Chapter: Medicine Study Notes : Haematology and Immunology
Haemostasis
Haemostasis
·
Necessary factors for haemostasis
(stopping bleeding):
o Vasoconstriction
o Platelets
o Coagulation (= fibrin production)
Coagulation
·
Key reaction: fibrinogen ® fibrin
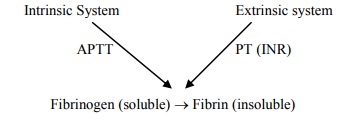
· Intrinsic pathway:
o XII ® II via IX and VIII
o Triggered by damage to endothelium
o Measured by Partial thromboplastin Time (PTT) = Activated PTT (APTT).
Also called PTTK
o Reduced by heparin treatment
· Extrinsic Pathway:
o VII ® II
o Triggered by chemicals extrinsic to blood stream
o Measured by Prothrombin time or INR (International Normalised Ratio): ratio of Patient PT to Control. Normal < 1.3. INR mainly measures top end of the extrinsic pathway – so INR may not be affected by heparin even though it affects the common pathway. APPT more sensitive to ¯common pathway
o Reduced by warfarin treatment
Hypo-Coagulation Diseases
·
Congenital:
o Haemophilia A
o Haemophilia B
o Von Willebrand‟s Disease
o Rare factor deficiencies
· Acquired:
o Liver diseases ® ¯coagulation factors
o DIC
o Vitamin K deficiency: needed for factors 2, 7, 9 and 10
o Uraemia: renal failure ® ¯platelets and coagulation function
o Massive blood transfusions ® dilution of clotting factors
o Factor inhibitors
Von Willebrand’s Disease
·
Bleeding time, APTT due to ¯ VIII (VW factor is a binding protein for VIII)
·
Symptoms: Superficial bleeds –
mouth, nose, gut, bruising, heavy menstrual bleeding
·
Autosomal dominant
·
Comes in mild, moderate and
severe forms
Haemophilia
·
Ratio of 4:1 of A (¯factor
VIII) to B (¯factor IX)
·
Prevalence of 13 – 18 per 100,000
males in Wellington (high)
·
Symptoms: bleeding into soft
tissues, joints, dental extraction. Deep bleeds ® major
orthopaedic implications. NOT superficial or gut
·
Classification:
o Severe: < 1% - joint bleeds, e.g. once a fortnight or month
o Moderate: 1 – 4 % - some joint bleeds, main problem with trauma, not
spontaneous bleeds
o Mild: 5 – 25% - main problem trauma
·
Lab diagnosis:
o INR: normal
o APTT: prolonged
o Fibrinogen: normal
o Platelets: normal
o Bleeding time: normal
o Factor assay reduced (do VIII first then IX)
·
Symptoms of a joint bleed:
o Strange sensation: not really a pain – treat at this point, they will
know despite no signs yet
o Swelling
·
Treatment:
o Factor replacement: either prophylactic or on demand
o Choice of factor product: blood derived or recombinant
o Management of inhibitors
Disseminated Intravascular Coagulation (DIC)
·
= Laying down fibrin
inappropriately within vasculature
·
Causes:
o Activation of extrinsic system by thromboplastin (triggers VII).
Thromboplastin is a lipoprotein substance from cell membranes. Due to: massive
injury (release of thromboplastin), septicaemia (damage to endothelium), tumour
cells breaking down
o Activation of intrinsic system: anoxia, acidosis, sepsis, burns
o Direct activation of II & X: amniotic fluid embolism, pancreatitis (® release
of toxic enzymes into blood)
·
Outcomes:
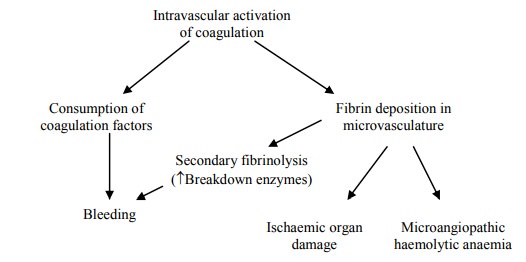
· Lab screen:
o PT
(Prothrombin time)
o APTT
o ¯Fibrinogen
o ¯Platelets
o Fibrin
degradation products
·
Treatment:
o Correct cause
o Platelet transfusion
o Fresh Frozen plasma
o Cryoprecipitate
Hypercoagulable States
·
Primary Causes:
o Factor V Leiden:
§ Most common primary cause
§ Point mutation on factor V prevents breakdown ® levels of
Va ® hypercoagulable
§ Heterozygous have lifetime risk of 30 – 40% of thrombotic event,
Homozygous then 50 – 60%
§ In thrombotic patients, 20 – 40% have factor V Leiden, mainly in
Caucasians
o Prothrombin gene mutation
o Antithrombin 3 deficiency:
§ ® Reduced
breakdown of thrombin
§ Heparin co-factor, a2 globulin
§ Autosomal dominant, 1:2-5000 in Caucasian
§ Found in 2 – 3 % of DVTs
§ Can also cause mesenteric or brachial thrombosis. These are rare so ® index of
suspicion
o Protein C or S deficiency
o Homocysteinaemia
·
Secondary Causes:
o Malignancy
o Pregnancy and for 6 weeks afterwards: hypercoagulable, stasis, venous
compression. If concurrent primary disorder then prophylaxis with sc heparin
(warfarin contra-indicated)
o Stasis: immobilisation, surgery, local pressure
o Age
o Myeloproliferative disorders
o Antiphospholipid Syndrome (acquired, aggressive)
o Infection
o Trauma
Data Interpretation
·
Serum = plasma that‟s clotted:
i.e. no clotting factors
· Citrated plasma: citrate chelates calcium – so can‟t act as a co-factor in clotting. Add Ca to reverse
· Aspirin for Coronary Heart Disease mimics VWD. (i.e. bleeding time, everything else normal). T½ of platelets = 3 – 4 days. Need to stop aspirin 10 days before surgery. ½ an aspirin enough to increase bleeding time. 45 minutes to have an effect after oral dose
·
Heparin ® APPT
·
Fractionated Heparin ® TT (APPT
may be normal)
·
Warfarin ® INR
·
Try to determine deficiency (e.g.
FVIII or Warfarin ® ¯2,7,9,10) or Inhibition (e.g. aspirin, heparin)
Related Topics