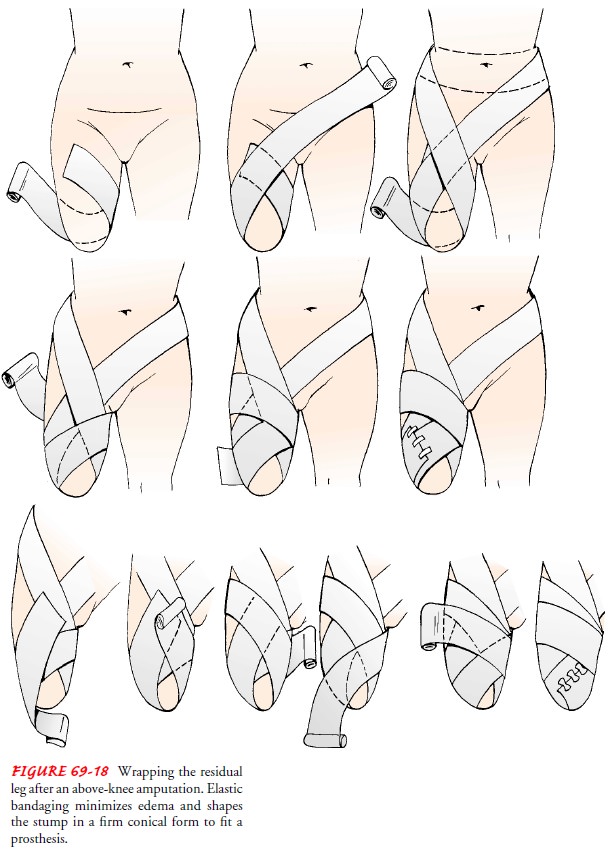
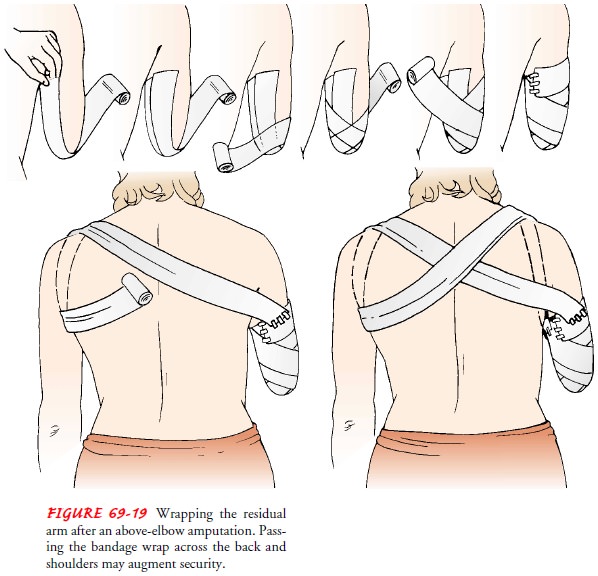
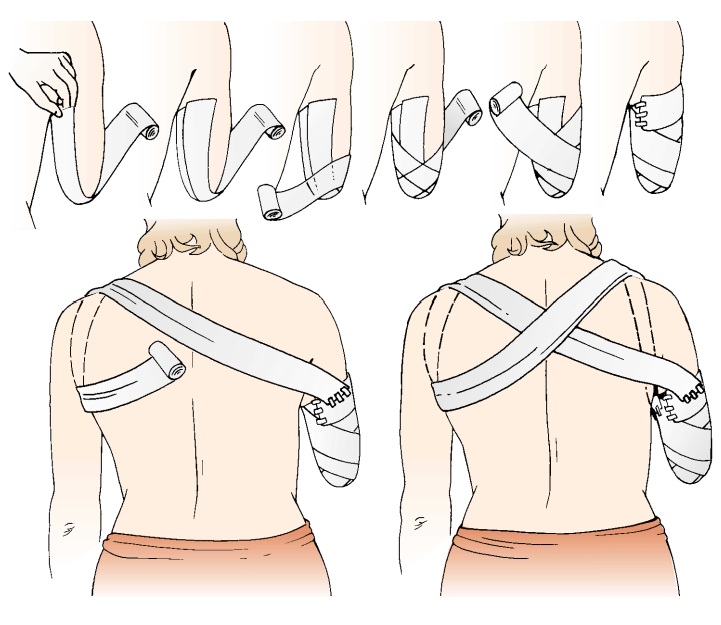
Residual limb shaping is important for prosthesis
fitting. The nurse instructs the patient and family in wrapping the residual
limb with elastic dressings (Figs. 69-18 and 69-19). After the in-cision is
healed, the nurse teaches the patient to care for the resid-ual limb.
