Chapter: Basic Radiology : Imaging of the Spine
Imaging of the Spine: Radiology Techniques
Imaging of the Spine
The spine is critical for normal
human function, providing structure, support, and protection of the spinal cord
and spinal nerves. Given the wide range of pathologic conditions that can
affect the spine, recognition of normal anatomy and variants, differentiation
from abnormal anatomy, and diag-nosis of different pathologic conditions are
the goals of spine imaging.
It is assumed that the reader is
already familiar with basic spine anatomy learned early in medical school. With
such a foundation, this topic on the imaging appearance of the spine will serve
to solidify and perhaps even enhance this knowledge base.
TECHNIQUES
Prior to the advent of computed
tomography (CT) in the 1970s, spine imaging consisted primarily of plain-film
radi-ography and an adjunct test, myelography, to be discussed later. Spine
imaging was revolutionized by CT, and, subse-quently, magnetic resonance (MR)
imaging, which for the first time allowed direct acquisition of axial,
sagittal, and coronal (multiplanar) images, allowing for better spatial and
contrast resolution. Not until the era of CT could the spinal cord be
visualized and evaluated. These imaging modalities have so changed the face of
diagnosis and treatment of spine pathology that virtually no neurosurgeon today
would under-take spine surgery without first obtaining a CT and/or MR imaging
study.
This section reviews the major
modalities currently em-ployed to image the spine. The highly specialized
technique of spinal arteriography, which is used principally to detect vascular
malformations, is beyond the scope of this review. Nuclear medicine scanning
