Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Trauma
Fractures
Fractures
A fracture is
a break in the continuity of bone and is defined ac-cording to its type and
extent. Fractures occur when the bone is subjected to stress greater than it
can absorb. Fractures are caused by direct blows, crushing forces, sudden
twisting motions, and even extreme muscle contractions. When the bone is
broken, ad-jacent structures are also affected, resulting in soft tissue edema,
hemorrhage into the muscles and joints, joint dislocations, rup-tured tendons,
severed nerves, and damaged blood vessels. Body organs may be injured by the
force that caused the fracture or by the fracture fragments.
Types of Fractures
A complete fracture involves a break across the entire cross-section
of the bone and is frequently displaced (removed from normal position). In an incomplete fracture (eg, greenstick
fracture), the break occurs through only part of the cross-section of the bone.
A comminuted fracture is one that
produces several bone frag-ments. A closed
fracture (simple fracture) is one that does not cause a break in the skin.
An open fracture (compound, or
complex,fracture) is one in which the skin or mucous membrane wound extends to
the fractured bone. Open fractures are graded accord-ing to the following
criteria:
·
Grade I is a clean wound less
than 1 cm long.
·
Grade II is a larger wound
without extensive soft tissue damage.
·
Grade III is highly
contaminated, has extensive soft tissue damage, and is the most severe.
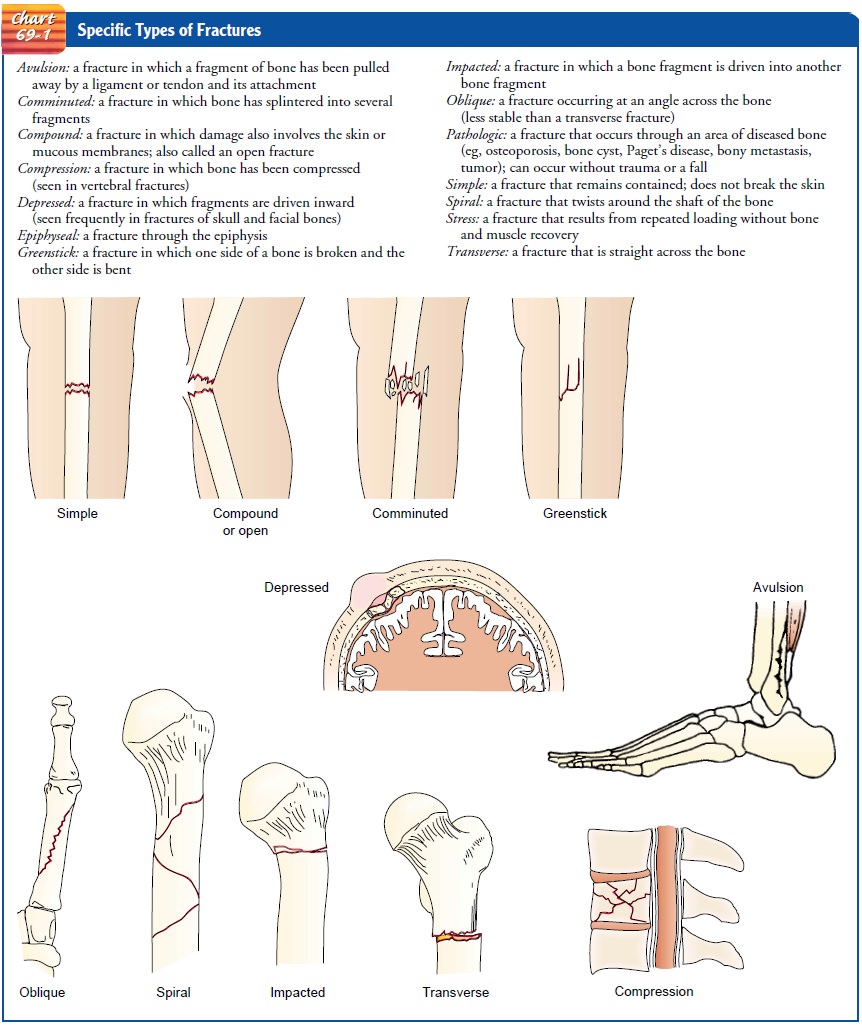
Fractures may also be described according to the anatomic
placement of fragments, particularly if they are displaced or nondisplaced.
