Chapter: Basic & Clinical Pharmacology : Drugs Used in the Treatment of Gastrointestinal Diseases
Drugs Used in the Treatment of Irritable Bowel Syndrome
DRUGS USED IN THE TREATMENT OF
IRRITABLE BOWEL SYNDROME
IBS is an idiopathic
chronic, relapsing disorder characterized by abdominal discomfort (pain,
bloating, distention, or cramps) in association with alterations in bowel
habits (diarrhea, constipa-tion, or both). With episodes of abdominal pain or
discomfort, patients note a change in the frequency or consistency of their
bowel movements.
Pharmacologic
therapies for IBS are directed at relieving abdominal pain and discomfort and
improving bowel function.
For
patients with predominant diarrhea, antidiarrheal agents, especially
loperamide, are helpful in reducing stool frequency and fecal urgency. For
patients with predominant constipation, fiber supplements may lead to softening
of stools and reduced straining; however, increased gas production may
exacerbate bloating and abdominal discomfort. Consequently, osmotic laxatives,
especially milk of magnesia, are commonly used to soften stools and pro-mote
increased stool frequency.
For chronic abdominal
pain, low doses of tricyclic antidepres-sants (eg, amitriptyline or
desipramine, 10–50 mg/d) appear to be helpful . At these doses, these agents
have no effect on mood but may alter central processing of visceral afferent
information. The anticholinergic properties of these agents also may have
effects on gastrointestinal motility and secretion, reduc-ing stool frequency
and liquidity. Finally, tricyclic antidepressants may alter receptors for
enteric neurotransmitters such as sero-tonin, affecting visceral afferent
sensation.
Several other agents
are available that are specifically intended for the treatment of IBS.
ANTISPASMODICS (ANTICHOLINERGICS)
Some agents are promoted
as providing relief of abdominal pain or discomfort through antispasmodic
actions. However, small or large bowel spasm has not been found to be an
important cause of symptoms in patients with IBS. Antispasmodics work primarily
through anticholinergic activities. Commonly used medications in this class
include dicyclomine and hyoscyamine . These drugs inhibit
muscarinic cholinergic receptors in the enteric plexus and on smooth muscle.
The efficacy of antispasmodics for relief of abdominal symptoms has never been
convincingly dem-onstrated. At low doses, they have minimal autonomic effects.
However, at higher doses they exhibit significant additional anti-cholinergic
effects, including dry mouth, visual disturbances, uri-nary retention, and
constipation. For these reasons, antispasmodics are infrequently used.
SEROTONIN 5-HT3-RECEPTOR ANTAGONISTS
5-HT3
receptors in the gastrointestinal tract activate visceral affer-ent pain
sensation via extrinsic sensory neurons from the gut to the spinal cord and
central nervous system. Inhibition of afferent gastrointestinal 5-HT3
receptors may reduce unpleasant visceral afferent sensation, including nausea,
bloating, and pain. Blockade of central 5-HT3
receptors also reduces the central response to visceral afferent stimulation.
In addition, 5-HT3-receptor
block-ade on the terminals of enteric cholinergic neurons inhibits colonic
motility, especially in the left colon, increasing total colonic transit time.
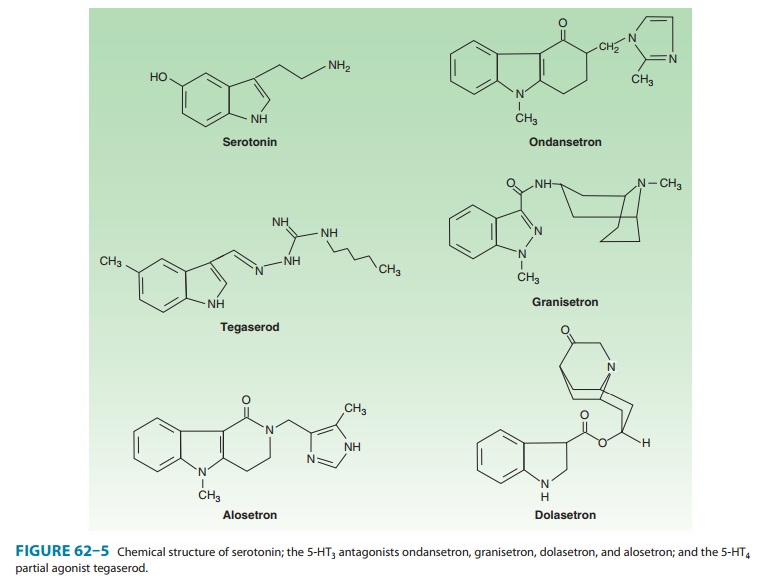
Alosetron is a 5-HT3antagonist that has been approved for thetreatment of patients
with severe IBS with diarrhea (Figure 62–5). Four other 5-HT3 antagonists
(ondansetron, granisetron, dolase-tron, and palonosetron) have been approved
for the preventionand treatment of nausea and vomiting (see Antiemetics);
however, their efficacy in the treatment of IBS has not been determined. The
differences between these 5-HT3 antagonists that determine their pharmacodynamic effects have
not been well studied.
