Chapter: Basic Radiology : Imaging of the Spine
Exercise: Neoplastic Spine Disease
EXERCISE 13-2. NEOPLASTIC SPINE DISEASE
13-4. In Case 13-4, what does this the
AP view from a tho racic myelogram in Figure 13-15 show?

A.
A bony abnormality
B.
An extradural mass
C.
An intradural-extramedullary mass
D.
An intramedullary mass
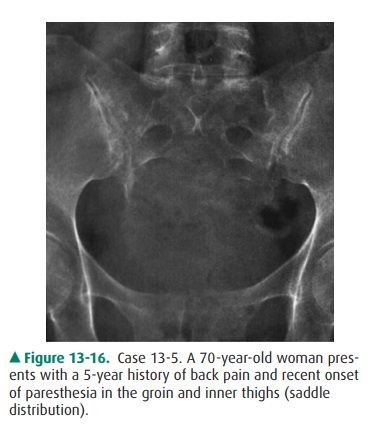
13-5.In Case 13-5, what is the
most likely diagnosis(Figure 13-16)?
A. Sacroiliitis
B.
A sacral tumor
C.
Constipation
D.
Osteoporosis
E.Uterine malignancy
13-6.In Case 13-6, on the lateral cervical spine radiograph in Figure
13-17, what is the main radiologic finding?
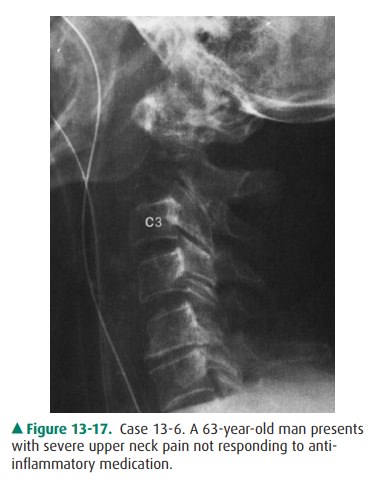
A. A
lesion of the C7 spinous process
B. An osteoblastic bony lesion
C. An abnormality of alignment
D. A destructive lesion at C2
E. A fracture
13-7. In Case 13-7, Figure 13-18, what diagnostic
possibili-ties should be most seriously considered?
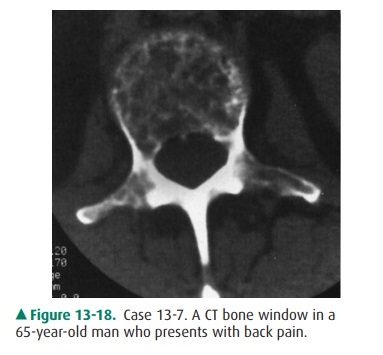
A.Congenital or traumatic lesions
B.Metabolic or endocrine disease
C.Myeloma or metastatic disease
D.Infectious or inflammatory disease
E.Degenerative or inflammatory disease
Radiologic Findings
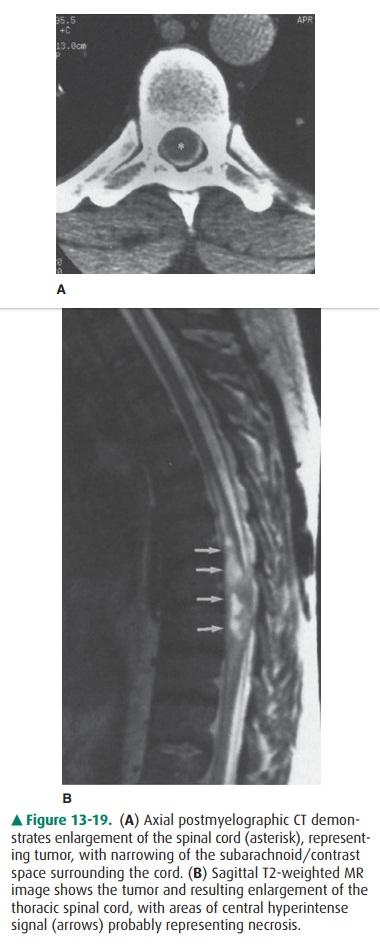
13-4. In this case, the patient has a lower thoracic primary spinal
cord astrocytoma (D is the correct answer to Question 13-4). The cord is normal
inferiorly but is seen to get wider toward the middle of the image. The
contrast column on either side of the lesion is nar-rowed, most noticeably on
the patient’s right. This le-sion has caused a “block” to the flow of contrast.
