Chapter: Medical Surgical Nursing: Management of Patients With Burn Injury
Nursing Process: Care of the Patient During the Rehabilitation Phase
NURSING PROCESS: CARE OF THE PATIENT DURING THE
REHABILITATION PHASE
Assessment
Information about the patient’s educational level,
occupation, leisure activities, cultural background, religion, and family
inter-actions is obtained early. The patient’s self-concept, mental sta-tus,
emotional response to the injury and hospitalization, level of intellectual
functioning, previous hospitalizations, response to pain and pain relief
measures, and sleep pattern are also essential components of a comprehensive
assessment. Information about the patient’s general self-concept, self-esteem,
and coping strate-gies in the past will be valuable in addressing emotional
needs.
Ongoing
physical assessments related to rehabilitation goals include range of motion of
affected joints, functional abilities in activities of daily living, early
signs of skin breakdown from splints or positioning devices, evidence of
neuropathies (neuro-logic damage), activity tolerance, and quality or condition
of healing skin. The patient’s participation in care and ability to demonstrate
self-care in such areas as ambulation, eating, wound cleaning, and applying
pressure wraps are documented on a reg-ular basis. In addition to these
assessment parameters, specific complications and treatments require additional
specific assess-ments; for example, the patient undergoing primary excision
re-quires postoperative assessment.
Recovery
from burn injury involves every system of the body. Therefore, assessment of
the burn patient must be comprehen-sive and continuous. Priorities will vary at
different points dur-ing the rehabilitation phase. Understanding the
pathophysiologic responses to burn injury forms the framework for detecting
early progress or signs and symptoms of complications. Early detection leads to
early intervention and enhances the potential for suc-cessful rehabilitation.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, priority nursing
diagnoses in the long-term rehabilitation phase of burn care may include the
following:
·
Activity intolerance related
to pain on exercise, limited joint mobility, muscle wasting, and limited
endurance
·
Disturbed body image related
to altered physical appearance and self-concept
·
Deficient knowledge about
postdischarge home care and follow-up needs
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on the assessment data, potential complications that may develop in the
rehabilitation phase include:
·
Contractures
·
Inadequate psychological
adaptation to burn injury
Planning and Goals
The
major goals for the patient include increased participation in activities of
daily living; increased understanding of the injury, treatment, and planned
follow-up care; adaptation and adjust-ment to alterations in body image,
self-concept, and lifestyle; and absence of complications.
Nursing Interventions
PROMOTING ACTIVITY TOLERANCE
Nursing interventions that must be carried out
according to a strict regimen and the pain that accompanies movement take their
toll on a burn patient. The patient may become confused and dis-oriented and
lack the energy to participate optimally in care. The nurse must schedule care
in such a way that the patient has periods of uninterrupted sleep. A good time
for planned patient rest is after the stress of dressing changes and exercise,
while pain interventions and sedatives may still be effective. This plan must
be communi-cated to family members and other care providers.
Burn patients may have insomnia related to frequent
night-mares about the burn injury or to other fears and anxieties about the
outcome of the injury. The nurse listens to and reassures the patient and
administers hypnotic agents, as prescribed, to pro-mote sleep.
Reducing
metabolic stress by relieving pain, preventing chill-ing or fever, and
promoting the physical integrity of all body sys-tems will help the patient
conserve energy for therapeutic activities and wound healing.
The
nurse incorporates physical therapy exercises in the pa-tient’s care to prevent
muscle atrophy and to maintain the mo-bility required for daily activities. The
patient’s activity tolerance, strength, and endurance will gradually increase
if activity occurs over increasingly longer periods. Fatigue, fever, and pain
toler-ance are monitored and used to determine the amount of activ-ity to be
encouraged on a daily basis. Activities such as family visits and recreational
or play therapy (eg, video games, radio, TV) can provide diversion, improve the
patient’s outlook, and increase tolerance for physical activity.
