Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Management of Patients with Fluid & Electrolyte Disturbances
Disorders of Water Balance: Hypoosmolality & Hyponatremia
HYPOOSMOLALITY & HYPONATREMIA
Hypoosmolality is nearly always associated with hyponatremia ([Na+] < 135 mEq/L). Table 49–5 lists rare instances in which
hyponatremia does not necessarily reflect hypoosmolality (pseudo-hyponatremia). Routine measurement of plasma
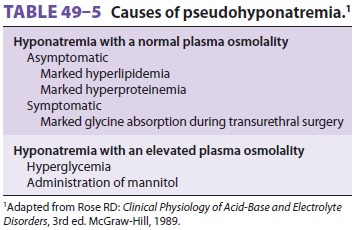
osmolality in hyponatremic patients rapidly excludes pseudohyponatremia.
Hyponatremia invariably reflects water
reten-tion from either an absolute increase in TBW or a loss of sodium in
relative excess to loss of water. The kidneys’ normal capacity to produce
dilute urine with an osmolality as low as 40 mOsm/kg (specific gravity 1.001)
allows them to excrete over 10 L of free water per day if necessary. Because of
this tre-mendous reserve, hyponatremia is nearly always the result of a defect
in urinary diluting capacity (urinary osmolality > 100 mOsm/kg or specific gravity > 1.003). Rare instances of hyponatremia without an abnormality in renal
diluting capacity (urinary osmolality < 100 mOsm/kg) are generally attributed to primary polydipsia or reset
osmorecep-tors; the latter two conditions can be differentiated by water
restriction.
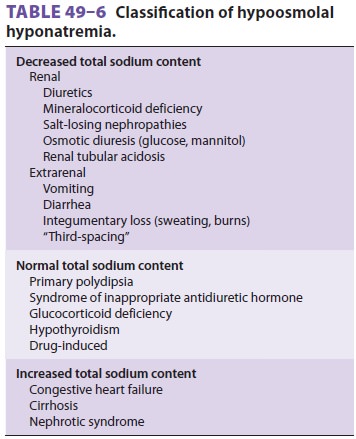
Clinically, hyponatremia is best classified
accord-ing to total body sodium content (Table 49–6).
Hyponatremia &Low Total Body Sodium
Progressive losses of both sodium and water even-tually lead to extracellular volume depletion. As the intravascular volume deficit reaches 5–10%, non-osmotic ADH secretion is activated (see above). With further volume depletion, the stimuli for nonosmotic ADH release overcome any hypona-tremia-induced suppression of ADH. Preservation of circulatory volume takes place at the expense of plasma osmolality.
Fluid losses resulting in hyponatremia may be renal or extrarenal in origin.
Renal losses are most commonly related to thiazide diuretics and result in a
urinary [Na+] greater
than 20 mEq/L. Extrare-nal losses are typically gastrointestinal and usually
produce a urinary [Na+] of less
than 10 mEq/L. A major exception to the latter is hyponatremia due to vomiting,
which can result in a urinary [Na+] greater than 20 mEq/L. In those
instances, bicar-bonaturia from the associated metabolic alkalosis obligates
concomitant excretion of Na + with HCO 3 to
maintain electrical neutrality in the urine; urinary chloride concentration,
however, is usually less than 10 mEq/L.
Hyponatremia & Increased Total Body Sodium
Edematous disorders are characterized by an
increase in both total body sodium and TBW. When the increase in water exceeds
that in sodium, hypo-natremia occurs. Edematous disorders include con-gestive
heart failure, cirrhosis, kidney failure, and nephrotic syndrome. Hyponatremia
in these set-tings results from progressive impairment of renal free water
excretion and generally parallels underly-ing disease severity.
Pathophysiological mechanisms include nonosmotic ADH release and decreased
delivery of fluid to the distal diluting segment in nephrons . The “effective”
circulat-ing blood volume is reduced.
Hyponatremia with Normal Total Body Sodium
Hyponatremia in the absence of edema or
hypovo-lemia may be seen with glucocorticoid insufficiency, hypothyroidism,
drug therapy (chlorpropamide and cyclophosphamide), and the syndrome of
inap-propriate antidiuretic hormone secretion (SIADH). The hyponatremia
associated with adrenal hypo-function may be due to cosecretion of ADH with
corticotropin-releasing factor (CRF). Diagnosis of SIADH requires exclusion of
other causes of hypo-natremia and the absence of hypovolemia, edema, and adrenal,
renal, or thyroid disease. Various malignant tumors, pulmonary diseases, and
central nervous system disorders are commonly associated with SIADH. In most
such instances, plasma ADH concentration is not elevated but is inadequately
suppressed relative to the degree of hypoosmolality in plasma; urine osmolality
is usually greater than 100 mOsm/kg and urine sodium concentration is greater
than 40 mEq/L.
Clinical Manifestations of Hyponatremia
Symptoms of hyponatremia are primarily neuro-logical and result from an increase in intracellular water. Their severity is generally related to the rapid-ity with which extracellular hypoosmolality devel-ops. Patients with mild to moderate hyponatremia ([Na+] > 125 mEq/L) are frequently asymptomatic. Early symptoms are typically nonspecific and may include anorexia, nausea, and weakness. Pro-gressive cerebral edema, however, results in leth-argy, confusion, seizures, coma, and finally death.Serious manifestations of hyponatremia are generally associated with plasma sodium concentrations less than 120 mEq/L. Compared with men, premenopausal women appear to be at greater risk of neurological impairment and damage from hyponatremia.
