Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Management of Patients with Fluid & Electrolyte Disturbances
Hypocalcemia
HYPOCALCEMIA
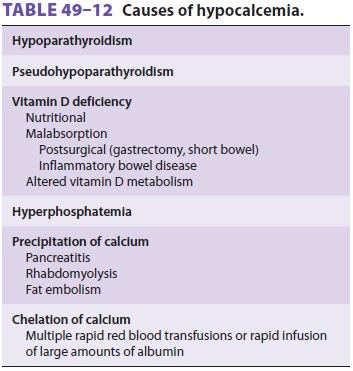
Hypocalcemia should be diagnosed only on the basis of the plasma ionized
calcium concentration. When direct measurements of plasma [Ca2+] are not available, the total
calcium concentration must be corrected for decreases in plasma albumin
concen-tration (see above). The causes of hypocalcemia are listed in Table
49–12.
Hypocalcemia due to hypoparathyroidism is a relatively common cause of
symptomatic hypocal-cemia. Hypoparathyroidism may be surgical, idio-pathic,
part of multiple endocrine defects (most often with adrenal insufficiency), or
associated with hypomagnesemia. Magnesium deficiency may impair the secretion
of PTH and antagonize the effects of PTH on bone. Hypocalcemia during sep-sis
is also thought to be due to suppression of PTH release. Hyperphosphatemia is also a relatively common cause of
hypocalcemia, particu-larly in patients with chronic renal failure.
Hypo-calcemia due to vitamin D deficiency may be the result of a markedly
reduced intake (nutritional), vitamin D malabsorption, or abnormal vitamin D
metabolism.
Chelation of calcium ions with the citrate ions in blood preservatives
is an important cause of perioperative hypocalcemia in transfused patients;
similar transient decreases in [Ca 2+] are also pos-sible following
rapid infusions of large volumes of albumin. Hypocalcemia following acute
pancreati-tis is thought to be due to precipitation of calcium with fats
(soaps) following the release of lipolytic enzymes and fat necrosis;
hypocalcemia following fat embolism may have a similar basis. Precipitation of
calcium (in injured muscle) may also be seen fol-lowing rhabdomyolysis.
Less common causes of hypocalcemia include calcitonin-secreting
medullary carcinomas of the thyroid, osteoblastic metastatic disease (breast
and prostate cancer), and pseudohypoparathyroidism (familial unresponsiveness
to PTH). Transient hypo-calcemia may be seen following heparin, protamine, or
glucagon administration.
Clinical Manifestations of Hypocalcemia
Manifestations of hypocalcemia include
paresthe-sias, confusion, laryngeal stridor (laryngospasm), carpopedal spasm
(Trousseau’s sign), masseter spasm (Chvostek’s sign), and seizures. Biliary
colic and bronchospasm have also been described. ECG may reveal cardiac
irritability or QT interval pro-longation, which may not correlate in severity
with the degree of hypocalcemia. Decreased cardiac con-tractility may result in
heart failure, hypotension,or both. Decreased responsiveness to digoxin and
β-adrenergic agonists may also occur.
Treatment of Hypocalcemia
Symptomatic hypocalcemia is a medical
emer-gency and should be treated immediately withintravenous calcium chloride
(3–5 mL of a 10% solu-tion) or calcium gluconate (10–20 mL of a 10% solu-tion).
(Ten milliliters of 10% CaCl 2 contains 272 mg of Ca2+, whereas 10 mL of 10%
calcium gluconate contains only 93 mg of Ca2+.) To avoid
precipita-tion, intravenous calcium should not be given with bicarbonate- or
phosphate-containing solutions. Serial ionized calcium measurements are
manda-tory. Repeat boluses or a continuous infusion (Ca 2+ 1–2 mg/kg/h) may be necessary. Plasma magnesium concentration should be
checked to exclude hypo-magnesemia. In chronic hypocalcemia, oral calcium (CaCO3) and vitamin D replacement are usually
necessary.
Anesthetic Considerations
Significant hypocalcemia should be corrected
pre-operatively. Serial ionized calcium levels should be monitored
intraoperatively in patients with a his-tory of hypocalcemia. Alkalosis should
be avoided to prevent further decreases in [Ca2+]. Intravenous cal-cium
may be necessary following rapid transfusions of citrated blood products or
large volumes of albu-min solutions. Potentiation of the negative inotropic
effects of barbiturates and volatile anesthetics should be expected. Responses to
NMBs are inconsistent and require close monitoring with a nerve stimulator.
Related Topics