Chapter: Medical Surgical Nursing: Management of Patients With Burn Injury
Acute or Intermediate Phase of Burn Care
ACUTE OR INTERMEDIATE PHASE OF BURN CARE
The acute or intermediate phase of burn care
follows the emergent/ resuscitative phase and begins 48 to 72 hours after the
burn injury. During this phase, attention is directed toward continued
assess-ment and maintenance of respiratory and circulatory status, fluid and
electrolyte balance, and gastrointestinal function. Infection pre-vention, burn
wound care (ie, wound cleaning, topical antibacterial therapy, wound dressing,
dressing changes, wound débridement, and wound grafting), pain management, and
nutritional support are priorities at this stage and will be discussed in
detail.
Airway obstruction caused by upper airway edema can
take as long as 48 hours to develop. Changes detected by x-ray and arte-rial
blood gases may occur as the effects of resuscitative fluid and the chemical
reaction of smoke ingredients with lung tissues be-come apparent. The arterial
blood gas values and other parameters determine the need for intubation or
mechanical ventilation.
As capillaries regain integrity, at 48 or more
postburn hours, fluid moves from the interstitial to the intravascular
compartment and diuresis begins (Table 57-4). If cardiac or renal function is
inadequate, for instance in the elderly patient or in the patient with
preexisting cardiac disease, fluid overload occurs and symp-toms of congestive
heart failure may result. Early detection allows for early intervention and carefully
calculated fluid intake. Vasoactive medications, diuretics, and fluid
restric-tion may be used to support circulatory function and prevent congestive
heart failure and pulmonary edema.
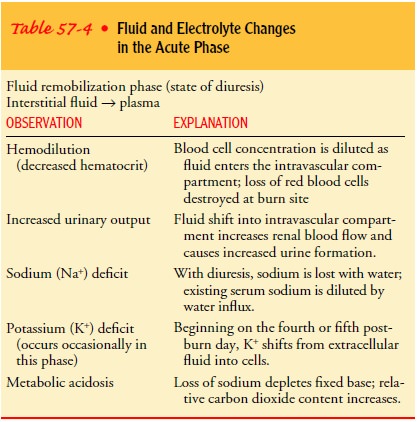
Cautious
administration of fluids and electrolytes continues during this phase of burn
care because of the shifts in fluid from the interstitial to intravascular
compartments, losses of fluid from large burn wounds, and the patient’s
physiologic responses to the burn injury. Blood components are administered as
needed to treat blood loss and anemia.
Fever is common in burn patients after burn shock resolves. A resetting of the core body temperature in severely burned patients results in a body temperature a few degrees higher than normal for several weeks after the burn. Bacteremia and septicemia also cause fever in many patients. Acetaminophen (Tylenol) and hypo-thermia blankets may be required to maintain body temperature in a range of 37.2° to 38.3°C (99° to 101°F) to reduce metabolic stress and tissue oxygen demand.
Central
venous, peripheral arterial, or pulmonary artery ther-modilution catheters may
be required for monitoring venous and arterial pressures, pulmonary artery
pressures, pulmonary capillary wedge pressures, or cardiac output. Generally,
however, invasive vascular lines are avoided unless essential because they
provide an additional port for infection in an already greatly compromised
patient.
Infection
progressing to septic shock is the major cause of death in patients who have
survived the first few days after a major burn. The immunosuppression that
accompanies exten-sive burn injury places the patient at high risk for sepsis.
The infection that begins within the burn site may spread to the bloodstream.
Infection Prevention
Despite
aseptic precautions and the use of topical antimicrobial agents, the burn wound
is an excellent medium for bacterial growth and proliferation. Bacteria such as
Staphylococcus, Proteus, Pseudo-monas,
Escherichia coli, and Klebsiella find
optimal conditions forgrowth within the burn wound. The burn eschar is a
nonviable crust with no blood supply; therefore, neither polymorpho-nuclear
leukocytes or antibodies nor systemic antibiotics can reach the area.