Patients with slowly developing or chronic
hyponatremia are generally less symptomatic, prob-ably because the gradual
compensatory loss of intra-cellular solutes (primarily Na +, K+, and amino acids)
restores cell volume to near normal. Neurological symptoms in patients with
chronic hyponatremia may be related more closely to changes in cell mem-brane
potential (due to a low extracellular [Na +]) than to changes in
cell volume.
Treatment of Hyponatremia
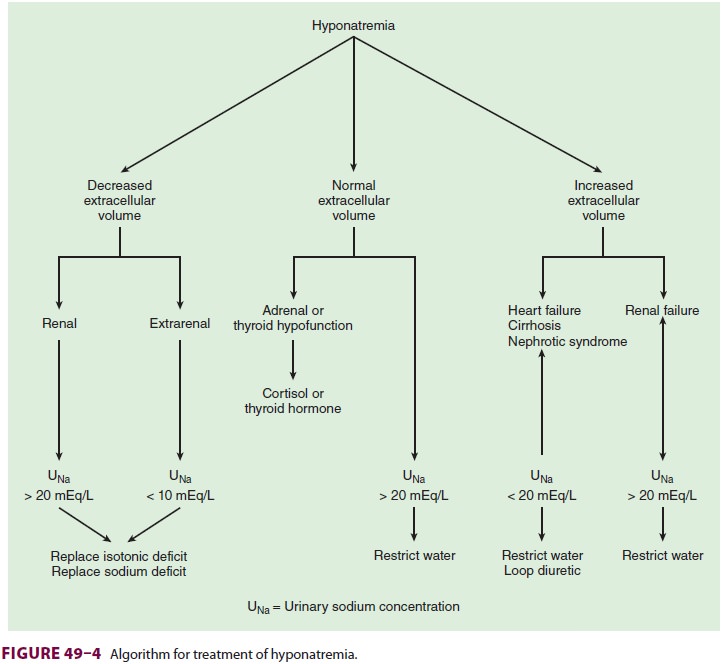
As with hypernatremia, the treatment of
hypona-tremia (Figure
49–4) is directed at correcting both the underlying disorder as well as the
plasma [Na+].Isotonic saline is
generally the treatment of choice for hyponatremic patients with decreased
total body sodium content. Once the ECF deficit is cor-rected, spontaneous
water diuresis returns plasma [Na+] to normal. Conversely, water
restriction is the primary treatment for hyponatremic patients with normal or
increased total body sodium. Morespecific treatments such as hormone
replacement in patients with adrenal or thyroid hypofunction and measures aimed
at improving cardiac output in patients with heart failure may also be
indicated. Demeclocycline, a drug that antagonizes ADH activity at the renal
tubules, has proved to be a use-ful adjunct to water restriction in the
treatment of patients with SIADH.
Acute
symptomatic hyponatremia requires prompt treatment. In such instances,
correction of plasma [Na+] to greater than 125 mEq/L is
usu-ally sufficient to alleviate symptoms. The amount of NaCl necessary to
raise plasma [Na+] to the desired value, the Na+ deficit, can be estimated by the follow-ing formula:
Na+ deficit = TBW × (desired [Na+] − present [Na+])
Excessively
rapid correction of hyponatre-mia has been associated with demyelinating
lesions in the pons (central pontine
myelinolysis), resulting in permanent neurological sequelae. The rapidity
with which hyponatremia is corrected should be tailored to the severity of
symptoms. The following correction rates have been suggested: for mild
symptoms, 0.5 mEq/L/h or less; for moderate symptoms, 1 mEq/L/h or less; and
for severe symp-toms, 1.5 mEq/L/h or less.
Example
An 80-kg
woman is lethargic and is found to have plasma [Na+] of 118 mEq/L. How much NaCl must be
given to raise her plasma [Na+] to 130 mEq/L?
Na+ deficit = TBW × (130 − 118)
TBW is
approximately 50% of body weight in females:
Na+ deficit = 80 × 0.5 × (130 − 118) = 480 mEq
Because normal (isotonic) saline contains154
mEq/L, the patient should receive 480 mEq ÷ 154 mEq/L, or 3.12 L of normal
saline. For a cor-rection rate of 0.5 mEq/L/h, this amount of saline should be
given over 24 h (130 mL/h).
Note that this calculation does not take into
account any coexisting isotonic fluid deficits, which, if present, should also
be replaced. More rapid cor-rection of hyponatremia can be achieved by giving a
loop diuretic to induce water diuresis while replacing urinary Na+ losses with isotonic saline. Even
more rapid corrections can be achieved with intravenous hypertonic saline (3%
NaCl). Hypertonic saline may be indicated in markedly symptomatic patients with
plasma [Na+] less than 110 mEq/L. Three percent
NaCl should be given cautiously as it can precipi-tate pulmonary edema,
hypokalemia, hyperchlore-mic metabolic acidosis, and transient hypotension;
bleeding has been associated with prolongation of the prothrombin time and
activated partial throm-boplastin time.
Anesthetic Considerations
Hyponatremia is often a manifestation of a
serious underlying disorder and requires careful preop-erative evaluation. A
plasma sodium concentration greater than 130 mEq/L is usually considered safe
for patients undergoing general anesthesia. In most circumstances, plasma [Na+] should be corrected to
greater than 130 mEq/L for elective procedures, even in the absence of
neurological symptoms. Lower concentrations may result in significant cere-bral
edema that can be manifested intraoperatively as a decrease in minimum alveolar
concentration or postoperatively as agitation, confusion, or somno-lence.
Patients undergoing transurethral resection of the prostate can absorb signì
cant amounts of water from irrigation fluids (as much as 20 mL/min) and are at
high risk for rapid development of pro-found acute water intoxication.
Related Topics