IMPROVING BODY IMAGE AND SELF-CONCEPT
Burn
patients frequently suffer profound losses. These include not only a loss of
body image due to disfigurement but also losses of personal property, homes,
loved ones, and ability to work. They lack the benefit of anticipatory grief
often seen in a patient approaching surgery or a person dealing with the
terminal illness of a loved one.
As care progresses, the patient who is recovering
from burns be-comes aware of daily improvement and begins to exhibit basic
con-cerns: Will I be disfigured? How long will I be in the hospital? What about
my job and family? Will I ever be independent again? How can I pay for my care?
Was my burn the result of my care-lessness? As the patient expresses such
concerns, the nurse must take time to listen and to provide realistic support.
The nurse can refer patients to a support group, such as those usually
available at re-gional burn centers or through organizations such as the
Phoenix Society. Through participation in such groups, patients will meet
others with similar experiences and learn coping strategies to help them deal
with their losses. Interaction with other burn survivors allows the patient to
see that adaptation to the burn injury is pos-sible. If a support group is not
available, visits from burn survivors can be helpful to the patient coping with
such a traumatic injury.
A
major responsibility of the nurse is to assess constantly the patient’s
psychosocial reactions. What are the patient’s fears and concerns? Does the
patient fear loss of control of care, indepen-dence, or sanity itself? Is the
patient afraid of rejection by family and loved ones? Does he or she fear being
unable to cope with pain or physical appearance? Does the patient have concerns
about sexuality, including sexual function? Being aware of these anxieties and
understanding the basis of the patient’s fears enable the nurse to provide
support and to cooperate with other members of the health care team in developing
a plan to help the patient deal with these feelings.
When
caring for burn patients, the nurse needs to be aware that there are prejudices
and misunderstandings in society about those who are viewed as different.
Opportunities and accommodations available to others are often denied those who
are disfigured. Such amenities include social participation, employment,
prestige, var-ious roles, and status. The health care team must actively
promote a healthy body image and self-concept in burn survivors so that they
can accept or challenge others’ perceptions of those who are disfigured.
Survivors themselves must show others who they are, how they function, and how
they want to be treated.
The
nurse can help patients practice their responses to people who may stare or
inquire about their injury once they are dis-charged from the hospital. The nurse can help
patients build selfesteem by recognizing their uniqueness—for example, with
small gestures such as providing a birthday cake, combing the patient’s hair before
visiting hours, giving information about the avail-ability of a cosmetician to
enhance appearance, and teaching the patient ways to direct attention away from
a disfigured body to the self within. Consultants such as psychologists, social
workers, vocational counselors, and teachers are valuable participants in
assisting burn patients to regain their self-esteem.
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
Contractures
With
early and aggressive physical and occupational therapy, contractures are rarely
a long-term complication. However, sur-gical intervention is indicated if a
full range of motion in the burn patient is not achieved.
Impaired Psychological Adaptation to the Burn Injury
Some patients, particularly those with limited
coping skills or psychological function or a history of psychiatric problems
before the burn injury, may not achieve adequate psychological adapta-tion to
the burn injury. Psychological counseling or psychiatric referral may be made
to assess the patient’s emotional status, to help the patient develop coping
skills, and to intervene if major psychological issues or ineffective coping is
identified.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
As the inpatient phase of recovery becomes shorter,
the focus of re-habilitative interventions is directed toward outpatient care
or care in a rehabilitation center. In the long term, much of the care of
healing burns will be performed by the patient and others at home. Throughout
the phases of burn care, efforts are made to prepare the patient and family for
the care that will continue at home. Thus, they are instructed about the
measures and procedures that they will need to perform. For example, patients
commonly have small areas of clean, open wounds that are healing slowly. They
are in-structed to wash these areas daily with mild soap and water and to apply
the prescribed topical agent or dressing.
