Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Trauma
Femur - Fracture
FEMUR
There is a high incidence of hip fracture among elderly people, who have brittle bones from osteoporosis (particularly women) and who tend to fall frequently. Weak quadriceps muscles, general frailty due to age, and conditions that produce decreased cerebral arterial perfusion (transient ischemic attacks, anemia, emboli, cardiovascular disease, effects of medications) contribute to the incidence of falls.
The patient who has sustained a hip frac-ture frequently
has a comorbidity (eg, cardiovascular, pulmonary, renal, endocrine). Often, a
fractured hip is a catastrophic event that will have a negative impact on the
patient’s lifestyle and qual-ity of life.
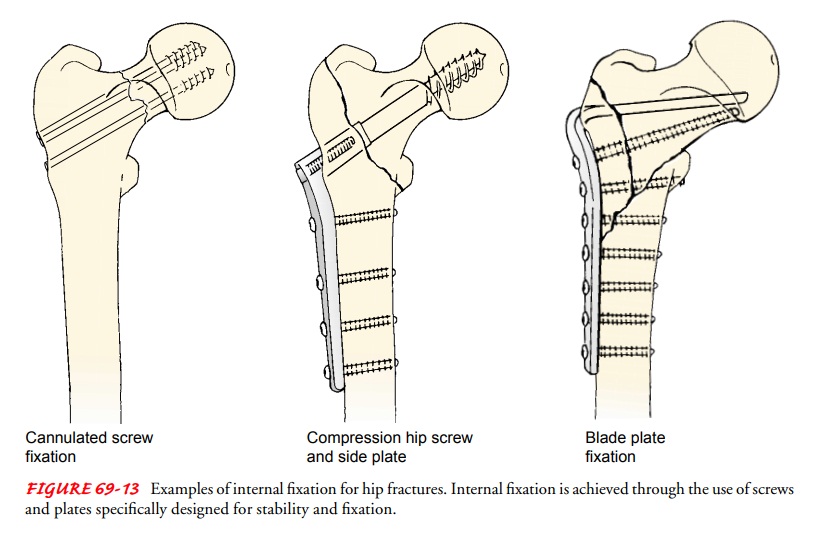
There are two major types of hip fracture. Intracapsular frac-tures are fractures
of the neck of the femur. Extracapsular
frac-tures are fractures of the trochanteric region (between the baseof the
neck and the lesser trochanter of the femur) and of the sub-trochanteric region
(Fig. 69-12). Fractures of the neck of the femur may damage the vascular system
that supplies blood to the head and the neck of the femur, and the bone may
die. For this reason, nonunion or aseptic necrosis is common in patients with
femoral neck fractures.
Extracapsular intertrochanteric fractures have an excellent blood supply and heal readily. However, extensive soft tissue damage may have occurred at the time of injury. It is not
uncommon for the fracture to be comminuted and unstable. There is a fairly high
mortality rate after intertrochanteric hip fractures, mainly because the
patients are usually elderly (70 to 85 years of age) and are poor surgical
candidates.
Clinical Manifestations
With fractures of the femoral neck, the leg is shortened,
ad-ducted, and externally rotated. The patient complains of pain in the hip and
groin or in the medial side of the knee. With most fractures of the femoral
neck, the patient is unable to move the leg without a significant increase in
pain. The patient is most comfortable with the leg slightly flexed in external
rotation. Im-pacted intracapsular femoral neck fractures cause moderate
dis-comfort (even with movement), may allow the patient to bear weight, and may
not demonstrate obvious shortening or rota-tional changes. With extracapsular
femoral fractures of the tro-chanteric or subtrochanteric regions, the
extremity is significantly shortened, externally rotated to a greater degree
than intra-capsular fractures, exhibits muscle spasm that resists positioning
of the extremity in a neutral position, and has an associated large hematoma or
area of ecchymosis. The diagnosis of fractured hip is confirmed with x-ray.
Gerontologic Considerations
Hip fractures are a frequent
contributor to death after the age of 75 years. Stress and immobility related
to the trauma predispose the older adult to pneumonia, sepsis, and reduced
ability to cope with other health problems.
Many elderly people
hospitalized with hip fracture are confused as a result of the stress of the
trauma, unfamiliar surroundings, sleep deprivation, medications, and systemic
illness. Preoperative predictors of postoperative delirium include age older
than 70 years, alcohol abuse, impaired cognitive status, poor functional
status, and markedly abnormal serum sodium, potassium, or glucose
con-centrations. In addition, confusion that develops in some elderly patients
may be caused by mild cerebral ischemia. Other factors associated with
confusion include responses to medications and anesthesia, malnutrition,
dehydration, infectious processes, mood disturbances, and blood loss.
To prevent
complications, the nurse must assess the elderly patient for chronic conditions
that require close monitoring. Examination of the legs may reveal edema due to
heart failure or peripheral pulselessness from arteriosclerotic vascular
dis-ease. Similarly, chronic respiratory problems may be present and may
contribute to the possible development of inadequate pulmonary ventilation.
Coughing and deep-breathing exercises are encouraged. Frequently, elderly
people are taking cardiac, antihypertensive, or respiratory medications that
need to be continued. The patient’s responses to these medications should be
monitored.
