Chapter: Biology of Disease: Transfusion and Transplantation
Laboratory Determination of Blood Groups
LABORATORY DETERMINATION OF BLOOD
GROUPS
Traditional methods for determining blood groups rely
on the agglutina-tion of erythrocytes by antibodies, usually referred to as
hemagglutination. Hemagglutination can be carried out on glass microscopy
slides or in micro-titer plates in which agglutination patterns are easily
distinguished from the settling of erythrocytes. Recent years have seen
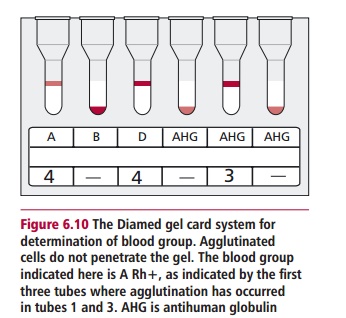
increasing use of the Diamed typing system to detect hemagglutination. This is
a system which uses mono-clonal typing antibodies, distributed in a gel,
contained in individual tubes set in plastic ‘cards’. Cells are added to the
antibodies and the cards are cen-trifuged. Where agglutination has occurred,
the agglutinates remain on top of the gel, whereas nonagglutinated cells settle
through the gel to the bottom (Figure
6.10). Most transfusion laboratories now use gel technology for blood
grouping and compatibility testing.
Whichever technique is used, a blood group, such as
the ABO grouping, is determined by incubating the individual’s erythrocytes
with antibodies to known antigens (anti-A and anti-B in this case) and also
mixing the indi-vidual’s plasma with erythrocytes of known A, B, AB or O blood
groups. The pattern of hemagglutination shown will enable the determination of
the blood group.
Hemagglutination
occurs when antibodies to an erythrocyte antigen cross-link the cells, forming
visible aggregates. The extent of hemagglutination depends on the temperature,
pH and the ionic strength of the medium. Agglutination is favored in low ionic
strength saline (LISS). Erythrocytes have a net electronegative charge and
repulsive forces normally keep them about 20 nm apart. When antibodies bind to
the erythrocyte, the reduced surface charge allows the cells to agglutinate.
This is most effectively achieved with IgM antibodies, which can cause direct
agglutination of erythrocytes. To obtain a direct agglutination with IgG
antibodies, it is usually necessary to include bovine serum albumin in the
medium, which masks the charges on the erythrocytes and allows them to come
closer together. Another method of reducing the negative charge is to use
proteolytic enzymes to remove sur-face proteins that carry the charge. The
enzyme can be added to the eryth-rocytes prior to the addition of the antibody,
or all the components can be added together. Polycationic polymers such as
polybrene will also reduce the negative charge on erythrocytes.
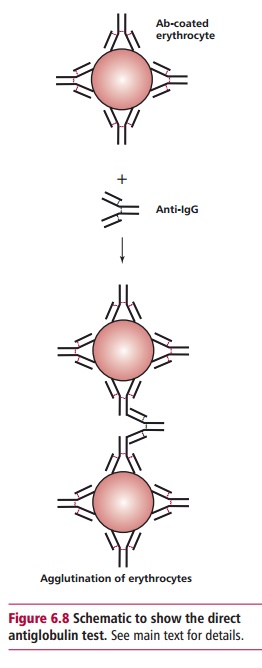
The antiglobulin test
uses the ability of antihuman globulin (AHG) to agglutinate erythrocytes
coated with nonagglutinating erythrocyte-specific IgG. This can be used to
detect erythrocytes already coated with anti-erythrocyte IgG in the direct
antiglobulin test (DAT), or can be used on cells which have been incubated with
antibody in vitro (see Figure 6.8).
Related Topics