Subsequent postmyelography CT (Figure 13-19 A) confirmed the spinal cord
enlargement. An MR image demonstrated the tumor (Figure 13-19 B) within the
spinal cord.
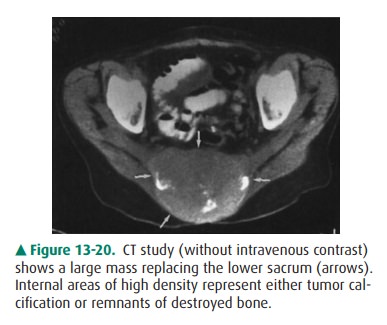
13-5. In this case, the plain film shows a large destructive mass
replacing most of the lower sacrum (B is the cor-rect answer to Question 13-5).
Notice how normal bone disappears below the midsacrum. A CT showed a large
destructive mass with areas of calcification (Figure 13-20).
13-6. In this case, the plain film shows that the body of C2
has been destroyed (lytic destruction) (D is the correct answer to Question
13-6).
13-7. In this case, the CT image shows multiple small areas of
lytic bony destruction. This is characteristic of ei-ther multiple myeloma or
metastatic disease (C is the correct answer to Question 13-7).
Discussion
Primary tumors of the spine can
arise from the bone or the neural elements. In Case 13-4, the diagnosis was
primary spinal cord glioma. The two most common spinal cord tumors are
astrocytomas and ependymomas. As with this patient, the diagnosis may be
elusive for some time while other diseases such as disk herniation are ruled
out. This patient even had a normal lumbar MR examination several months prior
to the myelogram. Although the thoracolumbar junction is usually visualized on
a lumbar MR imaging study, this tumor (at T10) was just missed. A thoracic MR
examination would certainly have made the diagnosis, but the patient’s doctor ordered
a myelogram. Spinal cord tumors are generally very difficult to treat. The more
malignant ones, usually astrocytomas, are as-sociated with a poor prognosis.
Ependymomas, because they are less infiltrative and more readily resectable,
are associated with a much better prognosis.
Primary bone tumors can be benign
or malignant. In the sacrum, giant-cell tumor is the most common benign tumor.
The most common primary sacral malignancy is chordoma. This is the diagnosis in
Case 13-5. Chordomas develop from remnants of the embryonic notochord and
represent 2% to 4% of primary malignant bone tumors. The sacrum is the most
common site for chordoma, accounting for 50% of these lesions. The skull base
accounts for 35% and other vertebraeaccount for 15%. Typical presentation of
sacral chordoma is low back pain, paresthesias, or rectal dysfunction. Figure
13-16 shows the typical radiographic appearance of expansile, lytic
destruction. On CT (see Figure 13-20), a large soft-tissue mass with internal
calcifications is characteristic.
