Chapter: Medicine and surgery: Haematology and clinical Immunology
Hypersensitivity reactions - Allergy
Allergy
Hypersensitivity reactions
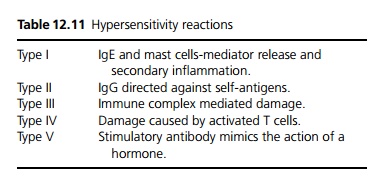
There are five basic types of hypersensitivity reactions (see Table 12.11)
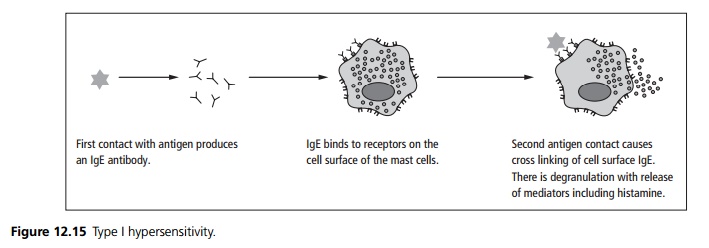
Type I hypersensitivity (allergy)
On the first encounter with an antigen IgE antibodies are formed. These bind to a receptor on the surface of mast cells. On subsequent contacts with the antigen there is cross-linking of IgE on the mast cells which triggers them to degranulate releasing histamine and other preformed mediators (see Fig. 12.15). The reaction also triggers arachadonic acid metabolism leading to the production of leukotrienes, prostaglandins, prostacyclins and thromboxane. The clinical reaction is characterised by vasodilation, bronchoconstriction, and localised tissue oedema (see also anaphylaxis page 499).
Type II hypersensitivity (antibody dependent cytotoxic hypersensitivity)
Type II hypersensitivity is mediated by antibodies, these may be directed at:
A normal ‘self ’ antigen, e.g. Goodpasture syndrome, myasthenia gravis, or autoimmune haemolytic anaemia.
A novel self-antigen may also become immunogenic e.g. α methyldopa (an antihypertensive) causes haemolysis by altering the cell membrane of red blood cells resulting in the expression of a red cell hidden antigen.
Alternatively either the antibody (e.g. haemolytic disease of the newborn) or the antigen (e.g. transfusion
reactions) may be foreign.
The cell becomes coated (opsonised) with antibody, which then activates the complement system leading to local tissue damage. An antibody coated target is also open to attack by phagocytes and killer cells (antibody dependent cellular cytotoxicity or ADCC).
Type III hypersensitivity (immune complexes)
Immune complexes are formed of antibodies bound to antigens. These are normally cleared from the tissues and the circulation. If they persist they result in local inflammation, cell accumulation, complement fixation and cellular damage. Immune complex mediated hypersensitivity can be divided into:
· External systemic which manifests as serum sickness, in which there is immune complex formation within the circulation, then tissue deposition resulting in local inflammation, cell accumulation, complement fixation and damage. Other examples include penicillin allergy and infective endocarditis.
· External local such as extrinsic allergic alveolitis in which there is local IgG production and cellular infiltration within the lung.
· Endogenous such as systemic lupus erythematosus and rheumatoid arthritis.
Type IV hypersensitivity (T cell mediated delayed type hypersensitivity)
This type of hypersensitivity reaction occurs when an antigen interacts with antigenspecific CD8 cytotoxic and CD4 helper T-cells. This results in the release pro inflammatory cytokines and causes the recruitment of multiple cells amplifying a small specific response into a large non-specific reaction. This is the basis of granuloma formation. Examples of type IV hypersensitivity include:
· Contact hypersensitivity: An epidermal reaction at the site of contact with the antigen often elicited by small molecules called haptens. Exposure to an agent such as nickel through the skin results in sensitisation of CD4+ T cells. Re-exposure to nickel results in T cell activation, activation of macrophages and release of local cytokines.
· Tuberculin hypersensitivity in which soluble antigens from mycobacteria administered subcutaneously results in fever, general unwellness, and an area of red, hard swelling at the site of injection.
Type V stimulatory
In type V hypersensitivity reactions an autoantibody is directly stimulatory via a target receptor. An example of this class is the antibody to the TSH receptor seen in Grave’s disease, which stimulates the thyroid gland causing hyperthyroidism.
Related Topics