ENHANCING BODY IMAGE
Amputation is a reconstructive procedure that alters the patient’s body image. The nurse who has established a trusting relationship with the patient is better able to communicate acceptance of the patient who has experienced an amputation. The nurse encour-ages the patient to look at, feel, and then care for the residual limb. It is important to identify the patient’s strength and resources to facilitate rehabilitation. The nurse assists the patient to regain the previous level of independent functioning. The patient who is ac-cepted as a whole person is more readily able to resume responsi-bility for self-care; self-concept improves, and body-image changes are accepted. Even with highly motivated patients, this process may take months.
HELPING THE PATIENT TO RESOLVE GRIEVING
The loss of an extremity
(or part of one) may come as a shock even if the patient was prepared
preoperatively. The patient’s behavior (eg, crying, withdrawal, apathy, anger)
and expressed feelings (eg, depression, fear, helplessness) will reveal how the
patient is cop-ing with the loss and working through the grieving process. The
nurse acknowledges the loss by listening and providing support.
The nurse creates an accepting and supportive atmosphere
in which the patient and family are encouraged to express and share their
feelings and work through the grief process. The support from family and
friends promotes the patient’s acceptance of the loss. The nurse helps the
patient deal with immediate needs and become oriented to realistic
rehabilitation goals and future inde-pendent functioning. Mental health and
support group referrals may be appropriate.
PROMOTING INDEPENDENT SELF-CARE
Amputation of an extremity affects the patient’s ability
to pro-vide adequate self-care. The patient is encouraged to be an active
participant in self-care. The patient needs time to accomplish these tasks and
must not be rushed. Practicing an activity with consistent, supportive
supervision in a relaxed environment en-ables the patient to learn self-care
skills. The patient and the nurse need to maintain positive attitudes and to
minimize fatigue and frustration during the learning process.
Independence in dressing, toileting, and bathing (shower
or tub) depends on balance, transfer abilities, and physiologic toler-ance of
the activities. The nurse works with the physical therapist and occupational
therapist to teach and supervise the patient in these self-care activities.
The patient with an upper extremity amputation has
self-care deficits in feeding, bathing, and dressing. Assistance is provided
only as needed; the nurse encourages the patient to learn to do these tasks,
using feeding and dressing aids when needed. The nurse, therapists, and
prosthetist work with the patient to achieve maximum independence.
HELPING THE PATIENT TO ACHIEVE PHYSICAL MOBILITY
Positioning assists in preventing the development
of hip or knee joint contracture in the patient with a lower extremity
amputa-tion. Abduction, external rotation, and flexion of the lower ex-tremity
are avoided. Depending on the surgeon’s preference, the residual limb may be
placed in an extended position or elevated for a brief period after surgery.
The foot of the bed is raised to elevate the residual limb.
The nurse encourages the patient to turn from side to
side and to assume a prone position, if possible, to stretch the flexor
mus-cles and to prevent flexion contracture of the hip. The nurse discourages
sitting for prolonged periods, to prevent flexion con-tracture. The legs should
remain close together to prevent an abduction deformity.
Postoperative ROM
exercises are started early, because contrac-ture deformities develop rapidly.
ROM exercises include hip and knee exercises for below-knee amputations and hip
exercises for above-knee amputations. It is important that the patient
under-stand the importance of exercising the residual limb.
