Chapter: Medical Surgical Nursing: Management of Patients With Burn Injury
Local and Systemic Responses to Burns
LOCAL AND SYSTEMIC RESPONSES TO BURNS
Burns
that do not exceed 25% TBSA produce a primarily local response. Burns that
exceed 25% TBSA may produce both a local and a systemic response and are
considered major burn injuries. This systemic response is due to the release of
cytokines and other mediators into the systemic circulation. The release of
local me-diators and changes in blood flow, tissue edema, and infection can
cause progression of the burn injury.
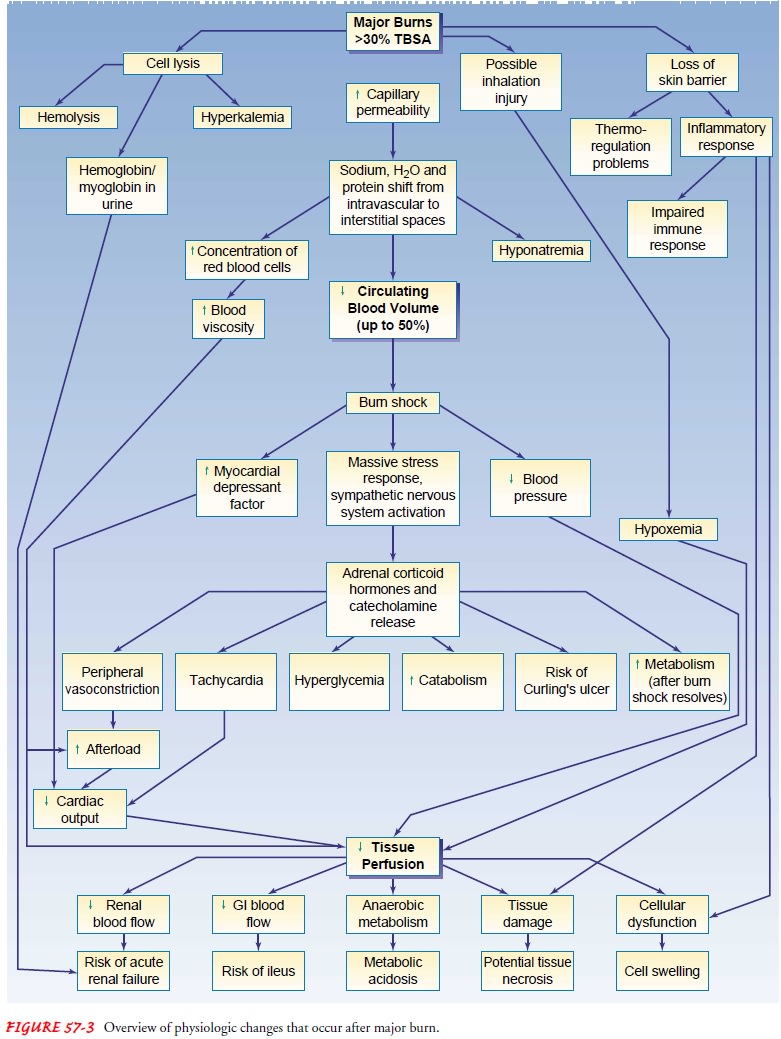
Pathophysiologic changes resulting from major burns during the initial burn-shock period include tissue hypoperfusion and organ hypofunction secondary to decreased cardiac output, fol-lowed by a hyperdynamic and hypermetabolic phase. The inci-dence, magnitude, and duration of pathophysiologic changes in burns are proportional to the extent of burn injury, with a max-imal response seen in burns covering 60% or more TBSA.
The
initial systemic event after a major burn injury is hemo-dynamic instability,
resulting from loss of capillary integrity and a subsequent shift of fluid,
sodium, and protein from the in-travascular space into the interstitial spaces.
Figure 57-3 illustrates the pathophysiologic processes in acute major burns.
Hemody-namic instability involves cardiovascular, fluid and electrolyte, blood
volume, pulmonary, and other mechanisms.
Cardiovascular Response
Hypovolemia is the immediate consequence of fluid
loss result-ing in decreased perfusion and oxygen delivery. Cardiac output
decreases before any significant change in blood volume is evi-dent. As fluid
loss continues and vascular volume decreases, car-diac output continues to fall
and blood pressure drops. This is the onset of burn shock. In response, the
sympathetic nervous system releases catecholamines, resulting in an increase in
peripheral re-sistance (vasoconstriction) and an increase in pulse rate.
Periph-eral vasoconstriction further decreases cardiac output. Myocardial
contractility may be suppressed by the release of inflammatory cytokine
necrosis factor (Wolf, Prough & Herndon, 2002).
