Chapter: Basic & Clinical Pharmacology : Drugs Used in the Treatment of Gastrointestinal Diseases
H2-Receptor Antagonists - Agents that Reduce Intragastric Acidity
H2-RECEPTOR
ANTAGONISTS
From
their introduction in the 1970s until the early 1990s, H2-receptor
antagonists (commonly referred to as H2
blockers) were the most commonly prescribed drugs in the world (see Clinical
Uses). With the recognition of the role of H
pylori in ulcer disease (which may be treated with appropriate
antibacterial therapy) and the advent of proton pump inhibitors, the use of
prescription H2 blockers has declined markedly.
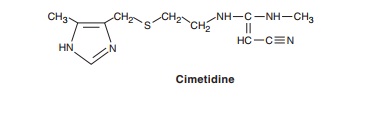
Chemistry & Pharmacokinetics
Four H2 antagonists are in
clinical use: cimetidine, ranitidine, famo-tidine, and nizatidine. All four
agents are rapidly absorbed from the intestine. Cimetidine, ranitidine, and
famotidine undergo first-pass hepatic metabolism resulting in a bioavailability
of approximately 50%. Nizatidine has little first-pass metabolism. The serum
half-lives of the four agents range from 1.1 to 4 hours; however, dura-tion of
action depends on the dose given (Table 62–1). H2 antagonists are cleared by a combination of
hepatic metabolism, glomerular filtration, and renal tubular secretion. Dose
reduction is required in patients with moderate to severe renal (and possibly
severe hepatic) insufficiency. In the elderly, there is a decline of up to 50%
in drug clearance as well as a significant reduction in vol-ume of
distribution.
Pharmacodynamics
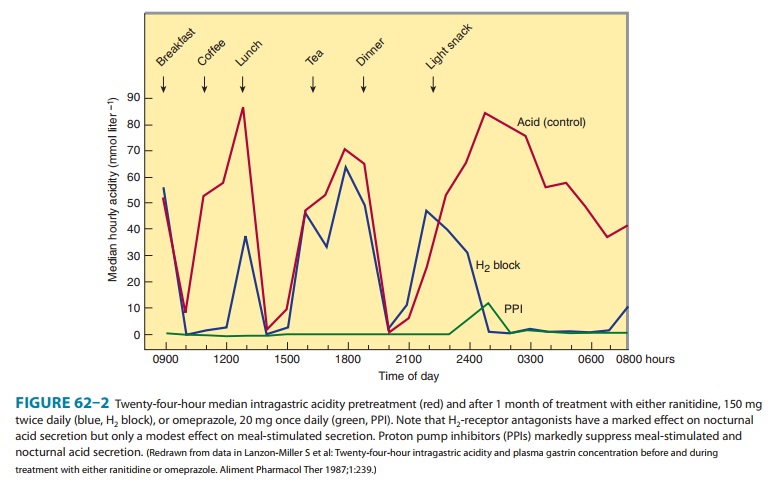
The
H2 antagonists exhibit competitive
inhibition at the parietal cell H2
receptor and suppress basal and meal-stimulated acid secretion (Figure 62–2) in
a linear, dose-dependent manner. They are highly selective and do not affect H1
or H3 receptors . The volume of gastric
secretion and the concentra-tion of pepsin are also reduced.
H2
antagonists reduce acid secretion stimulated by histamine as well as by gastrin
and cholinomimetic agents through two mechanisms. First, histamine released
from ECL cells by gastrin or vagal stimulation is blocked from binding to the
parietal cell H2 receptor. Second, direct
stimulation of the parietal cell by gastrin or acetylcholine has a diminished
effect on acid secretion in the presence of H2-receptor
blockade.
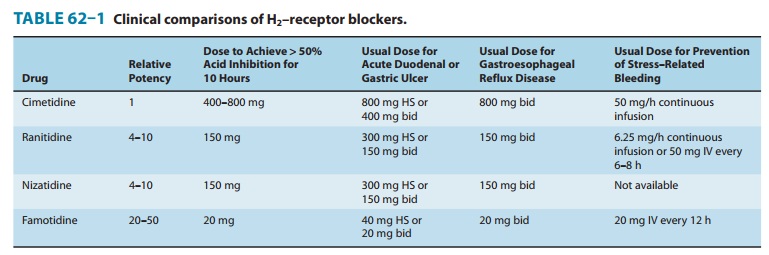
The potencies of the
four H2-receptor antagonists
vary over a 50-fold range (Table 62–1). When given in usual prescription doses
however, all inhibit 60–70% of total 24-hour acid secretion. H2 antagonists are
especially effective at inhibiting nocturnal acid secretion (which depends
largely on histamine), but they have a modest impact on meal-stimulated acid
secretion (which is stimu-lated by gastrin and acetylcholine as well as
histamine). Therefore, nocturnal and fasting intragastric pH is raised to 4–5
but the impact on the daytime, meal-stimulated pH profile is less. Recommended
prescription doses maintain greater than 50% acid inhibition for 10 hours;
hence, these drugs are commonly given twice daily. At doses available in
over-the-counter formulations, the duration of acid inhibition is less than 6
hours.