The upper extremities, trunk, and abdominal muscles are
ex-ercised and strengthened. The extensor muscles in the arm and the depressor
muscles in the shoulder play an important part in crutch walking. The patient
uses an overhead trapeze to change position and strengthen the biceps. The
patient may flex and extend the arms while holding weights. Doing push-ups
while seated strengthens the triceps muscles. Exercises, such as
hyper-extension of the residual limb, conducted under the supervision of the
physical therapist or occupational therapist, also aid in strengthening muscles
as well as increasing circulation, reducing edema, and preventing atrophy.
Because an upper extremity amputee uses both shoulders to
operate the prosthesis, the muscles of both shoulders are exercised. A patient
with an above-the-elbow amputation or shoulder dis-articulation is likely to
develop a postural abnormality caused by loss of the weight of the amputated
extremity. Postural exercises are helpful.
Strength and endurance are assessed, and activities are
in-creased gradually to prevent fatigue. As the patient progresses to
independent use of the wheelchair, use of ambulatory aids, or ambulation with a
prosthesis, the nurse emphasizes safety con-siderations. Environmental barriers
(eg, steps, inclines, doors, wet surfaces) are identified, and methods of
managing them are prac-ticed. It is important to anticipate, identify and
manage problems associated with the use of the mobility aids (eg, pressure on
the axillae from crutches, skin irritation of the hands from wheelchair use,
residual limb irritation from a prosthesis).
Amputation of the leg
changes the center of gravity; therefore, the patient may need to practice
position changes (eg, standing from sitting, standing on one foot). The patient
is taught transfer techniques early and is reminded to maintain good posture
when getting out of bed. A well-fitting shoe with a nonskid sole should be
worn. During position changes, the patient should be guarded and stabilized
with a transfer belt at the waist to prevent falling.
As soon as possible, the patient with a lower extremity
am-putation is assisted to stand between parallel bars to allow ex-tension of
the temporary prosthesis to the floor with minimal weight bearing. How soon
after surgery the patient is allowed to touch down the artificial foot depends
on the patient’s physical status and wound healing. As endurance increases and
balance is achieved, ambulation is started with the use of parallel bars or
crutches. The patient learns to use a normal gait, with the resid-ual limb
moving back and forth while the patient is walking with the crutches. To
prevent a permanent flexion deformity from occurring, the residual limb should not be held up in a flexed position.
The patient with an upper extremity amputation is taught
how to carry out the ADLs with one arm. The patient is started on one-handed
self-care activities as soon as possible. The use of a temporary prosthesis is
encouraged. The patient who learns to use the prosthesis soon after the
amputation is less dependent on one-handed self-care activities.
A patient with an upper
extremity amputation may wear a cotton T-shirt to prevent contact between the
skin and shoulder harness and to promote absorption of perspiration. The
pros-thetist advises about cleaning the washable portions of the harness.
Periodically, the prosthesis is inspected for potential problems.
The residual limb must be conditioned and shaped into a
con-ical form to permit accurate fit, maximum comfort, and function of the
prosthetic device. Elastic bandages, an elastic residual limb shrinker, or an
air splint is used to condition and shape the resid-ual limb. The nurse teaches
the patient or a member of the family the correct method of bandaging.
Bandaging supports the
soft tissue and minimizes the forma-tion of edema while the residual limb is in
a dependent position. The bandage is applied in such a manner that the
remaining muscles required to operate the prosthesis are as firm as possible,
whereas those muscles that are no longer useful atrophy. An improperly applied
elastic bandage contributes to circulatory prob-lems and a poorly shaped
residual limb.
Effective preprosthetic
care is important to ensure proper fitting of the prosthesis. The major
problems that can delay prosthetic fit-ting during this period are (1) flexion
deformities, (2) nonshrink-age of the residual limb, and (3) abduction deformities
of the hip.
The physician usually prescribes activities to condition
or “toughen” the residual limb in preparation for a prosthesis. The patient
begins by pushing the residual limb into a soft pillow, then into a firmer
pillow, and finally against a hard surface. The patient is taught to massage
the residual limb to mobilize the sur-gical incision site, decrease tenderness,
and improve vascularity. Massage is usually started once healing has occurred
and is first done by the physical therapist. Skin inspection and preventive
care are taught.