Prompt fluid resuscitation maintains the blood
pressure in the low-normal range and improves cardiac output. Despite adequate
fluid resuscitation, cardiac filling pressures (central venous pres-sure,
pulmonary artery pressure, and pulmonary artery wedge pressure) remain low
during the burn-shock period. If inadequate fluid resuscitation occurs,
distributive shock will occur. Generally, the greatest volume of fluid leak
occurs in the first 24 to 36 hours after the burn, peaking by 6 to 8 hours. As
the cap-illaries begin to regain their integrity, burn shock resolves and fluid
returns to the vascular compartment. As fluid is reabsorbed from the
interstitial tissue into the vascular compartment, blood volume increases. If
renal and cardiac function is adequate, urinary output increases. Diuresis
continues for several days to 2 weeks.
Burn Edema
Local swelling due to thermal injury is often
extensive. Edema is defined as the presence of excessive fluid in the tissue
spaces (Lund, 1999). As previously noted, in burns involving less than 25%
TBSA, the loss of capillary integrity and shift of fluid are localized to the
burn itself, resulting in blister formation and edema only in the area of
injury. Patients with more severe burns develop massive systemic edema. Edema
is usually maximal after 24 hours. It begins to resolve 1 to 2 days post-burn
and usually is completely resolved in 7 to 10 days post-injury. Edema in burn
wounds can be reduced by avoiding excessive fluid during the early post-burn
period. Unnecessary over-resuscitation will in-crease edema formation in both
burn tissue and non-burn tissue.
As
edema increases in circumferential burns, pressure on small blood vessels and
nerves in the distal extremities causes an ob-struction of blood flow and
consequent ischemia. This compli-cation is known as compartment syndrome. The
physician may need to perform an escharotomy,
a surgical incision into the eschar (devitalized
tissue resulting from a burn), to relieve theconstricting effect of the burned
tissue.
Effects on Fluids, Electrolytes, and Blood Volume
Circulating
blood volume decreases dramatically during burn shock. In addition, evaporative
fluid loss through the burn wound may reach 3 to 5 L or more over a 24-hour
period until the burn surfaces are covered.
During
burn shock, serum sodium levels vary in response to fluid resuscitation.
Usually hyponatremia (sodium depletion) is present. Hyponatremia is also common
during the first week of the acute phase, as water shifts from the interstitial
to the vascular space.
Immediately
after burn injury, hyperkalemia (excessive potas-sium) results from massive
cell destruction. Hypokalemia (potas-sium depletion) may occur later with fluid
shifts and inadequate potassium replacement.
At the time of burn injury, some red blood cells
may be de-stroyed and others damaged, resulting in anemia. Despite this, the
hematocrit may be elevated due to plasma loss. Blood loss during surgical
procedures, wound care, and diagnostic studies and on-going hemolysis further
contribute to anemia. Blood transfusions are required periodically to maintain
adequate hemoglobin levels for oxygen delivery. Abnormalities in coagulation,
including a de-crease in platelets (thrombocytopenia) and prolonged clotting
and prothrombin times, also occur with burn injury.
Pulmonary Response
Inhalation injury is the leading cause of death in fire victims. It is estimated that half of these deaths could have been prevented with use of a smoke detector. Often, burn victims make it out of a burning home safely. However, once they are outside, they may realize that their loved ones, pets, or valuable items are still inside the burning home. They then re-enter the burning home and are overcome with toxic smoke and fumes and become disoriented or unconscious.
Inhalation injury has a significant impact on
survivability of a burn patient. Deterioration in severely burned patients can
occur without evidence of a smoke inhalation injury. Bronchoconstric-tion
caused by release of histamine, serotonin, and thromboxane, a powerful vasoconstrictor,
as well as chest constriction secondary to circumferential full-thickness chest
burns causes this deteriora-tion. One third of all burn patients have a
pulmonary problem related to the burn injury (Flynn, 1999). Even without
pulmo-nary injury, hypoxia (oxygen starvation) may be present. Early in the
postburn period, catecholamine release in response to the stress of the burn
injury alters peripheral blood flow, thereby re-ducing oxygen delivery to the
periphery. Later, hypermetabolism and continued catecholamine release lead to
increased tissue oxy-gen consumption, which can lead to hypoxia. To ensure that
ad-equate oxygen is available to the tissues, supplemental oxygen may be
needed.
Pulmonary injuries fall into several categories:
upper airway in-jury; inhalation injury below the glottis, including carbon
mono-xide poisoning; and restrictive defects. Upper airway injury results from
direct heat or edema. It is manifested by mechanical ob-struction of the upper
airway, including the pharynx and larynx. Because of the cooling effect of
rapid vaporization in the pul-monary tract, direct heat injury does not
normally occur below the level of the bronchus. Upper airway injury is treated
by early naso-tracheal or endotracheal intubation.
Inhalation
injury below the glottis results from inhaling the products of incomplete
combustion or noxious gases. These prod-ucts include carbon monoxide, sulfur
oxides, nitrogen oxides, aldehydes, cyanide, ammonia, chlorine, phosgene,
benzene, and halogens. The injury results directly from chemical irritation of
the pulmonary tissues at the alveolar level. Inhalation injuries be-low the
glottis cause loss of ciliary action, hypersecretion, severe mucosal edema, and
possibly bronchospasm. The pulmonary surfactant is reduced, resulting in
atelectasis (collapse of alveoli). Expectoration of carbon particles in the
sputum is the cardinal sign of this injury.