Dehydration and poor nutrition may be present. At times,
elderly people who live alone are unable to summon help at the time of injury.
A day or two may pass before assistance is provided, and as a result,
dehydration occurs. Dehydration contributes to hemoconcentration and
predisposes to thromboembolism. There-fore, the patient needs to be encouraged
to consume adequate flu-ids and a healthy diet.
Muscle weakness and
wasting may have contributed to the fall and fracture in the first place. Bed
rest and immobility will cause an additional loss of muscle strength unless the
nurse encourages the patient to move all joints except the involved hip and
knee. Patients are encouraged to use their arms and the overhead trapeze to
reposition themselves. This strengthens the arms and shoulders, which
facilitates walking with assistive devices.
Medical Management
Temporary skin traction,
Buck’s extension, may be applied to re-duce muscle spasm, to immobilize the
extremity, and to relieve pain. The findings of a recent study ( Jerre et al.,
2000) suggested that there is no benefit to the routine use of preoperative
skin traction for patients with hip fractures and that the use of skin traction
should be based on evaluation of the individual patient.
The goal of surgical
treatment of hip fractures is to obtain a sat-isfactory fixation so that the
patient can be mobilized quickly and avoid secondary medical complications.
Surgical treatment consists of (1) open or closed reduction of the fracture and
internal fixation,replacement of the femoral head with a prosthesis
(hemiarthro-plasty), or (3) closed reduction with percutaneous stabilization
for an intracapsular fracture. Surgical intervention is carried out as soon as
possible after injury. The preoperative objective is to ensure that the patient
is in as favorable a condition as possible for the sur-gery. Displaced femoral
neck fractures may be treated as emergen-cies, with reduction and internal
fixation performed within 12 to 24 hours after fracture. This minimizes the
effects of diminished blood supply and reduces the risk for avascular necrosis.
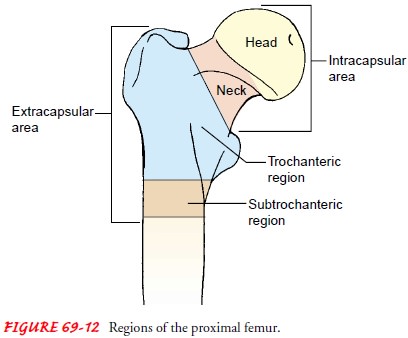
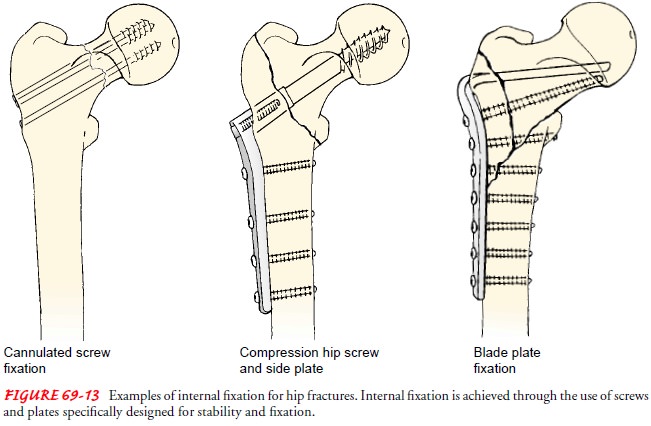
After general or spinal
anesthesia, the hip fracture is reduced under x-ray visualization using an
image intensifier. A stable fracture is usually fixed with nails, a
nail-and-plate combination, multiple pins, or compression screw devices (Fig.
69-13). The orthopedic surgeon determines the specific fixation device based on
the fracture site or sites. Adequate reduction is important for fracture
healing (the better the reduction, the better the healing).
Hemiarthroplasty (replacement of the head of the femur
with a prosthesis) is usually reserved for fractures that cannot be
satis-factorily reduced or securely nailed or to avoid complications of
nonunion and avascular necrosis of the head of the femur. Total hip replacement
may be used in selected patients with acetabular defects.
Postoperative Nursing Management
The immediate
postoperative care for a patient with a hip fracture is similar to that for
other patients undergoing major surgery. Attention is given to pain management,
preven-tion of secondary medical problems, and early mobilization of the
patient so that independent functioning can be restored.
During the first 24 to
48 hours, relief of pain and prevention of complications are priorities. The
nurse encourages deep breath-ing, coughing, and foot flexion exercises every 1
to 2 hours. Thigh-high elastic compression stockings and pneumatic compression
devices are used to prevent venous stasis. The nurse administers prescribed
intravenous prophylactic antibiotics and monitors the patient’s hydration,
nutritional status, and urine output. A pillow is placed between the legs to
maintain abduction and alignment and to provide needed support when turning the
patient.
REPOSITIONING THE PATIENT
The nurse may turn the patient onto the affected or unaffected extremity as prescribed by the physician. The standard method involves placing a pillow between the patient’s legs to keep the af-fected leg in an abducted position. The patient is then turned onto the side while proper alignment and supported abduction are maintained.
PROMOTING STRENGTHENING EXERCISE
The patient is
encouraged to exercise as much as possible by means of the overbed trapeze.