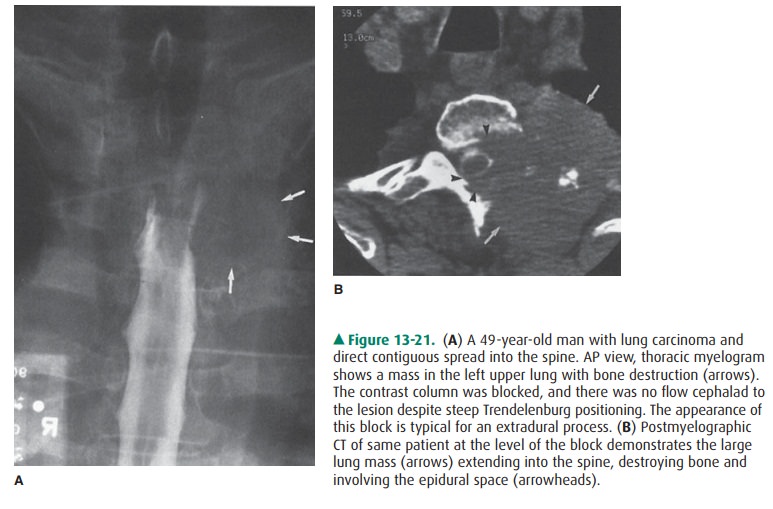
A common type of malignant spine
tumor is metastatic dis-ease, with lung and breast being the most frequent
primarysites. Virtually any tumor may metastasize to the spine. In gen-eral,
certain tumors tend to result in osteoblastic or dense metastases, and prostate
adenocarcinoma falls in this category. Other primary malignancies, such as
those in the lung and breast, tend to have osteolytic, destructive spine
metastases. The patient in Case 13-6 had lung carcinoma, and Figure 13-17 rep-resents
a hematogenous spread of tumor to the C2 vertebral body. Metastatic disease may
affect the spine by other mecha-nisms. Tumors adjacent to the spine may grow
directly into it (Figures 13-21 A, B). This may occur in lung carcinoma and
le-sions such as neuroblastoma or lymphoma (with retroperi-toneal/paraspinal
lymphadenopathy). Finally, the spinal canal may be affected by spread of
malignant neoplasm. Rarely, a metastatic lesion may occur in the spinal cord
itself, usually as a terminal event. Metastatic disease may occur in the
subarach-noid space by two methods. First, an intracranial malignancy (ie,
glioma, medulloblastoma) can seed the subarachnoid space. These are known as
“drop” metastases. Hematogenous spread to the subarachnoid space may occur in non-CNS
pri-mary tumors. Such involvement is known as leptomeningeal carcinomatosis or
carcinomatous meningitis (see Figure 13-8) and is associated with a very poor
prognosis.
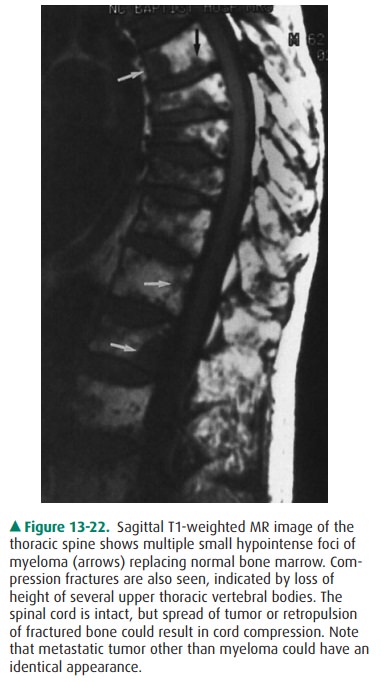
Multiple myeloma is a
disseminated malignancy caused by a proliferation of plasmacytes, typically
occurring in the mid-dle-aged and elderly, with a slight male predominance.
Thespine may be affected primarily or secondarily, and bone painaused by
pathologic compression fracture is the most com- mon symptom. Plain films may
be normal early in the course of the disease or show only mild osteopenia.
Later, multiple,small, lytic, “punched out” lesions may be seen. CT is very
sensitive, and Figure 13-18 shows the typical CT appearance of multiple
myeloma. The findings, however, would be indistinguishable from those of small
lytic metastases of other origin,and for this reason, metastases and myeloma
are often mentioned together in the context of multiple small lytic bony
lesions. MR imaging of multiple myeloma may have different appearances, but the
typical pattern would be multiple, small foci of decreased signal intensity
replacing the normal hyperintense bone marrow on T1-weighted images (Figure
13-22).
Related Topics