In addition to instructions about wound care,
patients and families require careful written and verbal instructions about
pre-vention of complications, pain management, and nutrition. In-formation
about specific exercises and use of pressure garments and splints is reviewed
with both the patient and family; written instructions are provided for
reference. They are taught to recog-nize abnormal signs and instructed to
report them to the physi-cian. All of this information will enable patients to
progress successfully through the rehabilitative phase of burn manage-ment. The
patient and family are assisted in planning for the pa-tient’s continued care
by identifying and acquiring supplies and equipment that are needed at home
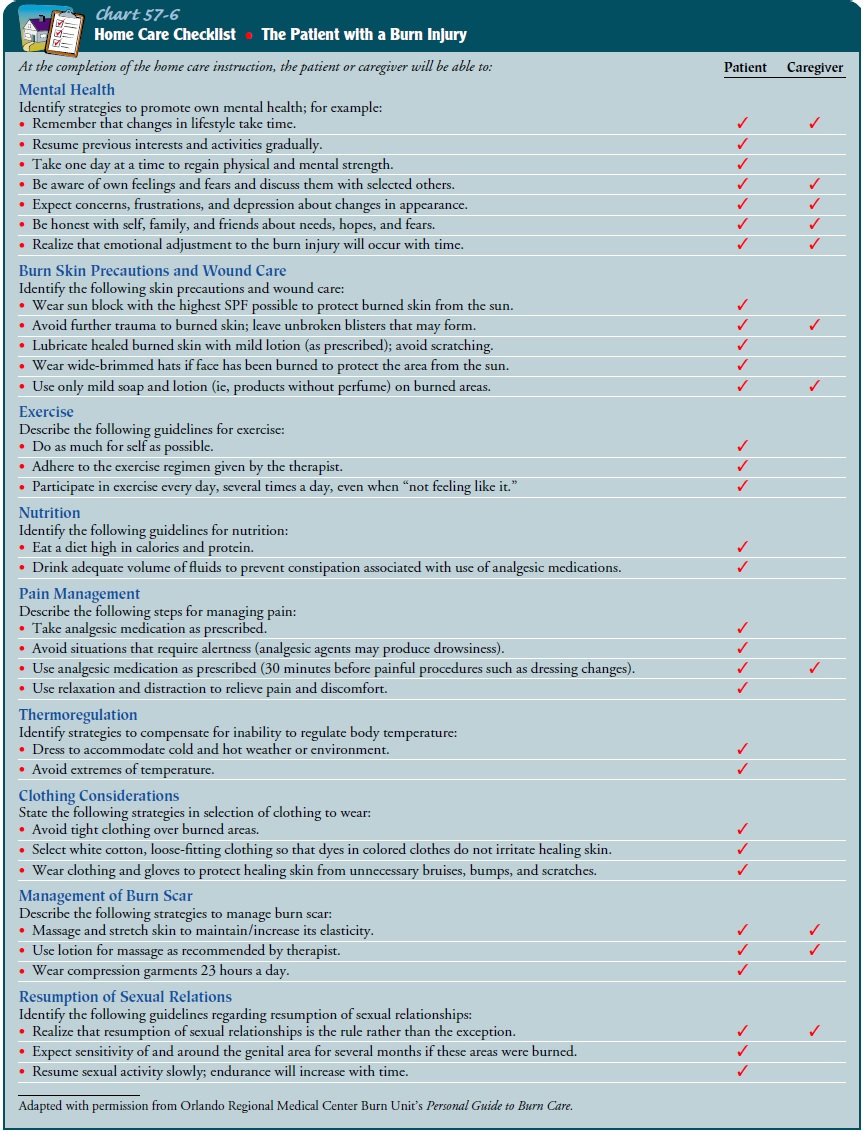
(Chart 57-6).
Continuing Care
Follow-up care by an interdisciplinary burn care team will be nec-essary. Preparations should begin during the early stages of care. Patients who receive care in a burn center usually return to the burn clinic or center periodically for evaluation by the burn team, modification of home care instructions, and planning for recon-structive surgery. Other patients receive ongoing care from the general or plastic surgeon who cared for them during the acute phase of their management. Still other patients require the services of a rehabilitation center and may be transferred to such a center for aggressive rehabilitation before going home.