Clinical Uses
H2-receptor antagonists
continue to be prescribed but proton pump inhibitors are steadily replacing H2 antagonists for most
clinical indications. However, the over-the-counter preparations of the H2 antagonists are
heavily used by the public.
A. Gastroesophageal Reflux Disease (GERD)
Patients
with infrequent heartburn or dyspepsia (fewer than 3 times per week) may take
either antacids or intermittent H2
antagonists. Because antacids provide rapid acid neutralization, they afford
faster symptom relief than H2
antagonists. However, the effect of antacids is short-lived (1–2 hours)
compared with H2 antagonists (6–10 hours). H2
antagonists may be taken prophylac-tically before meals in an effort to reduce
the likelihood of heart-burn. Frequent heartburn is better treated with
twice-daily H2 antagonists (Table 62–1) or proton
pump inhibitors. In patients with erosive esophagitis (approximately 50% of
patients with GERD), H2
antagonists afford healing in less than 50% of patients; hence proton pump
inhibitors are preferred because of their superior acid inhibition.
B. Peptic Ulcer Disease
Proton pump inhibitors
have largely replaced H2 antagonists in the treatment of acute peptic ulcer disease.
Nevertheless, H2 antagonists are still
sometimes used. Nocturnal acid suppression by H2 antagonists affords effective ulcer healing
in most patients
Pharmacodynamics
The H2
antagonists exhibit competitive inhibition at the parietal cell H2
receptor and suppress basal and meal-stimulated acid secretion (Figure 62–2) in
a linear, dose-dependent manner. They are highly selective and do not affect H1
or H3 receptors . The volume of gastric
secretion and the concentra-tion of pepsin are also reduced.
H2
antagonists reduce acid secretion stimulated by histamine as well as by gastrin
and cholinomimetic agents through two mechanisms. First, histamine released
from ECL cells by gastrin or vagal stimulation is blocked from binding to the
parietal cell H2 receptor. Second, direct
stimulation of the parietal cell by gastrin or acetylcholine has a diminished
effect on acid secretion in the presence of H2-receptor
blockade.
The
potencies of the four H2-receptor
antagonists vary over a 50-fold range (Table 62–1). When given in usual
prescription doses however, all inhibit 60–70% of total 24-hour acid secretion.
H2 antagonists are especially
effective at inhibiting nocturnal acid secretion (which depends largely on
histamine), but they have a modest impact on meal-stimulated acid secretion
(which is stimu-lated by gastrin and acetylcholine as well as histamine).
Therefore, nocturnal and fasting intragastric pH is raised to 4–5 but the
impact on the daytime, meal-stimulated pH profile is less. Recommended
prescription doses maintain greater than 50% acid inhibition for 10 hours;
hence, these drugs are commonly given twice daily. At doses available in
over-the-counter formulations, the duration of acid inhibition is less than 6
hours.
Clinical Uses
H2-receptor antagonists continue to be
prescribed but proton pump inhibitors
are steadily replacing H2 antagonists for most clinical indications. However, the
over-the-counter preparations of the H2 antagonists are heavily used by the public.
A. Gastroesophageal Reflux Disease (GERD)
Patients
with infrequent heartburn or dyspepsia (fewer than 3 times per week) may take
either antacids or intermittent H2
antagonists. Because antacids provide rapid acid neutralization, they afford
faster symptom relief than H2
antagonists. However, the effect of antacids is short-lived (1–2 hours)
compared with H2 antagonists (6–10 hours). H2
antagonists may be taken prophylac-tically before meals in an effort to reduce
the likelihood of heart-burn. Frequent heartburn is better treated with
twice-daily H2 antagonists (Table 62–1) or proton
pump inhibitors. In patients with erosive esophagitis (approximately 50% of
patients with GERD), H2
antagonists afford healing in less than 50% of patients; hence proton pump
inhibitors are preferred because of their superior acid inhibition.
