Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Trauma
Amputation
Amputation
Amputation is
the removal of a body part, usually an extremity.Amputation of a lower
extremity is often made necessary by pro-gressive peripheral vascular disease
(often a sequela of diabetes mellitus), fulminating gas gangrene, trauma
(crushing injuries, burns, frostbite, electrical burns), congenital
deformities, chronic osteomyelitis, or malignant tumor. Of all these causes,
peripheral vascular disease accounts for most amputations of lower
extrem-ities.
Amputation is used to relieve symptoms, improve function,
and save or improve the patient’s quality of life. If the health care team
communicates a positive attitude, the patient adjusts to the amputation more
readily and actively participates in the rehabili-tative plan, learning how to
modify activities and how to use as-sistive devices for ADLs and mobility.
Levels of Amputation
Amputation is performed at the most distal point that
will heal successfully. The site of amputation is determined by two factors:
circulation in the part, and functional usefulness (ie, meets the requirements
for the use of the prosthesis).
The circulatory status
of the extremity is evaluated through physical examination and specific
studies. Muscle and skin per-fusion is important for healing. Doppler
flowmetry, segmental blood pressure determinations, and transcutaneous partial
pres-sure of oxygen (PaO2) are valuable diagnostic aids. Angiography is
performed if revascularization is considered an option.
The objective of surgery is to conserve as much extremity
length as possible. Preservation of knee and elbow joints is de-sired. Figure
69-16 shows the levels at which an extremity may be amputated. Almost any level
of amputation can be fitted with a prosthesis.
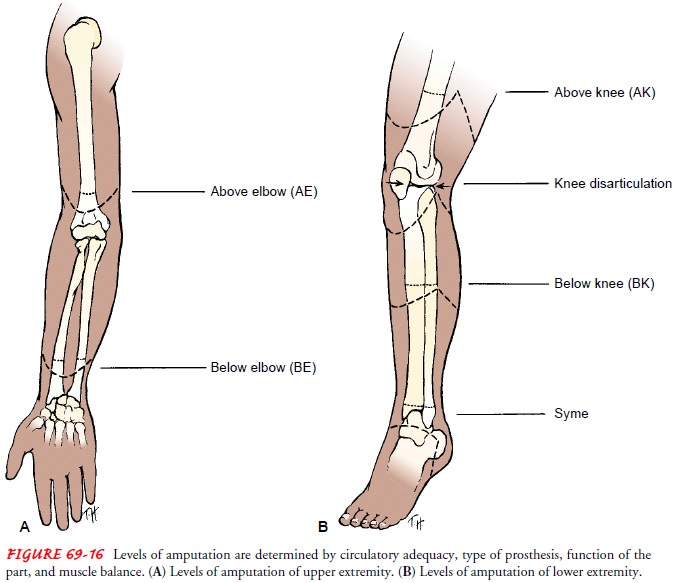
The amputation of toes
and portions of the foot causes minor changes in gait and balance. A Syme
amputation (modified ankle disarticulation amputation) is performed most
frequently for ex-tensive foot trauma and produces a painless, durable
extremity end that can withstand full weight-bearing. Below-knee amputations
are preferred to above-knee amputations because of the impor-tance of the knee
joint and the energy requirements for walking. Knee disarticulations are most
successful with young, active pa-tients who are able to develop precise control
of the prosthesis. When above-knee amputations are performed, all possible
length is preserved, muscles are stabilized and shaped, and hip contrac-tures
are prevented for maximum ambulatory potential. Most people who have a hip
disarticulation amputation must rely on a wheelchair for mobility.
Upper extremity amputations are performed to preserve the
maximum functional length. The prosthesis is fitted early for max-imum
function.
A staged amputation may be used when gangrene and infection exist.
Initially, a guillotine amputation is performed to remove the necrotic and
infected tissue. The wound is débrided and al-lowed to drain. Sepsis is treated
with systemic antibiotics. In a few days, after the infection has been
controlled and the patient’s con-dition has stabilized, a definitive amputation
with skin closure is performed.
Complications
Complications that may
occur with amputation include hemor-rhage,
infection, skin breakdown, phantom limb pain, and joint con-tracture. Because major blood vessels have been severed,
massivebleeding may occur. Infection is a risk with all surgical procedures.
The risk for infection increases with contaminated wounds after traumatic
amputation. Skin irritation caused by the prosthesis may result in skin
breakdown. Phantom limb pain is
caused by the severing of peripheral nerves. Joint contracture is caused by
positioning and a protective flexion withdrawal pattern associated with pain
and muscle imbalance.
Medical Management
The objective of treatment is to achieve healing of the amputa-tion wound, the result being a nontender residual limb (stump) with healthy skin for prosthesis use. Healing is enhanced by gentle handling of the residual limb, control of residual limb edema through rigid or soft compression dressings, and use of aseptic technique in wound care to avoid infection.
A closed rigid cast dressing is frequently used to provide uniform
compression, to support soft tissues, to control pain, and to pre-vent joint
contractures. Immediately after surgery, a sterilized residual limb sock is
applied to the residual limb. Felt pads are placed over pressure-sensitive
areas. The residual limb is wrapped with elastic plaster-of-paris bandages
while firm, even pressure is maintained. Care is taken not to constrict
circulation.
For the patient with a
lower extremity amputation, the plaster cast may be equipped to attach a
temporary prosthetic extension (pylon) and an artificial foot. This rigid
dressing technique is used as a means of creating a socket for immediate
postoperative pros-thetic fitting. The length of the prosthesis is tailored to
the indi-vidual patient. Early minimal weight bearing on the residual limb with
a rigid cast dressing and a pylon attached produces little dis-comfort. The
cast is changed in about 10 to 14 days. Elevated body temperature, severe pain,
or a loose-fitting cast may neces-sitate earlier replacement.
A removable rigid dressing may be placed over a soft dressing to
control edema, to prevent joint flexion contracture, and to pro-tect the
residual limb from unintentional trauma during transfer activities. This rigid
dressing is removed several days after surgery for wound inspection and is then
replaced to control edema. The dressing facilitates residual limb shaping.
A soft dressing with or without compression may be used if there is
significant wound drainage and frequent inspection of the resid-ual limb
(stump) is desired. An immobilizing splint may be incorporated in the dressing.
Stump (wound) hematomas are controlled with wound drainage devices to minimize
infection.
Rehabilitation
Patients who require
amputation because of severe trauma are usu-ally, but not always, young and
healthy, heal rapidly, and partici-pate in a vigorous rehabilitation program.
Because the amputation is the result of an injury, the patient needs
psychological support in accepting the sudden change in body image and in
dealing with the stresses of hospitalization, long-term rehabilitation, and
mod-ification of lifestyle. Patients who undergo amputation need sup-port as
they grieve the loss, and they need time to work through their feelings about
their permanent loss and change in body image. Their reactions are
unpredictable and can include anger, bitterness, and hostility.
The multidisciplinary rehabilitation team (patient,
nurse, phy-sician, social worker, psychologist, prosthetist, vocational
rehabil-itation worker) helps the patient achieve the highest possible level of
function and participation in life activities (Fig. 69-17). Pros-thetic clinics
and amputee support groups facilitate this rehabi-litation process. Vocational
counseling and job retraining may be necessary to help patients return to work.
Psychological problems (eg, denial, withdrawal) may be in-fluenced by the type of support the patient receives from the re-habilitation team and by how quickly ADLs and use of the prosthesis are learned. Knowing the full options and capabilities available with the various prosthetic devices can give the patient a sense of control over the disability.
Related Topics