Chapter: Basic Radiology : Brain and Its Coverings
Exercise: Seizure and Epilepsy
EXERCISE 12-8.
SEIZURE AND EPILEPSY
12-18. In Case 12-18, what is the most likely diagnosis (Figure
12-38 A–C)?

A.
Alzheimer’s dementia
B.
Gray matter heterotopia
C.
Hemimegalencephaly
D.
Mesial temporal sclerosis
E.
Multiple sclerosis
Radiologic Findings
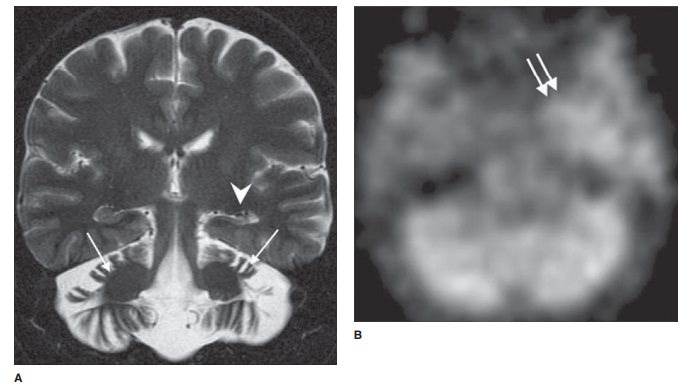
12-18. Coronal FMPIR MRI (Figure 12-38 A) demonstrates marked
atrophy of the left hippocampus with loss of normal laminar architecture (white
arrowhead). Ictal SPECT (Figure 12-38 B) shows increased radiotracer uptake in
the left medial temporal lobe (double ar-rows), whereas the interictal PET
(Figure 12-38 C) demonstrates diminished metabolic activity in the left
temporal lobe (black arrow). The constellation of findings is highly suggestive
of mesial temporal scle-rosis (D is the correct answer to Question 12-18).
Pronounced cerebellar atrophy (Figure 12-38 A) in this case is the result of
long-standing antiepileptic medication (white arrows).
Discussion
Although a comprehensive review
of seizure and epilepsy classification is beyond the scope of this section, it
is impor-tant to note the central role that imaging serves in the evalu-ation
and management of these patients. The etiology of seizure varies significantly
with patient age. In young chil-dren (3 months to 5 years), fever is the most
common precip-itant of seizure. The exact pathophysiology is not fully
understood; however, there is likely a relationship to an in-flammatory cascade
as well as a low seizure threshold in young children. Imaging is generally not
performed in the setting of a simple febrile seizure (seizures that last less
than 15 minutes, are generalized, and do not recur in a 24-hour period).
Febrile seizures that do not meet these criteria are classified as complex and
imply a more serious underlying abnormality including meningitis, abscess, or
encephalitis, for which imaging may be indicated. Other potential causes of
seizure in young children include cerebral anoxia, metabolic abnormalities,
cortical malformations (refer to Case 12-2), infection, or inherited
neurocutaneous diseases such as tuberous sclerosis.
In older children and adults,
common causes of seizure in-clude vascular malformations, cerebral injury due
to prior trauma or ischemia, or underlying tumor, among others. Note-worthy
tumors associated with intractable seizure include gan-glioglioma,
dysembryoplastic neuroepithelial tumor (DNET), and pleomorphic
xanthoastrocytoma; these generally occur in childhood or in young adulthood.
The most common cause of
medically refractory epilepsy is mesial temporal (hippocampal) sclerosis.
Although this entity is most commonly seen in adult patients, there is likely a
link to febrile seizures earlier in childhood or other remote cerebral insult
such as trauma or infection. On MR imaging, there is characteristic atrophy and
gliosis of the hippocam-pus, often with dilation of the ipsilateral temporal
horn due to volume loss. There may be atrophy and gliosis of ipsilateral fornix
and mammillary body as well. These patients are po-tential candidates for
temporal lobectomy, and additional imaging with ictal SPECT and interictal PET
is generally per-formed as described earlier.
Related Topics