Many patients require outpatient physical or
occupational therapy, often several times weekly. It is often the nurse who is
responsible for coor-dinating all aspects of care and ensuring that the
patient’s needs are met. Such coordination is an important aspect in assisting
a burn victim to achieve independence.
Patients
who return home after a severe burn injury, those who cannot manage their own
burn care, and those with inadequate support systems will need referral for
home care. During visits to the patient at home, the home care nurse assesses
the pa-tient’s physical and psychological status as well as the adequacy of the
home setting for safe and adequate care. The nurse mon-itors the patient’s
progress and adherence to the plan of care and notes any problems that
interfere with the patient’s ability to carry out the care. During the visit,
the nurse assists the patient and family with wound care and exercises.
Patients with severe or persistent depression or difficulty adjusting to
changes in their social and/or occupational roles are identified and referred
to the burn team for possible referral to a psychologist, psychi-atrist, or
vocational counselor.
The
burn team or home care nurse identifies community re-sources that may be
helpful for the patient and family. Several burn patient support groups and
other organizations throughout the United States offer services for burn
victims. They provide caring people (often recovered burn victims) who can visit
a burn patient in the hospital or home or telephone the patient and fam-ily
periodically to provide support and counseling about skin care, cosmetics, and
problems related to psychosocial adjustment. Such organizations, and many
regional burn centers, sponsor group meetings and social functions at which
outpatients are wel-come. Some also provide school-reentry programs and are
active in burn prevention activities. If more information is needed re-garding
burn prevention, the American Burn Association can help locate the nearest burn
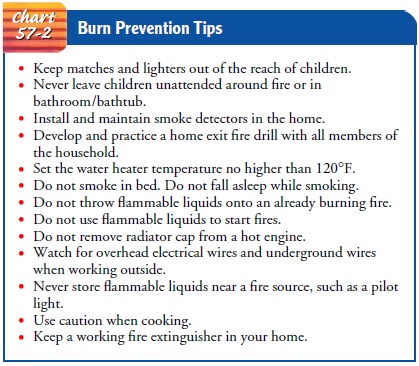
center and offer current burn prevention tips (see Chart 57-2).
Because
so much attention is given to the burn wound and the treatments that are
necessary to treat the burn wound and to prevent complications, the patient,
family, and health care providers may inadvertently ignore the patient’s
ongoing needs for health promotion and screening. Thus, the patient and fam-ily
are reminded of the importance of periodic health screening and preventive care
(eg, gynecologic examinations, dental care).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Demonstrates
activity tolerance required for desired daily activities
a) Obtains
sufficient sleep daily
b) Reports
absence of nightmares or sleep disturbances
c) Shows
gradually increasing tolerance and endurance in physical activities
d) Can
concentrate during conversations
e) Has
energy available to sustain desired daily activities
2) Adapts
to altered body image
a) Verbalizes
accurate description of alterations in body image and accepts physical
appearance
b) Demonstrates
interest in resources that may improve body appearance and function
c) Uses
cosmetics, wigs, and prostheses as desired to achieve acceptable appearance
d) Socializes
with significant others, peers, and usual social group
e) Seeks
and achieves return to role in family, school, and community as a contributing
member
3) Demonstrates
knowledge of required self-care and follow-up care
a) Describes
surgical procedures and treatments accurately
b) Verbalizes
detailed plan for follow-up care
c) Demonstrates
ability to perform wound care and pre-scribed exercises
d) Returns
for follow-up appointments as scheduled
e) Identifies
resource people and agencies to contact for specific problems
4) Exhibits
no complications
a) Demonstrates
full range of motion
b) Shows
no signs of withdrawal or depression
c) Displays
no psychotic behaviors
Related Topics