Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Trauma
Sports-Related Injuries
Sports-Related
Injuries
Many people participate
in recreational sports. These recreational athletes may push themselves beyond
the level of their physical conditioning and incur injuries. Injuries to the
musculoskeletal system may be acute (eg, sprains, strains, dislocations, fractures),
or they may be gradual, resulting from overuse (eg, chondroma-lacia patella,
tendinitis, stress fractures). Professional athletes are also susceptible to
injury, even though their training is supervised closely to minimize the
occurrence of injury.
·
Contusions result from direct
falls or blows. The initial dull pain becomes greater, with edema and stiffness
occurring by the next day.
·
Sprains commonly occur in
fingers, ankles, and knees. If the ligament damage is major, the joint becomes
unstable, and surgical repair may be required. In addition, an avulsion
frac-ture may exist.
·
Strains manifest with a sharp,
stabbing pain caused by bleed-ing and immediate protective muscle contraction.
Tennis players often suffer calf muscle strains; soccer players often
experience quadriceps strains; and swimmers, weight lifters, and tennis players
often suffer shoulder strains.
·
Tendinitis
(inflammation of a tendon) is caused by overuseand is
seen in tennis players (epicondylar tendinitis, or “ten-nis elbow”), in runners
and gymnasts (Achilles tendinitis), and in basketball players (infrapatellar
tendinitis).
·
Meniscal injuries of the knee
occur with excessive rotational stress.
·
Dislocations are seen with
sports that involve throwing or lifting.
·
Fractures occur with falls.
Skaters and bikers frequently suffer Colles’ fractures of the wrist when they
fall on out-stretched arms; ballet dancers and track and field athletes may
experience metatarsal fractures. Stress fractures occur with repeated bone
trauma from activities such as jogging, gymnastics, basketball, and aerobics.
The tibias, fibulas, and metatarsals are most vulnerable.
Patients who have
experienced a sports-related injury are of-ten highly motivated to return to
their previous level of activity. Compliance with restriction of activities and
gradual resumption of activities may be a significant problem for these
patients. They need to be taught how to avoid further injury or new injury.
With recurrence of symptoms, they need to diminish their level and in-tensity
of activity to a comfortable level and to treat the symptoms with RICE. The
time required to recover from a sports-related injury can be as short as a few
days or longer than 6 weeks.
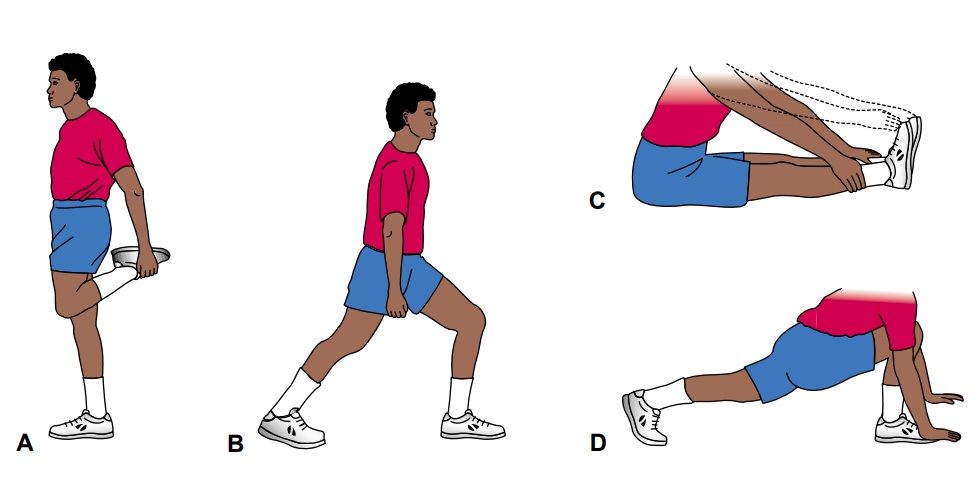
Prevention
Sports-related injuries
can be prevented by the use of proper equip-ment (eg, running shoes for
joggers, wrist guards for skaters) and by effectively training and conditioning
of the body. Specific training needs to be tailored to the person and the
sport. Warm-up routines generally include walking or slow jogging for about 5
minutes, fol-lowed by slow, gradual stretching. The athlete holds the stretch
for 10 seconds before relaxing and repeating the stretch (Fig. 69-1). Preparing
the body for sport activities increases the person’s flexi-bility and decreases
the incidence of strains and sprains.
After exercise, the body needs to cool off to prevent cardiovas-cular problems such as hypotension, syncope, and dysrhythmias. Changes in activities and stresses should occur gradually. In addi-tion, the athlete needs to be taught to “tune in” to body symptoms that indicate stress and to modify activities to minimize injury and to promote healing.