B. Peptic Ulcer Disease
Proton pump inhibitors have largely replaced H2 antagonists in the treatment of acute peptic ulcer disease. Nevertheless, H2 antagonists are still sometimes used. Nocturnal acid suppression by H2 antagonists affords effective ulcer healing in most patients with uncomplicated gastric and duodenal ulcers. Hence, all the agents may be administered once daily at bedtime, resulting in ulcer healing rates of more than 80–90% after 6–8 weeks of therapy. For patients with ulcers caused by aspirin or other NSAIDs, the NSAID should be discontinued. If the NSAID must be continued for clinical reasons despite active ulceration, a pro-ton pump inhibitor should be given instead of an H2 antagonist to more reliably promote ulcer healing. For patients with acute peptic ulcers caused by H pylori, H2 antagonists no longer play a significant therapeutic role. H pylori should be treated with a 10-to 14-day course of therapy including a proton pump inhibitor and two antibiotics . This regimen achieves ulcer heal-ing and eradication of the infection in more than 90% of patients. For the minority of patients in whom H pylori cannot be success-fully eradicated, H2 antagonists may be given daily at bedtime in half of the usual ulcer therapeutic dose to prevent ulcer recurrence (eg, ranitidine, 150 mg; famotidine, 20 mg).
C. Nonulcer Dyspepsia
H2 antagonists are commonly used as
over-the-counter agents and prescription agents for treatment of intermittent
dyspepsia not caused by peptic ulcer. However, benefit compared with placebo
has never been convincingly demonstrated.
D. Prevention of Bleeding from Stress-Related Gastritis
Clinically important bleeding from upper
gastrointestinal erosions or ulcers occurs in 1–5% of critically ill patients
as a result of impaired mucosal defense mechanisms caused by poor perfusion.
Although most critically ill patients have normal or decreased acid secretion,
numerous studies have shown that agents that increase intragastric pH (H2 antagonists or proton
pump inhibitors) reduce the incidence of clinically significant bleeding.
However, the opti-mal agent is uncertain at this time. For patients without a
nasoen-teric tube or with significant ileus, intravenous H2 antagonists are
preferable over intravenous proton pump inhibitors because of their proven
efficacy and lower cost. Continuous infusions of H2 antagonists are generally preferred to bolus
infusions because they achieve more consistent, sustained elevation of
intragastric pH.
Adverse Effects
H2 antagonists are extremely safe drugs. Adverse
effects occur in less than 3% of patients and include diarrhea, headache,
fatigue, myalgias, and constipation. Some studies suggest that intravenous H2 antagonists (or
proton pump inhibitors) may increase the risk of nosocomial pneumonia in
critically ill patients.
Mental status changes (confusion,
hallucinations, agitation) may occur with administration of intravenous H2 antagonists,
especially in patients in the intensive care unit who are elderly or who have
renal or hepatic dysfunction. These events may be more common with cimetidine.
Mental status changes rarely occur in ambulatory patients.
Cimetidine inhibits binding of
dihydrotestosterone to andro-gen receptors, inhibits metabolism of estradiol,
and increases serum prolactin levels. When used long-term or in high doses, it
may cause gynecomastia or impotence in men and galactorrhea in women. These
effects are specific to cimetidine and do not occur with the other H2 antagonists.
Although there are no known harmful effects on
the fetus, H2 antagonists cross the
placenta. Therefore, they should not be administered to pregnant women unless
absolutely necessary. The H2 antagonists are secreted into breast milk and may therefore
affect nursing infants.
H2 antagonists may rarely cause blood
dyscrasias. Blockade of cardiac H2 receptors may cause bradycardia, but this is rarely of clinical
significance. Rapid intravenous infusion may cause brady-cardia and hypotension
through blockade of cardiac H2 receptors; therefore, intravenous injections should be given
over 30 minutes. H2 antagonists rarely cause reversible abnormalities in liver
chemistry.
Drug Interactions
Cimetidine interferes with several important
hepatic cytochrome P450 drug metabolism pathways, including those catalyzed by
CYP1A2, CYP2C9, CYP2D6, and CYP3A4 . Hence, the half-lives of drugs metabolized
by these pathways may be prolonged. Ranitidine binds 4–10 times less avidly
than cime-tidine to cytochrome P450. Negligible interaction occurs with
nizatidine and famotidine.
H2 antagonists compete with creatinine and
certain drugs (eg, procainamide) for renal tubular secretion. All of these
agents except famotidine inhibit gastric first-pass metabolism of ethanol,
especially in women. Although the importance of this is debated, increased
bioavailability of ethanol could lead to increased blood ethanol levels.
Related Topics