Specific types of fractures are highlighted in Chart 69-1.
Clinical Manifestations
The clinical manifestations of a fracture are pain, loss
of function, deformity, shortening of the extremity, crepitus, and local
swell-ing and discoloration. Not all of these clinical manifestations are
present in every fracture. For example, many are not present with linear or
fissure fractures or with impacted fractures. The diagnosis of a fracture is
based on the patient’s symptoms, the physical signs, and the x-ray findings.
Usually, the patient reports having sus-tained an injury to the area.
PAIN
The pain is continuous and increases in severity until
the bone fragments are immobilized. The muscle spasm that accompanies fracture
is a type of natural splinting designed to minimize further movement of the
fracture fragments.
LOSS OF FUNCTION
After a fracture, the extremity cannot function properly,
because normal function of the muscles depends on the integrity of the bones to
which they are attached. Pain contributes to the loss of function. In addition,
abnormal movement (false motion) may be present.
DEFORMITY
Displacement,
angulation, or rotation of the fragments in a frac-ture of the arm or leg
causes a deformity (either visible or palpable) that is detectable when the
limb is compared with the uninjured extremity. Deformity also results from soft
tissue swelling.
SHORTENING
In fractures of long bones, there is actual shortening of
the ex-tremity because of the contraction of the muscles that are attached
above and below the site of the fracture. The fragments often over-lap by as
much as 2.5 to 5 cm (1 to 2 inches).
CREPITUS
When the extremity is examined with the hands, a grating
sensa-tion, called crepitus, can be
felt. It is caused by the rubbing of the bone fragments against each other.
SWELLING AND DISCOLORATION
Localized swelling and
discoloration of the skin (ecchymosis) oc-curs after a fracture as a result of
trauma and bleeding into the tis-sues. These signs may not develop for several
hours after the injury.
Emergency Management of Fractures
Immediately after
injury, whenever a fracture is suspected, it is im-portant to immobilize the
body part before the patient is moved. If an injured patient must be removed
from a vehicle before splints can be applied, the extremity is supported above
and below the fracture site to prevent rotation as well as angular motion.
Adequate splinting,
including joints adjacent to the fracture, is essential. Movement of fracture
fragments causes additional pain, soft tissue damage, and bleeding. Temporary,
well-padded splints, firmly bandaged over clothing, serve to immobilize the
fracture. Immobilization of the long bones of the lower extremi-ties may be
accomplished by bandaging the legs together, with the unaffected extremity
serving as a splint for the injured one. In an upper extremity injury, the arm
may be bandaged to the chest, or an injured forearm may be placed in a sling.
The neurovascular status distal to the injury should be assessed to determine
ade-quacy of peripheral tissue perfusion and nerve function.
With an open fracture, the wound is covered with
a clean (sterile) dressing to prevent contamination of deeper tissues. No
attempt is made to reduce the fracture, even if one of the bone fragments is
protruding through the wound. Splints are applied for immobilization.
In the emergency
department, the patient is evaluated com-pletely. The clothes are gently
removed, first from the uninjured side of the body and then from the injured
side. The patient’s clothing may be cut away. The fractured extremity is moved
as little as possible to avoid more damage.
Medical Management of Fractures
The principles of fracture treatment include reduction,
immobi-lization, and regaining of normal function and strength through
rehabilitation.
REDUCTION
Reduction of a fracture (“setting” the bone) refers to
restoration of the fracture fragments to anatomic alignment and rotation.
Either closed reduction or open reduction may be used to reduce a frac-ture.
The specific method selected depends on the nature of the fracture; however,
the underlying principles are the same. Usually, the physician reduces a
fracture as soon as possible to prevent loss of elasticity from the tissues
through infiltration by edema or hemorrhage. In most cases, fracture reduction becomes more difficult
as the injury begins healing.
Before fracture reduction and immobilization, the patient
is prepared for the procedure; permission for the procedure is ob-tained, and
an analgesic is administered as prescribed. Anesthesia may be administered. The
injured extremity must be handled gen-tly to avoid additional damage.
Closed Reduction.