also is not discussed, because it is seldom used as a primary diagnostic study
in the evaluation of spine disease (though spinal metastases are frequently
di-agnosed with whole-body isotope bone scanning).
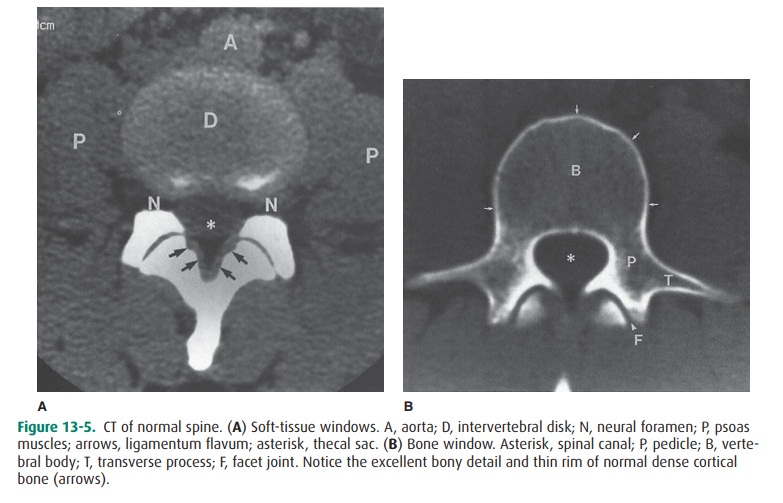
Plain Radiograph
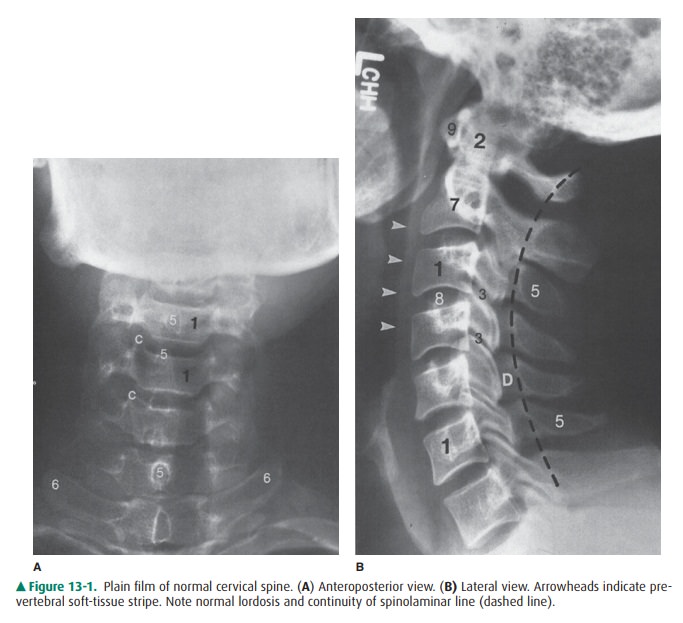
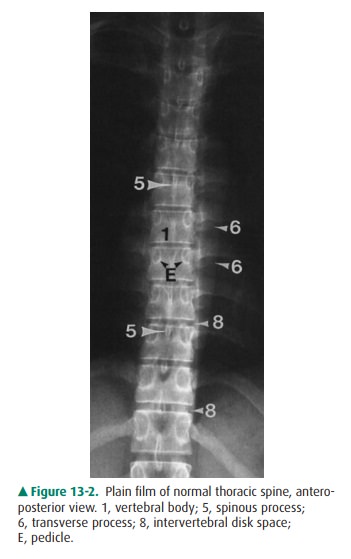
Plain films are conventional
radiographs, which are com-monly referred to as x-rays. They may be obtained in
a frontal projection—anteroposterior (AP) or posteroanterior (PA); the
difference is insignificant in the spine—a lateral projec-tion (side view), or
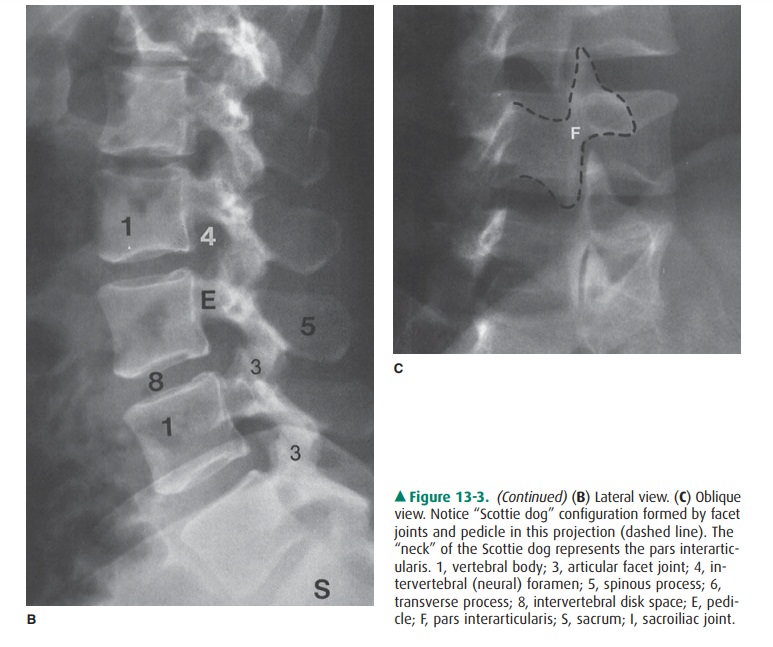
an oblique projection (Figures 13-1, 13-2, and 13-3). Plain films are most
useful for the visualization ofbony structures. Soft-tissue structures
(everything but bone) are largely radiolucent and cannot be seen clearly on
plain films unless abnormal density such as calcification is present. Although
plain films depict bone anatomy quite well, certain structures may be obscured
by other structures in front of or behind them. For instance, on a lateral
projection, both pedi-cles would be superimposed on one another (Figures 13-1 B
and 13-3 B). For this reason, multiple views are always ob-tained as part of a
routine examination.
On conventional radiographs, bony
structures appear white. This appearance is referred to as “radiodense” or
sim-ply “dense.” Normally, mineralized bones have a recognizable radiodensity,
which should always be assessed when viewing x-rays. Certain pathologic
conditions (eg, osteopenia and os-teolytic metastases) can result in decreased
bone density, and other conditions (eg, osteoblastic metastases and some exotic
diseases) may result in abnormally increased bone density.
