Chapter: Medicine Study Notes : Haematology and Immunology
Leukaemia
Leukaemia
·
Leuk: Greek for white
·
= Cancer dominantly of white
cells arising in MARROW. Lymphoma
primarily arises in lymph nodes
·
Summary:
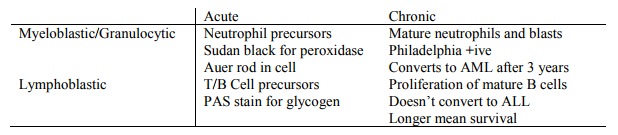
Chronic Leukaemia
· Chronic Myeloblastic Leukaemia (CML): Converts to AML/AGL.
· Chronic Lymphoblastic Leukaemia (CLL)
Acute Leukaemia
·
Rapid onset, 100% mortality
within 3 months if untreated
·
Very undifferentiated
(anaplastic) cells: blasts, no normal cells in blood
· Types:
o Acute Myeloblastic Leukaemia (AML). Chance of cure with chemo alone = 20
– 40%. With transplant = 60%. Has Auer rob in blast
o Acute Lymphoblastic Leukaemia (ALL)
·
Presentation:
o Tired due to anaemia, breathless
o Bleeding due to ¯platelets, nose bleeds
o Bacterial infection
o Hepatosplenomegaly, lymph nodes, bone pain (push on sternum)
· Investigations:
o FBC: ¯Hb, ¯platelets, white count: High, normal or low (sometimes leukaemia cells stay in marrow)
o Bone marrow: > 30% of nucleated cells in the marrow are leukaemic
blasts
·
Classification:
o Cytochemistry:
§ Staining. PAS - +ive stain for
glycogen Þ lymphoblastic
§ Sudan black +ive for peroxidase Þ myeloblastic
o Immunology: flow cytometry
o Cytogenetics
Treatment
·
Supportive Care:
o Antibiotics, platelet/RBC transfusion
o Venous catheter: Hickman catheter
·
Cytotoxic Treatment:
o Complex multi-drug protocols
o Remission induction: 1-4 weeks depending on protocol. FBC normal and < 5% blasts in marrow (that‟s normal). AML – achieved in 70 – 80%. ALL – achieved in 70 – 80% of adults, 95% of kids
o Consolidation: more drugs to mop up residual blasts, including CNS
prophylaxis (some drugs don‟t penetrate CNS well)
o But 60 – 80% chance of relapse over next 2 – 4 years
·
Bone Marrow Transplantation:
o = Haematopoietic stem cell transplantation
· Kill of leukaemic cells with dose: but limited by marrow toxicity. With marrow transplantation can push dose higher (limit is organ toxicity) if cancer is responsive
· Process: patient and donor preparation, conditioning (chemo & high does radiation), stem cell infusion, neutropenic phase, post neutropenic phase
·
Sources of stem cells: Self
(autologous), twin (syngenic), HLA matched sibling (allogenic), HLA partial
matched sibling, matched unrelated donor (MUD)
·
Peritransplant mortality = 20%
Fever in a Neutropenic Patient
·
Eg in patients undergoing
chemotherapy
·
Indicators of serious infection:
o Signs and symptoms of infection will be reduced – can‟t mount an
inflammatory response
o Temperature:
§ > 38.5 C
§ > 38 for 4 hours
§ Patient fells unwell but no temperature
o Neutropenia:
§ Neutrophils < 0.5 * 10E9/L (less than 0.2 Þ serious
concern)
§ Neutrophils falling
§ Prolonged neutropenia (> 7 days)
·
Types of infection (drives
focused history)
o Respiratory: SOB, cough
o Skin infection
o Mouth and teeth
o Perianal (pain on moving bowels and wiping)
o Pain around central line
o Less often: bowel & UTI
·
Focused exam:
o Signs of septic shock: Pulse, BP and peripheral circulation
o Chest: percussion and auscultation
o Mouth: a good look around – abscesses will be sensitive to pain
o Skin infections, especially lines
o Quick abdominal
o Exam perianal area – test for sensitivity to touch. Don‟t do PR (risk of minor trauma ® bacteraemia)
·
Investigations:
o FBC
o Blood culture (debate about whether to take it from the central line or
not)
o CXR
o Swabs from anything that looks infected, including central line
o Maybe CRP: in bacteraemia
·
Normally don‟t find
anything. Over half infections are low
grade line infections
·
If in doubt, treat empirically now.
If infected will deteriorate quickly:
o Gentamycin + Ticarcillin (synthetic penicillin)
o Monotherapy (eg imipenem)
o +/- Vancomycin (for staph line sepsis)
·
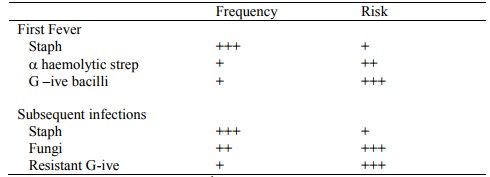
Causes of infection:
·
Subsequent fevers: longer in
hospital (hospital acquired infection), longer on antibiotics, etc
·
If fever persists:
o Repeat the above exam and investigations – but unlikely to add anything
new
o Choices:
§ Change antibiotics
§ Consider antifungal: Amphotericin.
Watch for nephrotoxicity and the patient feels awful
·
Obscure fevers:
o Central venous line infection
o Occult sinusitis (check with CT)
o Hepatosplenic candidiasis (check with CT ® abscess ® biopsy)
o Pulmonary/disseminated aspergillus (doesn‟t respond to amphotericin)
o Viral
o Drugs
·
Prevention:
o Avoid hospitalisation
o Strict hand washing
o Avoid invasive procedures (beware interventionist surgeons!)
o Care of IV devices
o Consider prophylactic antimicrobials
· Prophylaxis
o Bacteria: selective gut decontamination (origin of many infections is bowel flora): Ciprofloxacin (fluorinated quinolone). Arguments for and against
o Anti-fungal: Fluconazole, Itraconazole (OK for prophylaxis, not so good as amphotericin for established infection)
o Anti-viral: acyclovir (for HSV), ganciclovir (for CMV)
o Anti-pneumocystis: co-trimoxazole (but beware marrow suppression) or
aerolised pentamidine
· Other possible treatments:
o Granulocyte-CSF: try to marrow production of neutrophils
o Maybe g-globulin infusions
o Transfuse granulocytes: emerging area
Related Topics