Phenomenal numbers of bacteria—more than 1 billion per gram of tissue—may
appear and subsequently spread to the bloodstream or release their toxins,
which reach distant sites. Staph-ylococci and enterococci are the organisms
responsible for more than 50% of nosocomial bloodstream infections in patients
with burn injuries. Fungi such as Candida
albicans also grow easily in burn wounds.
When
the burn wound is healing through spontaneous re-epithelialization or is being
prepared for skin grafting, it must be protected from sepsis. Burn wound sepsis
has these characteristics:
·
105
bacteria per gram of tissue
·
Inflammation
·
Sludging and thrombosis of
dermal blood vessels
The primary source of bacterial infection appears
to be the patient’s intestinal tract, the source of most microbes. The
intestinal mucosa normally serves as a barrier to keep the internal
environ-ment free from a variety of pathogens. After a severe burn injury, the
intestinal mucosal barrier becomes markedly permeable. Be-cause of this impaired
intestinal mucosal barrier, the disturbed microbial flora and endotoxins found
in the intestinal lumen pass freely into the systemic circulation, finally
causing infection. If the intestinal mucosa receives some type of protection
against permeability change, infection could be avoided. Early enteral feeding
is one step to help avoid this increased intestinal perme-ability and prevent
early endotoxin translocation (Cioffi, 2000; Peng, Yuan & Ziao, 2001).
Infection
impedes burn wound healing by promoting excessive inflammation and damaging
tissue. A major secondary source of pathogenic microbes is the environment.
Infection control is a major role of the burn team in providing appropriate
burn wound care. Cap, gown, mask, and gloves are worn while caring for the
patient with open burn wounds. Clean technique is used when caring directly for
burn wounds.
Tissue
specimens are obtained for culture regularly to moni-tor colonization of the
wound by microbial organisms. These may be swab, surface, or tissue biopsy
cultures. Swab or surface cultures are noninvasive, simple, and painless.
However, data ob-tained from such cultures apply only to the area sampled;
there-fore, invasive wound biopsy cultures may be required. Antibiotics are
seldom prescribed prophylactically because of the risk of pro-moting resistant
strains of bacteria. Systemic antibiotics are ad-ministered when there is
documentation of burn wound sepsis or other positive cultures such as urine,
sputum, or blood. Sensitivity of the organisms to the prescribed antibiotics
should be deter-mined before administration. Several parenteral antimicrobial
agents may be given together to treat the infection. Careful at-tention is paid
to antibiotic use in the burn unit because inap-propriate use of antibiotics
significantly affects the microbial flora present in the unit.
Wound Cleaning
Various
measures are used to clean the burn wound. Hydro-therapy
in the form of shower carts, individual showers, and bedbaths can be used
to clean the wounds. Total immersion hydro-therapy is performed in some
settings. Because of the high risk of infection and sepsis, the use of plastic
liners and thorough de-contamination of hydrotherapy equipment and wound care
areas are necessary to prevent cross-contamination. Tap water alone can be used
for burn wound cleansing. The temperature of the water is maintained at 37.8°C (100°F), and the temperature
of the room should be maintained between 26.6° and 29.4°C (80° to 85°F). Hydrotherapy, in
whatever form, should be limited to a 20- to 30-minute period to prevent
chilling of the patient and additional metabolic stress.
During the bath, the patient is encouraged to be as
active as possible. Hydrotherapy provides an excellent opportunity for
ex-ercising the extremities and cleaning the entire body. When the patient is
removed from the tub after the bath, any residue ad-hering to the body is
washed away with a clear water spray or shower. Unburned areas, including the
hair, must be washed reg-ularly as well. At the time of wound cleaning, all
skin is inspected for any hints of redness, breakdown, or local infection. Hair
in and around the burn area, except the eyebrows, should be clipped short.
Intact blisters may be left, but the fluid should be aspirated with a needle
and syringe and discarded.