After bone density is assessed,
the next evaluation should be the alignment of the spine. A normal spine should
show cer-vical and lumbar lordosis (anterior convexity) (Figures 13-1 and 13-3)
and thoracic kyphosis (posterior convexity). Ab-normalities in alignment may
result from incorrect position-ing of the patient or be a reflection of an
underlying problem. Such abnormalities may be minor, such as straightening or
reversal of normal cervical lordosis in the case of muscle spasm. Abnormal
curvature, such as scoliosis, may be idio-pathic, congenital, or secondary to
an underlying lesion.
Major alterations in alignment,
such as subluxation, can re-sult from trauma. In assessing alignment, it is
important to determine whether the vertebral bodies, as well as the poste-rior
elements (ie, spinous processes, pedicles, and laminae), are appropriately
positioned. The spinal cord rests within the spinal canal formed by the foramen
within each vertebra, but the cord is not visible on plain films. Its location
is thus de-fined by identifying the boundaries of the spinal canal. The
anterior margin of the spinal canal is the posterior aspect of the vertebral
body, and the posterior limit of the spinal canal can be approximated by
locating, on a lateral radiograph, the junction of the spinous process and the
laminae. Identifica-tion of the spinolaminar line also helps in the evaluation
of alignment (Figure 13-1 B).
Most anatomic features of the
spine are readily identifi-able on plain radiographs (Figures 13-1, 13-2, and
13-3) such as vertebral bodies, facet joints, disk spaces, pedicles, laminae,
transverse and spinous processes, and the neural foramen, whereas certain other
areas can be evaluated only on special-ized views. For instance, the open-mouth
view facilitates vi-sualization of the atlantoaxial (C1-2) articulation and
provides an additional view of the dens (Figure 13-1 D). This view is an
essential component of a trauma workup. Oblique views allow visualization of
the neural foramen in the cervi-cal spine (lateral views are used for this
purpose in the thora-columbar spine) (Figure 13-1 C). The neuroforamina are
formed by the pedicles of the vertebrae above and below (Figures 13-1 C and
13-3 B) and allow for the exit of the spinal nerves from the spinal canal.
There are 8 pairs of cervical spinal nerves, 12 pairs of thoracic spinal
nerves, and 5 pairs of lumbar spinal nerves. Abnormal bony projections, known
as osteophytes, are a common manifestation of de-generative spine disease and,
if present within the neural foramen, may be a cause of nerve root compression.
Spinal nerves also can be compressed by disk herniations, but this type of
neural compression cannot be diagnosed by means of plain films alone.
Small bony structures, such as the
cervical transverse foramen (for the vertebral artery) and the small facets for
rib articulation in the thoracic spine, are not well visualized on plain
radiographs. Because “soft-tissue” structures are also poorly demonstrated on
plain radiographs, the intervertebral disk is not well seen with x-rays unless
it is calcified (and therefore dense). However, differences in the soft-tissue
den-sity can impart additional information. In the cervical spine, for
instance, calcification in the region of the carotid artery bifurcation may
suggest atherosclerotic vascular narrowing. In the evaluation of cervical
trauma, one should always assess the width of the normal soft-tissue stripe
that is anterior tothe vertebral bodies (Figure 13-1 B). This prevertebral soft-tissue
stripe may become widened in cervical spine trauma (prompting a closer search
for fracture) and also in certain inflammatory conditions. When reviewing
thoracic or lum-bar spine films, attention to the soft tissues may facilitate
di-agnosis of a host of conditions ranging from pneumonia and lung cancer to
retroperitoneal diseases and abdominal aortic aneurysms. Therefore, it is
important not to focus only on the spine when interpreting spine radiographs.
Myelography
Contrast myelography has been
around since its accidental discovery in 1922, when Sicard and Forestier,
intending to administer extradural lipiodol to treat sciatica, inadvertently
introduced the material into the subarachnoid space. This radiopaque oil was
noted to move freely, and it was immedi-ately recognized that with the use of
fluoroscopy (real-time radiography) and conventional radiography, this
procedure would be useful for diagnosing intraspinal tumors. Lipiodol quickly
replaced air as the medium of choice for myelogra-phy (air is lucent and is
therefore a “negative” contrast agent; iodinized oils such as lipiodol and,
later, the popular Pan-topaque (iophendylate) are dense and therefore
“positive” contrast agents). Following Mixter and Barr’s 1934 report on the
syndrome of herniated intervertebral disk, myelography became a widely used
test. In the 1980s, the wide availability of less toxic water-soluble agents
and, finally, nonionic contrast agents such as iopamidol and iohexol made
myelography a readily tolerated procedure.