The prosthesis socket is custom molded to the residual
limb by the prosthetist. Prostheses are designed for specific activity lev-els
and patient abilities. Types of prostheses include hydraulic, pneumatic, biofeedback-controlled,
myoelectrically controlled, and synchronized prostheses.
Adjustments of the
prosthetic socket are made by the prosthetist to accommodate the residual limb
changes that occur during the first 6 months to 1 year after surgery. A light plaster
cast, an elastic bandage, or a shrinking sock is used to limit edema during
periods when the patient is not wearing the permanent prosthesis.
Some patients are not
candidates for a prosthesis and are thus nonambulatory
amputees. If use of a prosthesis is not possible, thepatient is instructed
in the use of a wheelchair to achieve indepen-dence. A special wheelchair
designed for patients who have had am-putations is recommended. Because of the
decreased weight in the front, a regular wheelchair may tip backward when the
patient sits in it. In an amputee wheelchair, the rear axle is set back about 5
cm (2 inches) to compensate for the change in weight distribution.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
After any surgery, efforts are made to reestablish
homeostasis and to prevent problems related to surgery, anesthesia, and
immobil-ity. The nurse assesses body systems (eg, respiratory,
gastrointes-tinal, genitourinary) for problems associated with immobility (eg,
pneumonia, anorexia, constipation, urinary stasis) and institutes corrective
management. Avoiding problems associated with im-mobility and restoring
physical activity are necessary for mainte-nance of health.
Massive hemorrhage due to a loosened suture is
the most threat-ening problem. The nurse monitors the patient for any signs or
symptoms of bleeding. It is also important to monitor the patient’s vital signs
and to observe the suction drainage.
Infection is
a frequent complication of amputation. Patientswho have undergone traumatic amputation
have a contaminated wound. The nurse administers antibiotics as prescribed. It
is im-portant to monitor the incision, dressing, and drainage for indi-cations
of infection (eg, change in color, odor, or consistency of drainage; increasing
discomfort). The nurse also monitors for systemic indicators of infection (eg,
elevated temperature) and promptly reports indications of infection to the
surgeon.
Skin breakdown may result from immobilization or from pres-sure from
various sources. The prosthesis may cause pressure areas to develop. The nurse
and the patient assess for breaks in the skin. Careful skin hygiene is
essential to prevent skin irritation, infec-tion, and breakdown. The healed
residual limb is washed and dried (gently) at least twice daily. The skin is
inspected for pres-sure areas, dermatitis, and blisters. If they are present,
they must be treated before further skin breakdown occurs. Usually, a resid-ual
limb sock is worn to absorb perspiration and to prevent direct contact between
the skin and the prosthetic socket. The sock is changed daily and must fit
smoothly to prevent irritation caused by wrinkles. The socket of the prosthesis
is washed with a mild detergent, rinsed, and dried thoroughly with a clean
cloth. The nurse advises the patient that the socket must be thoroughly dry
before the prosthesis is applied.
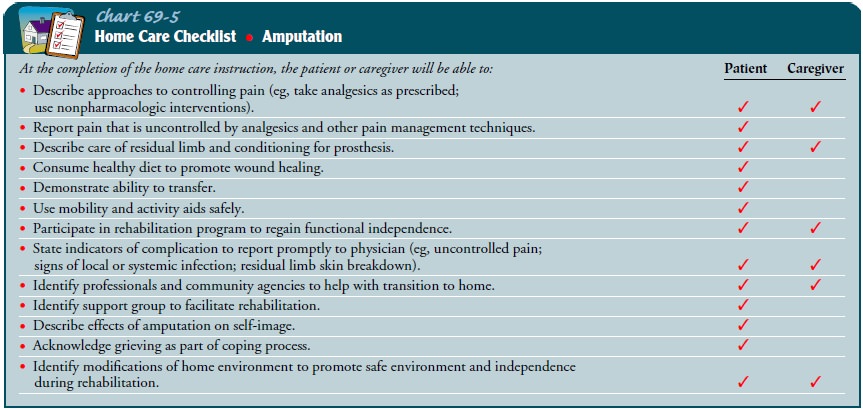
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching the Patient to Manage Self-Care
Before discharge to the home or to a rehabilitation
facility, the nurse encourages the patient and family to become active
parti-cipants in care. They participate, as appropriate, in skin care and
residual limb care and in the management of the prosthesis. The patient
receives ongoing instructions and practice sessions in learning how to transfer
and how to use mobility aids and other assistive devices safely. The nurse
explains the signs and symp-toms of complications that must be reported to the
physician (Chart 69-5).