Conscientious
management of the burn wound is essential. When nonviable loose skin is
removed, aseptic conditions must be established. Wound cleaning is usually
performed at least daily in wound areas that are not undergoing surgical
intervention. When the eschar begins to separate from the viable tissue beneath
(approximately 1.5 to 2 weeks after the burn), more frequent cleaning and
débridement may be in order.
After
the burn wounds are cleaned, they are gently patted with towels and the
prescribed method of wound care is performed. Physician preferences, the
availability of skilled nursing staff, and resources in terms of number of
personnel, supplies, and time must be considered in choosing the best method
for a given pa-tient. Whatever the method, the goal is to protect the wound
from overwhelming proliferation of pathogenic organisms and invasion of deeper
tissues until either spontaneous healing or skin grafting can be achieved.
Patient comfort and ability to participate in the
prescribed treatment are also important considerations. Wound care proce-dures,
particularly tub baths, are metabolically stressful. There-fore, the patient is
assessed for signs of chilling, fatigue, changesin hemodynamic status, and pain
unrelieved by analgesic med-ications or relaxation techniques.
Topical Antibacterial Therapy
There is general agreement that some form of
antimicrobial ther-apy applied to the burn wound is the best method of local
care in extensive burn injury. Topical antibacterial therapy does not
ster-ilize the burn wound; it simply reduces the number of bacteria so that the
overall microbial population can be controlled by the body’s host defense
mechanisms. Topical therapy promotes con-version of the open, dirty wound to a
closed, clean one.
Criteria
for choosing a topical agent include the following:
·
It is effective against
gram-negative organisms, Pseudomonasaeruginosa,
Staphylococcus aureus, and even fungi.
·
It is clinically effective.
·
It penetrates the eschar but
is not systemically toxic.
·
It does not lose its
effectiveness, allowing another infection to develop.
·
It is cost-effective,
available, and acceptable to the patient.
·
It is easy to apply,
minimizing nursing care time.
The three most commonly used topical agents are
silver sulfadi-azine (Silvadene), silver nitrate, and mafenide acetate
(Sulfamylon). These agents are described in Table 57-5. Many other topical
agents are available, including povidone–iodine ointment 10% (Betadine),
gentamicin sulfate, nitrofurazone (Furacin), Dakin’s solution, acetic acid,
miconazole, and chlortrimazole. Bacitracin may be used for facial burns or on
skin grafts initially.
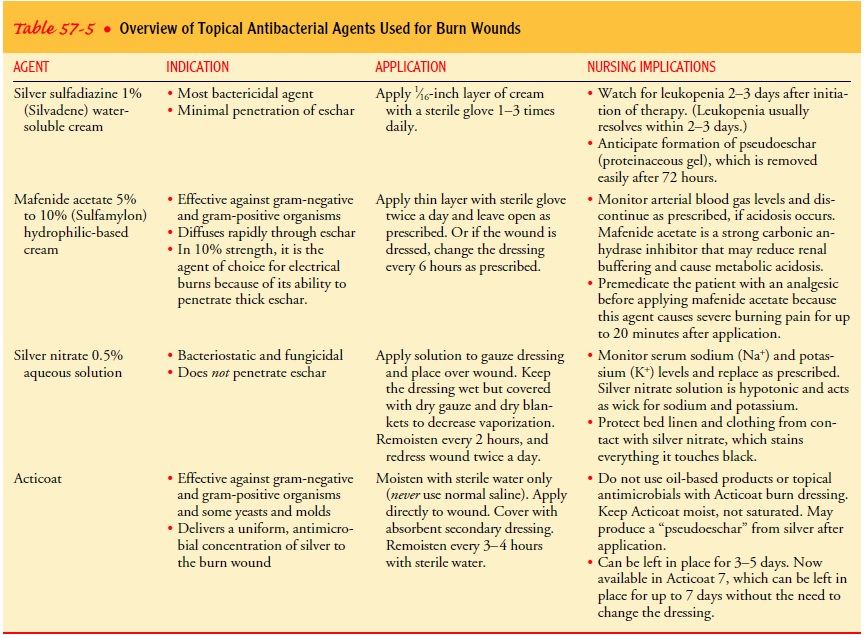
A
newer product used in burn wound care is Acticoat Anti-microbial Barrier
dressing. Acticoat is a silver-coated dressing approved for treatment of burn
wounds and donor sites. This
dressing is kept moist with water for a controlled, sustained re-lease of
silver over the wound to provide an antimicrobial barrier. Acticoat has been
shown to have a better antimicrobial perfor-mance than the traditional
silver-based products commonly used in burn wound treatment. Acticoat is also
cost-effective. The dressing can be left in place for up to 5 days, decreasing
patient discomfort, the cost of dressing supplies, and nursing time for
dressing changes. The dressing has been shown clinically to be very effective
for prevention of burn wound infection (Yin, Langford & Burrell, 1999).