Myelography is employed most
commonly to evaluate for disk herniations and to rule out spinal cord
compression caused by tumor or trauma. In many parts of the United States, CT
and MR imaging have all but replaced myelography. However, in many locations,
myelography is still performed. A myelogram is often followed by a
postmyelogram CT ex-amination, which is addressed later.
The technique for performing
myelography is simple. The patient is placed prone on a fluoroscopy table.
Under fluoro-scopic guidance, a lumbar puncture (LP) is made with an 18- to
22-gauge spinal needle (a fluoroscopically guided LP is much easier than an LP
performed on a sick patient on the ward in the decubitus position).
Cerebrospinal fluid (CSF) is then drawn for laboratory tests if needed, and
contrast material is placed into the subarachnoid space. Once instillation of
the contrast agent is fluoroscopically confirmed, the needle can be withdrawn
and the spine studied. Depending on the spinal level to be examined, the
patient can be standing, flat, or in Trendelenburg position. Typically,
multiple views includinglateral, AP, and oblique views are obtained. In the
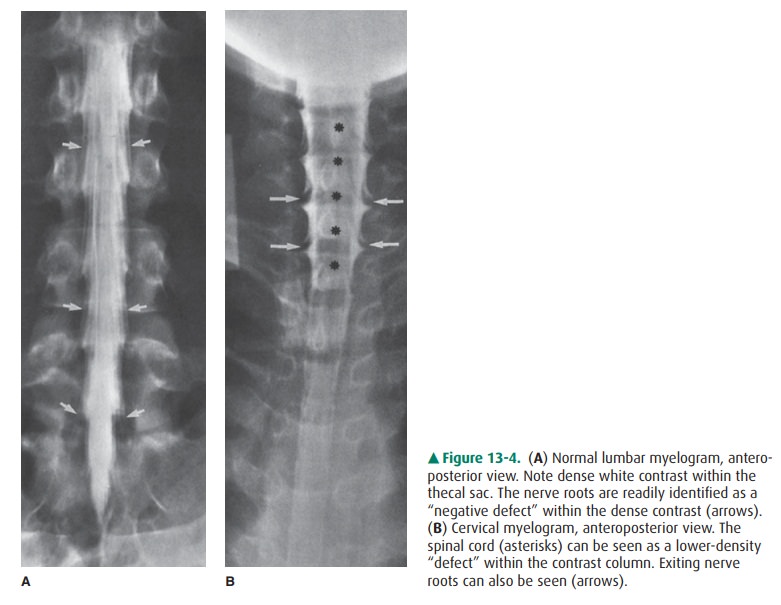
lumbar re-gion, the cauda equina nerve roots are well visualized (Figure 13-4
A). The conus medullaris, usually at L1-2, also can be seen. In the thoracic
and cervical levels, the spinal cord can be seen as a “negative” shadow within
the dense contrast, and its size and shape can therefore be evaluated (Figure 13-4
B). Cervical spinal nerves are also well seen (Figure 13-4 B). The presence of
any lesions and their precise location relative to the dura usually can be
determined on the basis of the myel-ographic appearance. For instance, lesions
may be extradural, intradural but extramedullary (not in the spinal cord), or
in-tramedullary (within the spinal cord).