In most instances, closed reduction is
accom-plished by bringing the bone fragments into apposition (ie, placing the
ends in contact) through manipulation and manual traction. The extremity is
held in the desired position while the physician applies a cast, splint, or
other device. Reduction under anesthesia with percutaneous pinning may be used.
The immobilizing device maintains the reduction and stabilizes the extremity for
bone heal-ing. X-rays are obtained to verify that the bone fragments are
cor-rectly aligned.
Traction (skin or skeletal) may be used to effect fracture reduc-tion and immobilization. Traction may be used until the patient is physiologically stable and able to withstand surgical fixation.
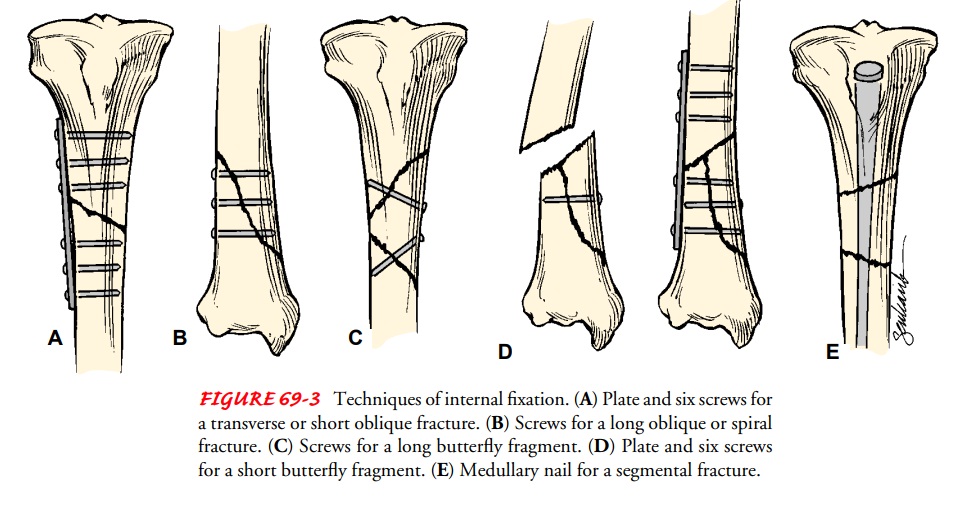
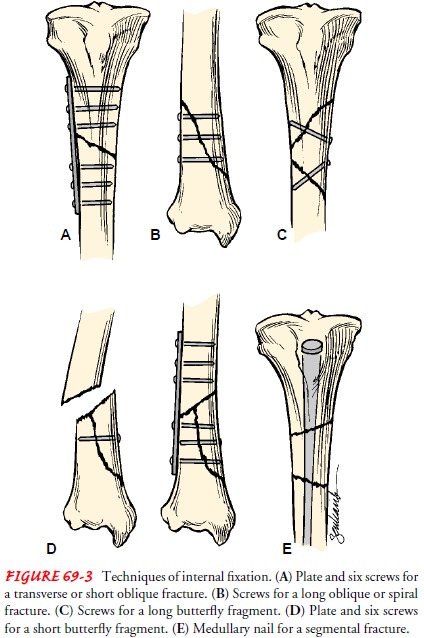
Open Reduction.
Some fractures require
open reduction. Througha surgical approach, the fracture fragments are reduced.
Internal fix-ation devices (metallic pins, wires, screws, plates, nails, or
rods) may be used to hold the bone fragments in position until solid bone
healing occurs. These devices may be attached to the sides of bone, or they may
be inserted through the bony fragments or directly into the medullary cavity of
the bone (Fig. 63-3). Internal fixation de-vices ensure firm approximation and
fixation of the bony fragments.
IMMOBILIZATION
After the fracture has been reduced, the bone fragments must be immobilized, or held in correct position and alignment, until union occurs. Immobilization may be accomplished by external or internal fixation. Methods of external fixation include bandages, casts, splints, continuous traction, and external fixators. Metal implants used for internal fixation serve as internal splints to immobilize the fracture.
