Chapter: Clinical Anesthesiology: Perioperative & Critical Care Medicine: Management of Patients with Fluid & Electrolyte Disturbances
Hypercalcemia
HYPERCALCEMIA
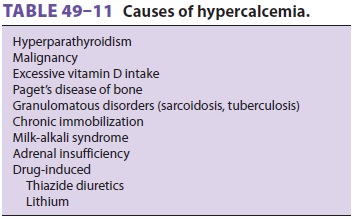
Hypercalcemia can occur as a result of a vari-ety of disorders (Table
49–11). In primary hyper-parathyroidism,
secretion of PTH is increased andis independent of [Ca2+]. In contrast, in second-ary hyperparathyroidism (chronic
renal failureor malabsorption), the elevated PTH levels are in response to
chronic hypocalcemia. Prolonged sec-ondary hyperparathyroidism, however, can
occa-sionally result in autonomous secretion of PTH, resulting in a normal or
elevated [Ca 2+] (tertiaryhyperparathyroidism).
Patients with cancer can present with
hypercal-cemia whether or not bone metastases are present. Most often this is
due to direct bony destruction, or secretion of humoral mediators of
hypercalcemia (PTH-like substances, cytokines, or prostaglandins), or both.
Hypercalcemia due to increased turnover of calcium from bone can also be
encountered in patients with benign conditions such as Paget’s disease and
chronic immobilization. Increased gastrointestinal absorption of calcium can
lead to hypercalcemia in patients with the milk-alkali syn-drome (marked
increase in calcium intake), hypervi-taminosis D, or granulomatous diseases
(enhanced sensitivity to vitamin D).
Clinical Manifestations of Hypercalcemia
Hypercalcemia often produces anorexia, nausea, vomiting, weakness, and
polyuria. Ataxia, irritabil-ity, lethargy, or confusion can rapidly progress to
coma. Hypertension is often present initially before hypovolemia supervenes.
ECG signs include a shortened ST segment and a shortened QT interval.
Hypercalcemia increases cardiac sensitivity to digi-talis. Pancreatitis, peptic
ulcer disease, and kidney failure may also complicate hypercalcemia.
Treatment of Hypercalcemia
Symptomatic hypercalcemia requires rapid
treatment. The most effective initial treatmentis rehydration followed by a
brisk diuresis (urinary output 200–300 mL/h) utilizing intravenous saline
infusion and a loop diuretic to accelerate calcium excretion. Premature
diuretic therapy prior to rehy-dration may aggravate the hypercalcemia by
exac-erbating volume depletion. Renal loss of potassium and magnesium usually
occurs during diuresis, and laboratory monitoring and intravenous replacement
as necessary should be performed. Although hydra-tion and diuresis may remove
the potential risk of cardiovascular and neurological complications of
hypercalcemia, the serum calcium level usually remains elevated above normal.
Additional therapy with a bisphosphonate or calcitonin may be required to
further lower the serum calcium level. Severe hypercalcemia (>15 mg/dL) usually
requires addi-tional therapy after saline hydration and furosemide calciuresis.
Bisphosphonates or calcitonin are pre-ferred agents. Intravenous administration
of pami-dronate (Aredia) or etidronate (Didronel) is often utilized in this setting.
Dialysis is very effective in correcting severe hypercalcemia and may be
neces-sary in the presence of kidney or heart failure. Addi-tional treatment
depends on the underlying cause of the hypercalcemia and may include
glucocorticoids in the setting of vitamin D–induced hypercalcemia such as
granulomatous disease states.
It is necessary to look for the underlying
eti-ology and direct appropriate treatment toward the cause of the
hypercalcemia once the initial threat of hypercalcemia has been removed.
Approximately 90% of all hypercalcemia is due to either malignancy or
hyperparathyroidism. The best laboratory test for discriminating between these
two main categories of hypercalcemia is the PTH assay. The serum PTH
concentration is usually suppressed in malignancy states and elevated in
hyperparathyroidism.
Anesthetic Considerations
Significant
hypercalcemia is a medical emergency and should be corrected, if possible,
before admin-istration of any anesthetic. Ionized calcium levels should be
monitored closely. If surgery must be performed, saline diuresis should be
continued intraoperatively with care to avoid hypovolemia; appropriate
goal-directed hemodynamic and fluid management therapy should be utilized, especially for patients
with cardiac impair-ment. Serial measurements of [K+] and [Mg2+] are helpful in detecting iatrogenic
hypokalemia and hypomagnesemia. Responses to anesthetic agents are not
predictable. Ventilation should be controlled under general anesthesia.
Acidosis should be avoided so as to not worsen the elevated plasma [Ca2+].
Related Topics