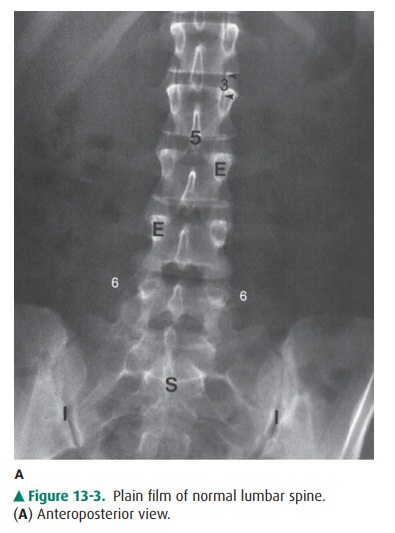
Computed Tomography
CT utilizes x-rays to obtain
images by means of multiple sources and detectors surrounding the patient in a
radial fashion. This is why the patient appears to be entering a large
doughnut-shaped device during the CT examination. Thedata obtained are
processed by a computer, which then gen-erates an image. Nowadays, with multidetector
CT, image re-construction in coronal, sagittal, and oblique planes in addition
to the source axial images allows for improved spa-tial resolution. Once the
raw data are obtained, images can be displayed with different “windows” and
“level” values that take advantage of density (“attenuation” in CT terminology)
differences between tissues. For instance, filming a set of soft-tissue windows
allows differentiation of soft-tissue structures that are very similar in
attenuation to adjacent structures (eg, muscle and fluid). This is one of the
key features of CT, whereas plain films usually cannot distinguish between the
different soft tissues as well. In the spine, CT makes it possi-ble to
discriminate between CSF, nerve roots, and ligaments, for instance. Therefore,
a CT examination can demonstrate the ligamentum flavum, nerve roots, epidural
fat, and other structures that cannot be identified discretely on plain films
(Figure 13-5 A). Additionally, images can be obtained with a bone algorithm, whose
window and level gives detailed information about bony structures (Figure 13-5
B), although on such images, little soft-tissue information is available.
CT is widely used to image the
spine in the evaluation of many pathologic conditions. Most common indications
in-clude trauma, spine tumors, and degenerative disk disease(ie, to rule out
disk herniation in patients with myelopathy or radiculopathy). Assuming a
normal appearance on plain films, CT is often the first study ordered in the
evaluation of patients with back pain.
CT Myelography
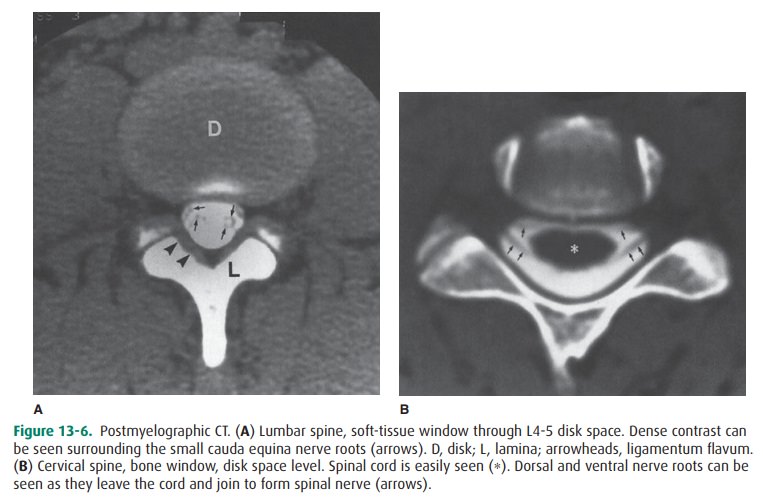
As mentioned earlier, in patients
who have undergone myel-ography, CT is often obtained immediately afterwards
(Figure 13-6). It has been shown that a postmyelogram CT is more sensitive in
the detection of pathologic conditions than is either test alone. This is
particularly true for lesions within the spinal canal, such as disk herniations
or tumors unassoci-ated with a bony component. The presence of subarachnoid
contrast allows dramatic visualization of the cauda equina nerve roots and
spinal cord in a way that cannot be achieved with regular CT.
MR Imaging
Since the early 1980s, MR imaging
has gained widespread acceptance as the most sensitive imaging modality in the
study of spine disease. MR imaging undeniably allows visu-alization of
intraspinal anatomy with much higher contrastresolution than does any other
modality. The ability to image directly in the sagittal and coronal planes
contributes a great deal to the evaluation of the diseased spine. A
de-scription of the physics of MR imaging is beyond the scope of this topic,
and the reader is referred elsewhere for this information. Because dense
cortical bone has few mobile protons (which are necessary to create an MR
signal), MR imaging is sometimes limited in its ability to demonstrate ei-ther
osteophytes that may be a source of clinical symptoms or calcific components of
other lesions. In such cases, CT with its superb depiction of bony detail may
be useful as an adjunct examination. On the other hand, MR imaging is very
sensitive in its ability to detect abnormalities in bone marrow. The vertebral
bodies normally contain a large amount of bone marrow, and an abnormal
appearance may be seen in a variety of disorders, such as anemia, infection,
and metastatic disease.