No single topical medication is universally
effective. Using dif-ferent agents at different times in the postburn period
may be necessary. Bacteriologic cultures are required to monitor the effect of
topical medications. Prudent use and alternation of anti-microbial agents
result in less resistant strains of bacteria, greater effectiveness of the
agents, and a decreased risk of sepsis.
Before a topical agent is reapplied, the previously applied top-ical agent must be thoroughly removed. The number of times the dressings are changed and soaked is planned to promote optimal therapeutic use of the topical agent.
Wound Dressing
When
the wound is clean, the burned areas are patted dry and the prescribed topical
agent is applied; the wound is then covered with several layers of dressings. A
light dressing is used over joint areas to allow for motion (unless the
particular area has a graft and motion is contraindicated). A light dressing is
also applied over areas for which a splint has been designed to conform to the
body contour for proper positioning. Circumferential dressings should be
applied distally to proximally. If the hand or foot is burned, the fingers and
toes should be wrapped individually to promote adequate healing.
Burns
to the face may be left open to air once they have been cleaned and the topical
agent has been applied. Careful attention must be given to burns left exposed
to ensure that they do not dry out and convert to a deeper burn.
Close communication and cooperation among the
patient, surgeon, nurse, and other health care team members are essential for
optimal burn wound care. Different wound areas on a given patient may require a
variety of wound care techniques. Diagrams posted at the bedside are useful to
inform staff of the current pre-scription for wound care, splints to be applied
over dressings, and the exercise regimen to be followed before dressings are
reapplied.
OCCLUSIVE METHOD
There
is a role for occlusive dressings in treating specific wounds. An occlusive
dressing is a thin gauze that is impregnated with a topical antimicrobial agent
or that is applied after topical anti-microbial application. Occlusive
dressings are most often used over areas with new skin grafts. Their purpose is
to protect the graft, promoting an optimal condition for its adherence to the
recipient site. Ideally, these dressings remain in place for 3 to 5 days, at
which time they are removed for examination of the graft.
When
these dressings are applied, precautions are taken to prevent two body surfaces
from touching, such as fingers or toes, ear and scalp, the areas under the
breasts, any point of flexion, or between the genital folds. Functional body
alignment positions are maintained by using splints or by careful positioning
of the patient.
Dressing Changes
Dressings
are changed in the patient’s unit, hydrotherapy room, or treatment area
approximately 20 minutes after an analgesic agent is administered. They may
also be changed in the operat-ing room after the patient is anesthetized. A
mask, goggles, hair cover, disposable plastic apron or cover gown, and gloves
are worn by health care personnel when removing the dressings. The outer
dressings are slit with blunt scissors, and the soiled dress-ings are removed
and disposed of in accordance with established procedures for contaminated
materials.
Dressings that adhere to the wound can be removed
more comfortably if they are moistened with tap water or if the patient is allowed
to soak for a few moments in the tub. The remaining dressings are carefully and
gently removed. The patient may partic-ipate in removing the dressings,
providing some degree of control over this painful procedure. The wounds are
then cleaned and débrided to remove debris, any remaining topical agent,
exudate, and dead skin. Sterile scissors and forceps may be used to trim loose
eschar and encourage separation of devitalized skin. During this procedure, the
wound and surrounding skin are carefully inspected. The color, odor, size,
exudate, signs of re-epithelialization, andother characteristics of
the wound and the eschar and any changes from the previous dressing change are
noted.