ROTATOR CUFF TEARS
Rotator cuff tears
may result from an acute injury or fromchronic joint stresses. Patients
complain of pain, limited ROM, and some joint dysfunction, including muscle
weakness. In many cases, the patient with a rotator cuff tear experiences night
pain and is unable to sleep on the involved side. The patient is un-able to perform
over-the-head activities. The acromioclavicu-lar joint is tender. X-rays are
helpful in evaluating the joint. Arthrography and magnetic resonance imaging
(MRI) are used to determine soft tissue pathology and the extent of the rotator
cuff tear.
Medical Management
Initial conservative management includes use of
nonsteroidal anti-inflammatory drugs (NSAIDs) including cyclooxygenase-2
(COX-2) inhibitors, rest with modification of activities, injec-tion of a
corticosteroid into the shoulder joint, and progressive stretching, ROM, and
strengthening exercises. Some rotator cuff tears require arthroscopic débridement (removal of devi-talized
tissue) or arthroscopic or open acromioplasty with ten-don repair.
Postoperatively, the shoulder is immobilized for several days to 4 weeks.
Physical therapy with shoulder exercises is begun as prescribed, and the
patient is instructed in how to perform the exercises at home. Full recovery is
expected in 6 to 12 months.
EPICONDYLITIS (TENNIS ELBOW)
Epicondylitis is a
chronic, painful condition that is caused by ex-cessive, repetitive extension,
flexion, pronation, and supination activities of the forearm. These excessive,
repetitious activities re-sult in inflammation (tendinitis) and minor tears in
the tendons at the origin of the muscles on the medial or lateral
epicondyles.Activities contributing to the development of epicondylitis
in-clude tennis, racket sports, pitching, gymnastics, and repetitive use of a
screwdriver. The pain characteristically radiates down the extensor (dorsal)
surface of the forearm. The patient may have a weakened grasp. Most often,
relief is obtained by rest and avoid-ance of the aggravating activity.
Medical Management
Application of ice after the activity and administration
of NSAIDs, including COX-2 inhibitors, usually relieve the pain. In some
in-stances, the arm is immobilized in a molded splint or cast. Because of its
degenerative effects on tendons, local injection of a cortico-steroid is
reserved for patients with severe pain who do not respond to NSAIDs and
immobilization. After pain subsides, rehabilita-tion exercises include gentle
and gradually increased stretching of the tendons. A tennis elbow counterforce
strap to limit extension of the elbow may be prescribed when activity is
resumed. Occa-sionally, surgery may be needed to release strictures or to
débride the joint.
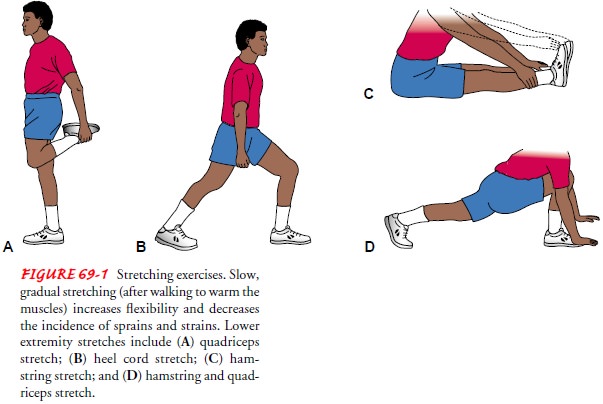
LATERAL AND MEDIAL COLLATERAL LIGAMENT INJURY
Lateral and medial collateral ligaments of the knee (Fig.
69-2) provide stability at the sides of the knee. Injury to these liga-ments
occurs when the foot is firmly planted and the knee is struck—either medially,
causing stretching and tearing injury to the lateral collateral ligament, or
laterally, causing stretching and tearing injury to the medial collateral
ligament. The patient experiences pain, joint instability, and inability to
walk without assistance.
Medical Management.
Emergency management
includes RICE. The joint is evaluated for fracture. Hemarthrosis (bleeding into
the joint) may develop, contributing to the pain. The joint fluid is aspirated
to relieve pressure.
The treatment depends on the severity of the sprain.
Conser-vative management includes limited weight bearing and use of protective
elastic bandaging or a brace. As pain subsides, ROM exercise is encouraged. The
patient’s return to full activities, in-cluding sports, depends on return of
motion, functional stability of the joint, and muscle strength.
If needed, surgical reconstruction may be performed immedi-ately or delayed. Generally, the leg is immobilized, and weight bearing is restricted for 6 to 8 weeks. A progressive rehabilitation program helps to restore the function and strength of the knee. Rehabilitation requires many months, and the patient may need to wear a derotational brace while engaging in sports.