This device helps strengthen the arms and shoulders in preparation for
protected ambulation (eg, toe touch, partial weight bearing). On the first
postoperative day, the patient transfers to a chair with assistance and begins
assisted ambulation. The amount of weight bearing that can be permit-ted
depends on the stability of the fracture reduction. The physi-cian prescribes
the degree of weight bearing and the rate at which the patient can progress to
full weight bearing. Physical therapists work with the patient on transfers,
ambulation, and the safe use of a walker and crutches.
The patient who has experienced a fractured hip can
antici-pate discharge to home or to an extended care facility with the use of
an ambulatory aid. Some modifications in the home may be needed to permit safe
use of walkers and crutches and for the patient’s continuing care.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Elderly people with hip fractures are particularly prone
to compli-cations that may require more vigorous treatment than the fracture.
In some instances, shock proves fatal. Achievement of homeostasis after injury
and after surgery is accomplished through careful mon-itoring and collaborative
management, including adjustment of therapeutic interventions as indicated.
Neurovascular complications may occur from direct injury tonerves and blood vessels
or from increased tissue pressure. With hip fracture, bleeding into the tissues
is expected. Excessive swell-ing may be observed. Therefore, the nurse must
monitor the neuro-vascular status of the affected leg.
Deep vein thrombosis is
the most common complication. Toprevent DVT, the nurse encourages intake of
fluids and ankle and foot exercises. Elastic compression stockings, sequential
compres-sion devices, and prophylactic anticoagulant therapy may be
pre-scribed. The nurse assesses the patient’s legs at least every 4 hours for
signs of DVT.
Pulmonary complications are a threat to elderly patients under-going hip surgery.
Deep-breathing exercises, a change of position at least every 2 hours, and the
use of an incentive spirometer help to prevent respiratory complications. The
nurse assesses breath sounds at least every 4 to 8 hours to detect adventitious
or dimin-ished sounds.
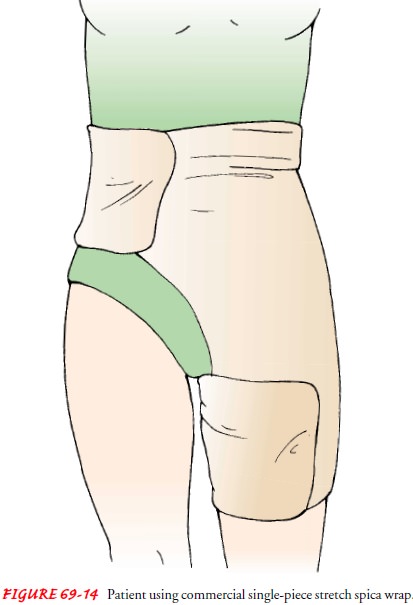
Skin breakdown is often seen in elderly patients with hip frac-ture.
Blisters caused by tape are related to the tension of soft tis-sue edema under
the nonelastic tape. An elastic hip spica wrap dressing (Fig. 69-14) or elastic
tape applied in a vertical fashion may reduce the incidence of tape blisters.
In addition, patients with hip fractures tend to remain in one position and may
develop pressure ulcers. Proper skin
care, especially on the heels, back, sacrum,and shoulders, helps to relieve
pressure. High-density foam, sta-tic air, or another type of special mattress
may provide protection by distributing pressure more evenly.
Loss of bladder control (incontinence) may occur. In general,the routine use of
an indwelling catheter is avoided because of the high risk for urinary tract
infection. If a catheter is inserted at the time of surgery, it usually is
removed on the morning of the first postoperative day. Because urinary
retention is common after sur-gery, the nurse must assess the patient’s voiding
patterns. To en-sure proper urinary tract function, the nurse encourages
liberal fluid intake within the cardiovascular tolerance of the patient.
Delayed complications of hip fractures include infection, non-union, avascular necrosis of the femoral head (particularly with femoral neck fractures), and fixation device problems (eg, pro-trusion of the fixation device through the acetabulum, loosening of hardware). Infection is suspected if the patient complains of per-sistent, moderate discomfort in the hip and has a mildly elevated sedimentation rate. The nursing management of the elderly patient with a hip fracture is summarized in the Plan of Nursing Care.
HEALTH PROMOTION
Osteoporosis screening
of patients who have experienced hip frac-ture is important for prevention of
future fractures. With dual-energy x-ray absorptiometry (DEXA) scan screening,
the actual risk for additional fracture can be determined. Specific patient
education regarding dietary requirements, lifestyle changes, and exercise to
promote bone health is needed. Specific therapeutic in-terventions need to be
initiated to retard additional bone loss and to build bone mineral density.
Studies have shown that health care providers caring for patients with hip
fractures fail to diagnose or treat these patients for osteoporosis despite the
high probability that hip fractures are secondary to osteoporosis (Kamel, et
al., 2000). Fall prevention is also important and may be achieved through
exercises to improve muscle tone and balance and through the elimination of
environmental hazards. In addition, the use of hip protectors that absorb or
shunt impact forces may help to pre-vent an additional hip fracture if the
patient were to fall.
Related Topics