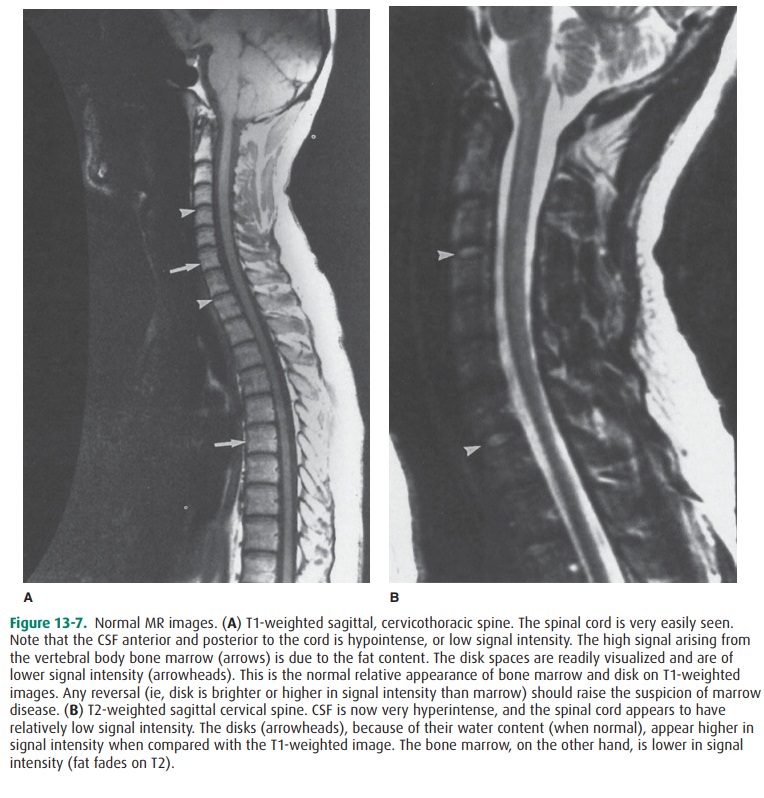
MR images can be obtained with a
variety of “sequences.” The most commonly utilized are called “spin-echo,” and
these can be “weighted” for either T1 or T2. (A thorough ex-planation of these
parameters can be found elsewhere). On a T1-weighted image, normal adult
(yellow/fatty) bone mar-row has a “high signal” (ie, it is hyperintense,
whitish in color), and CSF has a “low signal” (ie, it is hypointense, or black
in color). Neural tissue, such as the spinal cord or nerve roots, is
intermediate in signal intensity (Figure 13-7 A). Cor-tical bone, lacking
mobile protons to produce a signal, is hy-pointense on all pulse sequences. On
T2-weighted images, marrow becomes lower in signal intensity, CSF becomes
hy-perintense, and neural tissue maintains an intermediate sig-nal intensity.
However, the spinal cord appears relatively lower in signal intensity,
surrounded as it is by CSF that is hy-perintense (Figure 13-7 B). The
intervertebral disks in normal individuals are typically of intermediate signal
on T1-weighted images and, because of their water content, appear hyperintense
on T2-weighted images. Any alterations in the expected normal signal intensity
for an anatomic structure should prompt a search for either a technical or a
pathologic explanation for the abnormal signal. Postcontrast imaging, scanning
after administration of intravenous gadolinium (gadopentetate dimeglumine) or
other paramagnetic con-trast agents, adds valuable information to either
clarify ques-tions raised by the precontrast imaging results or permit
detection of lesions that were invisible without contrast. In recent years, the
use of fat suppression has increased the util-ity of contrast-enhanced imaging
of the spine, particularly in the evaluation of lesions within the spinal canal
(Figure 13-8) and bone.

Related Topics