Nursing Management
The nurse provides
patient teaching about proper use of ambula-tory devices, the healing process,
and activity limitation to promote healing. The nurse teaches the surgical
patient about pain man-agement, medications (analgesics, antibiotics), brace
use, wound care, possible complications (eg, altered neurovascular status,
infec-tion, skin breakdown), and self-care.
ANTERIOR AND POSTERIOR CRUCIATE LIGAMENT INJURY
The anterior cruciate
ligament (ACL) and the posterior cruciate ligament (PCL) of the knee stabilize
forward and backward mo-tion of the femur and tibia (see Fig. 69-2). These
ligaments cross in the center of the knee. Injury occurs when the foot is
firmly planted, the knee is hyperextended, and the person twists the torso and
femur. The patient reports a pop or tearing sensation with this twisting
injury. Usually, the ACL is torn. The patient expe-riences pain, joint
instability, and pain with ambulation.
Medical Management
Emergency management
includes RICE. The joint is evaluated for fracture. Joint effusion and
hemarthrosis require joint aspira-tion and wrapping with a compression elastic
dressing.
Treatment depends on the
severity of the injury and the effect of the injury on daily activities.
Conservative treatment involves application of a brace, physical therapy, and
avoidance of jump-ing activities. Surgical ACL reconstruction includes tendon
repair with grafting and is performed as ambulatory arthroscopic sur-gery.
After surgery, the patient is taught to control pain with oral opioid
analgesics, NSAIDs, COX-2 inhibitors, and cryotherapy (a cooling pad
incorporated in a dressing). The patient is taught about monitoring
neurovascular status of the leg, wound care, and signs of complications that
need to be reported promptly to the surgeon. Exercises (ankle pumps, quadriceps
sets, and ham-string sets) are encouraged during the early postoperative
period. The nurse reinforces instruction about weight-bearing limits, ex-ercise
restrictions, and the use of a knee brace or immobilizer. The patient must
protect the graft by complying with exercise restric-tions. The physical
therapist supervises progressive ROM and weight bearing (as the patient is
permitted). Continuous passive motion may be helpful in restoring full ROM.
Rehabilitation after surgery typically takes 6 to 12 months.
MENISCAL INJURIES
In the knee, there are
two crescent-shaped (semilunar) cartilages, called menisci, attached to the
edge of the shallow articulating sur-face of the head of the tibia (see Fig.
69-2). Each meniscus moves slightly
backward and forward to accommodate the condyles of the femur when the leg is
flexed or extended. Normally, little twist-ing movement is permitted in the
knee joint. In sports or acci-dents, twisting of the knee or repetitive
squatting and impact may result in either tearing or detachment of the
cartilage from its attachment to the head of the tibia.
These injuries leave
loose cartilage in the knee joint that may slip between the femur and the
tibia, preventing full extension of the leg. If this happens during walking or
running, patients often describe their leg as “giving way” under them. Patients
may hear or feel a click in the knee when they walk, especially when they
extend the leg that is bearing weight, as in going upstairs. When the cartilage
is attached to the front and back of the knee but torn loose laterally
(bucket-handle tear), it may slide between the bones to lie between the
condyles and prevent full flexion or extension. As a result, the knee “locks.”
Meniscal injuries produce pain and disability because the patient never knows
when the knee will mal-function. Also, the torn cartilage is an irritant in the
joint, causing inflammation, chronic synovitis, and effusion.
Medical Management
Initial conservative
treatment includes immobilization of the knee, use of crutches,
antiinflammatory agents, analgesics, and modification of activities to avoid
those causing the symptoms. If symptoms persist, the damaged cartilage is
surgically removed (meniscectomy) through a procedure in which the surgeon uses
an arthroscope to visualize and
repair the damage. After surgery, apressure dressing is applied, and a
knee-immobilizing splint may be required. The most common complication is an
effusion into the knee joint, which produces marked pain. The physician may
need to aspirate the joint to remove fluid and relieve the pressure. These
patients are taught quadriceps-setting and ROM exercises. Additional exercises
help to restore full function, stability, and strength. After arthroscopic
meniscectomy, most patients resume activities in a day or two, and sports can
be resumed in several weeks, as prescribed by the physician.
RUPTURE OF THE ACHILLES TENDON
Traumatic rupture of the
Achilles tendon, generally within the tendon sheath, occurs during activities
when there is a sudden contraction of the calf muscle with the foot fixed
firmly to the floor or ground. The patient experiences sharp pain and is unable
to plantar flex the foot. Immediate surgical repair of complete Achilles tendon
ruptures is usually recommended to obtain satisfactory re-sults. After surgery,
a cast or brace is used to immobilize the joint. In some situations,
conservative management with a plantar-flexed cast for 6 to 8 weeks may be
used. After immobilization, a heel lift is worn and progressive physical
therapy to promote ankle ROM and strength is begun.
Related Topics