Wound Débridement
As
debris accumulates on the wound surface, it can retard ker-atinocyte migration,
thus delaying the epithelialization process. Débridement, another facet of burn
wound care, has two goals:
·
To remove tissue contaminated
by bacteria and foreign bodies, thereby protecting the patient from invasion of
bacteria
·
To remove devitalized tissue
or burn eschar in preparation for grafting and wound healing
There
are three types of débridement—natural, mechanical, and surgical.
NATURAL DÉBRIDEMENT
With
natural débridement, the dead tissue separates from the un-derlying viable
tissue spontaneously. After partial- and full-thickness burns, bacteria that
are present at the interface of the burned tis-sue and the viable tissue
underneath gradually liquefy the fibrils of collagen that hold the eschar in place for the first or second
postburn week. Proteolytic and other natural enzymes cause this phenomenon.
Using antibacterial topical agents, however, tends to slow this natural process
of eschar separation. It is advanta-geous to the patient to speed this process
through other means, such as mechanical or surgical débridement, thereby
reducing the time during which bacterial invasion and other iatrogenic
prob-lems may arise.
MECHANICAL DÉBRIDEMENT
Mechanical
débridement involves using surgical scissors and for-ceps to separate and
remove the eschar. This technique can be performed by skilled physicians,
nurses, or physical therapists and is usually done with daily dressing changes
and wound cleaning procedures. Débridement by these means is carried out to the
point of pain and bleeding. Hemostatic agents or pressure can be used to stop
bleeding from small vessels.
Dressings
are also useful débriding agents. Coarse-mesh dress-ings applied dry or
wet-to-dry (applied wet and allowed to dry) will slowly débride the wound of
exudate and eschar when they are removed. Topical enzymatic débridement agents
are available to promote débridement of the burn wounds. Because such agents do
not have antimicrobial properties, they should be used with topical
antibacterial therapy to protect the patient from bac-terial invasion.
SURGICAL DÉBRIDEMENT
Early surgical excision to remove devitalized
tissue along with early burn wound closure is now being recognized as one of
the most important factors contributing to survival in a patient with a major
burn injury. Aggressive surgical wound closure has re-duced the incidence of
burn wound sepsis, thus improving sur-vival rates (Gibran & Heimbach,
2000). Early excision is carried out before the natural separation of eschar is
allowed to occur.
Surgical débridement is an operative procedure
involving either primary excision (surgical removal of tissue) of the full
thick-ness of the skin down to the fascia (tangential excision) or shaving the
burned skin layers gradually down to freely bleeding, viable tis-sue. Surgical
excision is initiated early in burn wound manage-ment. This may be performed a
few days after the burn or as soon as the patient is hemodynamically stable and
edema has decreased.
Ideally,
the wound is then covered immediately with a skin graft, if needed, and an
occlusive dressing. If the wound bed is not ready for a skin graft at the time
of excision, a temporary biologic dress-ing may be used until a skin graft can
be applied during subse-quent surgery.
The
use of surgical excision carries with it risks and compli-cations, especially
with large burns. The procedure creates a high risk of extensive blood loss (as
much as 100 to 125 mL of blood per percent body surface excised) and lengthy
operating and anesthesia time. However, when conducted in a timely and
effi-cient manner, surgical excision results in shorter hospital stays and
possibly a decreased risk of complications from invasive burn wound sepsis.
Gerontologic Considerations
Eschar
separation in full-thickness burns is typically delayed in elderly patients,
and older patients are frequently poor risks for surgical excision. Therefore,
prolonged hospitalization, immobi-lization, and associated problems may be
common. If the elderly patient can tolerate surgery, early excision with skin
grafting is the treatment of choice because it decreases the mortality rate in
this population. Prevention of complications of prolonged hos-pitalization,
immobility, and surgery is essential in the care of the elderly burn patient.
Related Topics