Continuing Care in the Home and Community
After the patient has achieved physiologic homeostasis
and has demonstrated achievement of major health care goals, rehabili-tation
continues either in a rehabilitation facility or at home. Continued support and
supervision by the home care nurse are essential.
Before the patient’s
discharge to the home, the nurse should as-sess the home environment.
Modifications are made to ensure the patient’s continuing care, safety, and
mobility. An overnight or weekend experience at home may be tried to identify
problems that were not identified on the assessment visit. Physical therapy and
occupational therapy may continue in the home or on an out-patient basis.
Transportation to continuing health care appoint-ments must be arranged. The
social service department of the hospital or the community agency managing
continued health care may be of great assistance in securing personal
assistance and transportation services.
During follow-up health
visits, the nurse evaluates the patient’s physical and psychosocial adjustment.
Periodic preventive health assessments are necessary. Frequently, an elderly
spouse is unable to provide the assistance required, and additional help at
home is needed. Modifications in the plan of care are made on the basis of such
findings. Often, the patient and family find involvement in an amputee support
group to be of value; here, they are able to share problems, solutions, and
resources. Talking with those who have successfully dealt with a similar
problem may help the patient develop a satisfactory solution.
Because patients and their family members and health care
providers tend to focus on the most obvious needs and issues, the nurse reminds
the patient and family about the importance of continuing health promotion and
screening practices, such as reg-ular physical examinations and diagnostic
screening tests. Those patients who have not been involved in these practices
in the past are instructed in their importance and are referred to appropriate
health care providers.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Experiences
absence of pain
a) Appears
relaxed
b) Verbalizes
comfort
c) Uses
measures to increase comfort
d) Participates in self-care and rehabilitative activities
2) Experiences
absence of phantom limb pain
a) Reports
diminished phantom sensations
b) Uses
distraction techniques
c) Performs
stump desensitization massage
3) Achieves
wound healing
a) Controls
residual limb edema
b) Achieves
healed, nontender, nonadherent scar
c) Demonstrates
residual limb care
4) Demonstrates
improved body image and effective coping
a) Acknowledges
change in body image
b) Participates
in self-care activities
c) Demonstrates
increasing independence
d) Projects
self as a whole person
e) Resumes
role-related responsibilities
f) Reestablishes
social contacts
g) Demonstrates
confidence in abilities
5) Exhibits
resolution of grieving
a) Expresses
grief
b) Works
through feelings with family and friends
c) Focuses
on future functioning
d) Participates
in support group
6) Achieves
independent self-care
a) Asks
for assistance when needed
b) Uses
aids and assistive devices to facilitate self-care
c) Verbalizes
satisfaction with abilities to perform ADLs
7) Achieves
maximum independent mobility
a) Avoids
positions contributing to contracture development
b) Demonstrates
full active ROM
c) Maintains
balance when sitting and transferring
d) Increases
strength and endurance
e) Demonstrates
safe transferring technique
f) Achieves
functional use of prosthesis
g) Overcomes
environmental barriers to mobility
h) Uses
community services and resources as needed
8) Exhibits
absence of complications of hemorrhage, infection, skin breakdown
a) Does
not experience excessive bleeding
b) Maintains
normal blood values
c) Is
free of local or systemic signs of infection
d) Repositions
self frequently
e) Is
free of pressure-related problems
f) Reports
any skin discomfort and irritations promptly
Related Topics