Chapter: Basic Radiology : Imaging of the Spine
Exercise: Spine Infection And Inflammation
EXERCISE 13-4.
SPINE INFECTION AND INFLAMMATION
13-11. What is the most likely diagnosis in Case 13-11 (Figure
13-27)?

A.
Spine metastases
B.
Posttraumatic changes
C.
Discitis and osteomyelitis
D.
Epidural abscess
E.
Degenerative changes
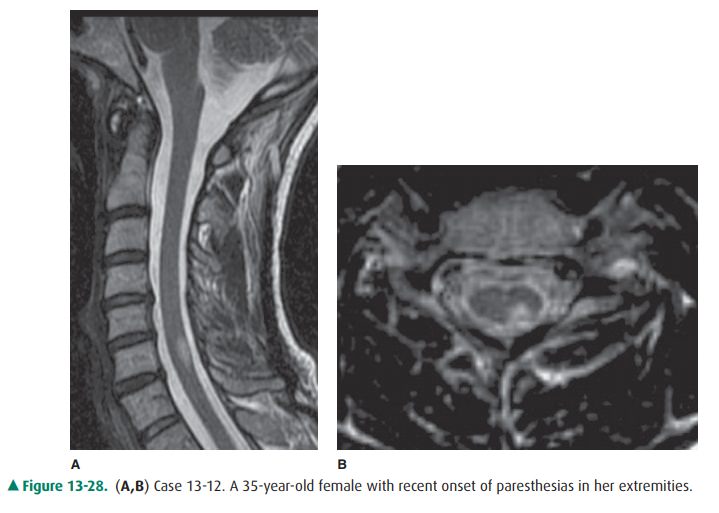
13-12. Regarding Case
13-12, what is the main abnormality visualized in Figure 13-28?
A.
None
B.
Artifact
C.
Subarachnoid lesion
D.
Intramedullary lesion
E.
Syrinx
Radiologic Findings
13-11. In this case, there is discitis and osteomyelitis (C is
the correct answer to Question 13-11). Enhancement is identified within the
C3-4 and C4-5 intervertebral disks with involvement of the adjacent vertebral
bod-ies on the sagittal T1-weighted postcontrast images (Figure 13-27 A) and an
increase in the T2 hyperin-tensity in Figure 13-27 B. Additionally,
enhancement, T2 hyperintensity, and increased thickness within the prevertebral
soft tissues from C2-C5 levels (arrow-head) is present. There is linear
epidural enhance-ment seen at the C5 level (arrow).
13-12. In this case, the sagittal T2-weighted image
demon-strates an intramedullary T2 hyperintense lesion at the C6 level that on
the axial image is localized to the left posterior cord (D is the correct
answer to Ques-tion 13-12).
Discussion
Spine infections include
vertebral osteomyelitis and discitis, which occur most commonly as a result of
hematogenous spread. Penetrating trauma, contiguous spread from
adjacentinfection, or iatrogenic causes are additional routes of
dis-semination. The presenting feature is usually pain. A major-ity of the
lesions occur in the lumbar spine, followed by the thoracic spine, with peak
incidences between 60 and 80 years of age. Staphylococcus
aureus is the most common organism in adults. Epidural abscess can result
as a complication of os-teomyelitis and is commonly associated with diabetics,
pa-tients with chronic renal failure, alcoholics, and intravenous drug users.
Ventral location of the epidural abscess is usually seen in cases secondary to
osteomyelitis. MR imaging has a specificity, sensitivity, and accuracy of 92%,
96%, and 94%, respectively, for detection of vertebral osteomyelitis. Imaging
characteristics include increase in T1 hypointensity and T2 hyperintensity,
along with variable enhancement in the inter-vertebral disk and adjacent vertebral
body as seen in Case 13-11, Figure 13-27. Although T2 hyperintensity and
con-trast enhancement can be seen in degenerative changes, in-fection of the
spine is commonly associated with paraspinal and epidural inflammatory changes.
Inflammatory diseases of the
spinal cord can result from both infectious and noninfectious causes. The
noninfective etiologies are more common and include disorders such as multiple
sclerosis, acute disseminated encephalomyelitis(ADEM), idiopathic transverse
myelitis, Devic’s disease, and sarcoidosis. Multiple sclerosis (MS) is
diagnosed with tempo-ral and spatially varied clinical signs and symptoms of
white matter involvement supplemented by CSF analysis and MRI findings that are
seen in more than 90% of cases. The cervical cord is more likely to be
affected. Abnormality in the cord ranges from one to multiple lesions, although
diffuse involve-ment of the cord can also be seen. Typically, lesions occupy a
seg-ment less than two vertebral bodies in length (Figure 13-28 A), are peripherally
located within the posterior or lateral white matter, and involve less than
half the cross-sectional area of the cord as seen in Figure 13-28 B. Presence
of enhancement is thought to be reflective of active disease. ADEM is
histo-pathologically inseparable from MS and can be differentiated from MS on
account of its monophasic nature. Idiopathic acute transverse myelitis lesions,
on the other hand, are frequently greater than two vertebral segments in length
and clinically present with bilateral signs or symptoms as well as a clearly
defined sensory level.
Related Topics