MAINTAINING AND RESTORING FUNCTION
Reduction and
immobilization are maintained as prescribed to pro-mote bone and soft tissue
healing. Swelling is controlled by elevat-ing the injured extremity and
applying ice as prescribed. Neuro-vascular status (circulation, movement,
sensation) is monitored, and the orthopedic surgeon is notified immediately if
signs of neurovascular compromise are identified. Restlessness, anxiety, and
discomfort are controlled with a variety of approaches, such as re-assurance,
position changes, and pain relief strategies, including use of analgesics.
Isometric and muscle-setting exercises are encouraged to minimize disuse
atrophy and to promote circulation. Participa-tion in activities of daily
living (ADLs) is encouraged to promote independent functioning and self-esteem.
Gradual resumption of activities is promoted within the therapeutic
prescription. With in-ternal fixation, the surgeon determines the amount of
movement and weight-bearing stress the extremity can withstand and pre-scribes
the level of activity.
Nursing Management
PATIENTS WITH CLOSED FRACTURES
The nurse encourages
patients with closed (simple) fractures to re-turn to their usual activities as
rapidly as possible. The nurse teaches patients how to control swelling and
pain associated with the frac-ture and with soft tissue trauma and encourages
them to be active within the limits of the fracture immobilization (Chart
69-2).
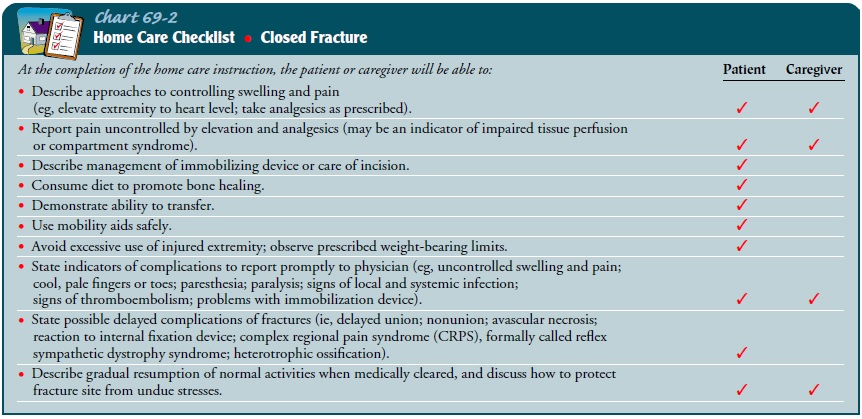
It is important to teach exercises to maintain the health of unaffected muscles and to increase
the strength of muscles needed for trans-ferring and for using assistive
devices (eg, crutches, walker, special utensils). The nurse and physical
therapist teach patients how to use assistive devices safely. Plans are made to
help patients modify their home environment as needed and to secure personal
assis-tance if necessary. Patient teaching includes self-care, medication
information, monitoring for potential complications, and the need for
continuing health care supervision. Fracture healing and restoration of full
strength and mobility may take months.
PATIENTS WITH OPEN FRACTURES
In an open fracture, there is risk of osteomyelitis,
tetanus, and gas gangrene. The objectives of management are to prevent
infection of the wound, soft tissue, and bone and to promote healing of soft
tissue and bone. The nurse administers tetanus prophylaxis if in-dicated.
Serial irrigation and débridement are used to remove anaerobic organisms. Intravenous
antibiotics are prescribed to pre-vent or treat infection.
Prompt, thorough wound irrigation and débridement in the
operating room are necessary. The wound is cultured. Devitalized bone fragments
are removed. The fracture is carefully reduced and stabilized by external
fixation or intramedullary nails. Any
damage to blood vessels, soft tissue, muscles, nerves, and tendons is treated.
With open fractures,
primary wound closure is usually delayed. Heavily contaminated wounds are left
unsutured and dressed with sterile gauze to permit swelling and wound drainage.
Wound irri-gation and débridement may be repeated, removing infected and
devitalized tissue and increasing vascularity in the region. After it has been
determined that infection is not present, the wound is closed in 5 to 7 days,
and all dead space is obliterated by grafting of autogenous skin or a flap.
The nurse elevates the
extremity to minimize edema. It is im-portant to assess neurovascular status
frequently. The nurse mea-sures the patient’s temperature at regular intervals
and monitors the patient for signs of infection. In 4 to 8 weeks, bone grafting
may be necessary to bridge bone defects and to stimulate bone healing.
Related Topics