Carbon monoxide is probably the most common cause
of inhalation injury because it is a byproduct of the combustion of organic
materials and is therefore present in smoke. The patho-physiologic effects are
due to tissue hypoxia, a result of carbon monoxide combining with hemoglobin to
form carboxyhemo-globin, which
competes with oxygen for available hemoglobin-binding sites. The affinity of
hemoglobin for carbon monoxide is 200 times greater than that for oxygen.
Treatment usually con-sists of early intubation and mechanical ventilation with
100% oxygen. However, some patients may require only oxygen ther-apy, depending
on the extent of pulmonary injury and edema. Administering 100% oxygen is
essential to accelerate the removal of carbon monoxide from the hemoglobin
molecule.
Restrictive defects arise when edema develops under
full-thickness burns encircling the neck and thorax. Chest excursion may be
greatly restricted, resulting in decreased tidal volume. In such situations,
escharotomy is necessary.
Pulmonary abnormalities are not always immediately
apparent. More than half of all burn victims with pulmonary involvement do not
initially demonstrate pulmonary signs and symptoms. Any patient with possible
inhalation injury must be observed for at least 24 hours for respiratory
complications. Airway obstruction may occur very rapidly or develop
in hours. Decreased lung compli-ance, decreased arterial oxygen levels, and
respiratory acidosis may occur gradually over the first 5 days after a burn.
Indicators
of possible pulmonary damage include the following:
·
History indicating that the
burn occurred in an enclosed area
·
Burns of the face or neck
·
Singed nasal hair
·
Hoarseness, voice change, dry
cough, stridor, sooty sputum
·
Bloody sputum
·
Labored breathing or tachypnea
(rapid breathing) and other signs of reduced oxygen levels (hypoxemia)
·
Erythema and blistering of the
oral or pharyngeal mucosa
Diagnosis
of inhalation injury is an important priority for many burn victims. Serum
carboxyhemoglobin levels and arterial blood gas levels are frequently used to
assess for inhalation inju-ries. Bronchoscopy and xenon-133 (133Xe)
ventilation-perfusion scans can also be used to aid diagnosis in the early
postburn pe-riod. Pulmonary function studies may also be useful in diagnos-ing
decreased lung compliance or obstructed airflow (Fitzpatrick & Cioffi,
2002; Flynn, 1999).
Pulmonary
complications secondary to inhalation injuries in-clude acute respiratory
failure and acute respiratory distress syn-drome (ARDS). Respiratory failure
occurs when impairment of ventilation and gas exchange is life-threatening. The
immediate intervention is intubation and mechanical ventilation. If
ventila-tion is impaired by restricted chest excursion, immediate chest
es-charotomy is needed. ARDS may develop in the first few days after the burn
injury secondary to systemic and pulmonary re-sponses to the burn and
inhalation injury.
Other Systemic Responses
Renal
function may be altered as a result of decreased blood vol-ume. Destruction of
red blood cells at the injury site results in free hemoglobin in the urine. If
muscle damage occurs (eg, from electrical burns), myoglobin is released from
the muscle cells and excreted by the kidney. Adequate fluid volume replacement
restores renal blood flow, increasing the glomerular filtration rate and urine
volume. If there is inadequate blood flow through the kidneys, the hemoglobin
and myoglobin occlude the renal tubules, resulting in acute tubular necrosis
and renal failure.
The immunologic defenses of the body are greatly
altered by burn injury. Serious burn injury diminishes resistance to
infec-tion. As a result, sepsis remains the leading cause of death in
ther-mally injured patients (Cioffi, 2001). The loss of skin integrity is
compounded by the release of abnormal inflammatory factors, altered levels of
immunoglobulins and serum complement, im-paired neutrophil function, and a
reduction in lymphocytes (lym-phocytopenia). Research suggests that burn injury
results in loss of T-helper cell lymphocytes (Munster, 2002). There is a
signif-icant impairment of the production and release of granulocytes and macrophages
from bone marrow after burn injury. The re-sulting immunosuppression places the
burn patient at high risk for sepsis.
Loss
of skin also results in an inability to regulate body tem-perature. Burn
patients may therefore exhibit low body temper-atures in the early hours after
injury. Then, as hypermetabolism resets core temperatures, burn patients become
hyperthermic for much of the postburn period, even in the absence of infection.
Two potential gastrointestinal complications may
occur: par-alytic ileus (absence of intestinal peristalsis) and Curling’s
ulcer. Decreased peristalsis and bowel sounds are manifestations of par-alytic
ileus resulting from burn trauma. Gastric distention and nausea may lead to
vomiting unless gastric decompression is ini-tiated. Gastric bleeding secondary
to massive physiologic stress may be signaled by occult blood in the stool,
regurgitation of “coffee ground” material from the stomach, or bloody vomitus.
These signs suggest gastric or duodenal erosion (Curling’s ulcer).
Related Topics