Pharmacokinetics & Pharmacodynamics
Alosetron is a highly
potent and selective antagonist of the 5-HT3 receptor. It is rapidly absorbed from the
gastrointestinal tract with a bioavailability of 50–60% and has a plasma
half-life of 1.5 hours but a much longer duration of effect. It undergoes
extensive hepatic cytochrome P450 metabolism with renal excretion of most
metabolites. Alosetron binds with higher affinity and disso-ciates more slowly
from 5-HT3 receptors than other
5-HT3 antagonists, which
may account for its long duration of action.
Clinical Uses
Alosetron
is approved for the treatment of women with severe IBS in whom diarrhea is the
predominant symptom (“diarrhea-predominant IBS”). Its efficacy in men has not
been established. In a dosage of 1 mg once or twice daily, it reduces
IBS-related lower abdominal pain, cramps, urgency, and diarrhea. Approximately
50–60% of patients report adequate relief of pain and discomfort with alosetron
compared with 30–40% of patients treated with placebo. It also leads to a
reduction in the mean number of bowel movements per day and improvement in
stool consistency. Alosetron has not been evaluated for the treatment of other
causes of diarrhea.
Adverse Events
In
contrast to the excellent safety profile of other 5-HT3-receptor
antagonists, alosetron is associated with rare but serious gastroin-testinal
toxicity. Constipation occurs in up to 30% of patients with
diarrhea-predominant IBS, requiring discontinuation of the drug in 10%. Serious
complications of constipation requiring hospitalization or surgery have
occurred in 1 of every 1000 patients. Episodes of ischemic colitis—some
fatal—have been reported in up to 3 per 1000 patients. Given the seriousness of
these adverse events, alosetron is restricted to women with severe
diarrhea-predominant IBS who have not responded to conventional thera-pies and
who have been educated about the relative risks and benefits.
Drug Interactions
Despite being
metabolized by a number of CYP enzymes, alose-tron does not appear to have
clinically significant interactions with other drugs.
SEROTONIN 5-HT4-RECEPTOR AGONISTS
The pharmacology of tegaserod was discussed previously under Laxatives. This agent was approved for the short-term treatment of women with IBS who had predominant constipation. Controlled studies demonstrated a modest improvement (approximately 15%) in patient global satisfaction and a reduction in severity of pain and bloating in patients treated with tegaserod, 6 mg twice daily, com-pared with placebo. Owing to an increased number of cardiovascu-lar deaths observed in post-marketing studies in patients taking tegaserod, it was voluntarily removed from the market.
CHLORIDE CHANNEL ACTIVATOR
As
discussed previously, lubiprostone is a prostanoic acid deriva-tive that
stimulates the type 2 chloride channel (ClC-2) in the small intestine and is
used in the treatment of chronic constipa-tion. Lubiprostone recently was
approved for the treatment of women with IBS with predominant constipation. Its
efficacy for men with IBS is unproven. The approved dose for IBS is 8 mcg twice
daily (compared with 24 mcg twice daily for chronic consti-pation).
Lubiprostone has not been compared with other less expensive laxatives (eg,
milk of magnesia). Lubiprostone is listed as category C for pregnancy and should
be avoided in women of child-bearing age.
Related Topics