Chapter: Biology of Disease: Toxicology
Ethanol - Toxicology Poisons
ETHANOL
Ethanol is an addictive drug and its abuse can lead to
dependency and alcoholism. Its abuse is increasingly common in the developed
world. The toxic effects of chronic alcohol abuse on the liver, brain and GIT
are widely known. Ethanol can also modify the effects of other drugs, for
example it inhibits the hydroxylation of barbiturates by the P-450 system
preventing their ready excretion by the kidneys.
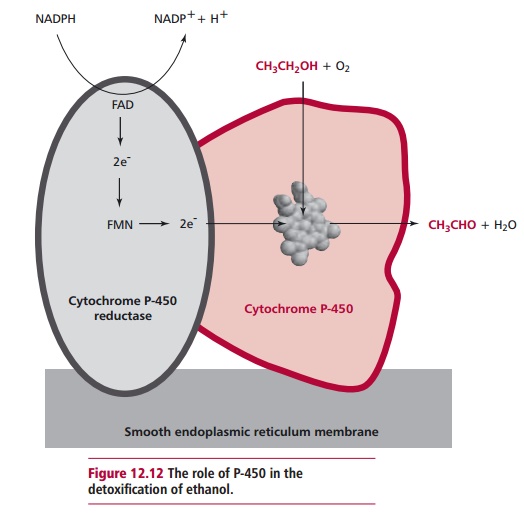
The metabolism of ethanol occurs mainly in the liver by one of
two mechanisms. Normally only small amounts are degraded by the P-450 system (Figure 12.12), although this oxidation
can become of major importance because the P-450 system is induced by chronic
alcohol consumption. The
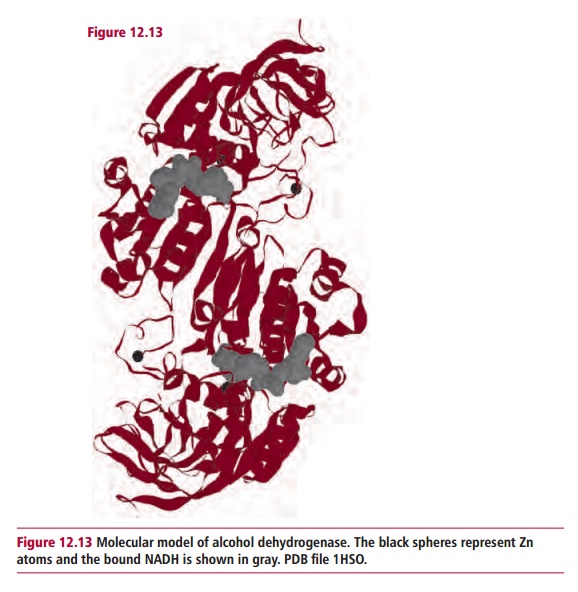
major catabolic pathway is to oxidize ethanol to the
corresponding aldehyde, ethanal, in a reaction catalyzed by alcohol
dehydrogenase, ADH (Figure12.13).
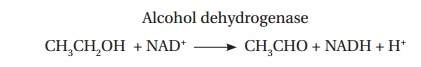
Alcohol
dehydrogenase
CH3CH2OH
+ NAD+ ® CH3CHO + NADH + H+
The effectiveness of ADH varies between different populations
and hence the undesirable effects of drinking can appear after widely varied
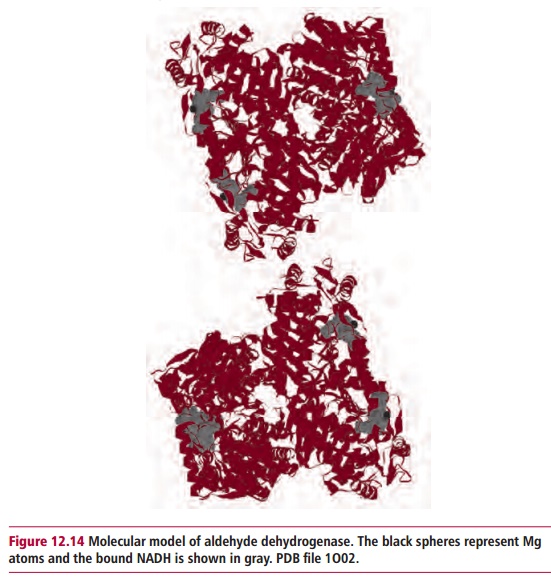
intakes. The ethanal may subsequently be oxidized to ethanoic acid (acetic
acid) by aldehyde dehydrogenase, ALDH (Figure
12.14).
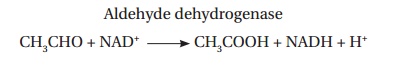
Aldehyde
dehydrogenase
CH3CHO + NAD+
® CH3COOH + NADH + H+
Much of the acetate made from ethanol escapes into the blood and
can result in acidosis . The effect of both enzymes is to increase the NADH/NAD+
ratio, that is, alcohol consumption leads to the accumulation of NADH with
consequent severe effects. The increased NADH inhibits fatty acid oxidation and
stimulates the synthesis of triacylglycerols in the liver producing a fatty
liver. The oxidation of lactate to pyruvate is also inhibited, slowing
gluconeogenesis (Margin Note 12.3).
The increased lactate exacerbates the acidosis and the decreased
gluconeogenesis may cause hypoglycemia.
The capacity of liver mitochondria to oxidize acetate to CO2
is limited because the activation of acetate to acetyl CoA requires ATP:
Acetate + Coenzyme A + ATP ® acetyl CoA + AMP + PPi
Adenosine triphosphate is now in short supply because
glycolysis, which requires free NAD, is slowed and because the processing of acetyl
CoA by the TCA cycle is blocked since NADH inhibits the regulatory enzymes
isocitrate dehydrogenase and 2-oxoglutarate dehydrogenase. Acetyl CoA is
converted to ketone bodies that are released into the blood, intensifying the
acidosis caused by acetate and lactate. Acetaldehyde also accumulates and this
extremely reactive compound can bind to liver proteins, impairing their
functions and causing severe damage to liver cells, leading to their death.
Acetaldehyde can also escape from the liver and react with blood proteins to
form stable adducts. These can provide useful markers of the past drinking
activity of an individual.
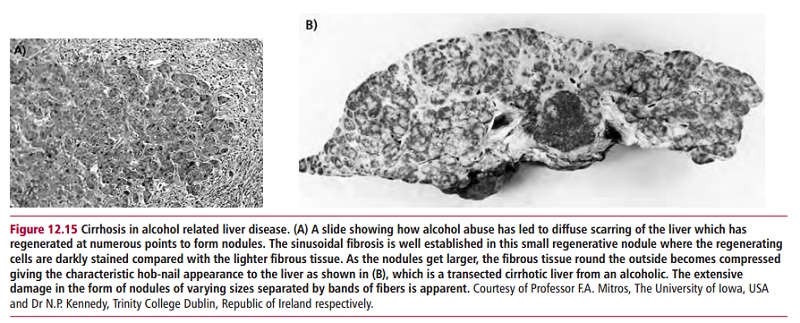
Liver damage from excessive alcohol consumption occurs in three
stages. The first stage is the formation of the fatty liver described above.
This condition, in the absence of other complications, is readily reversible
within four to six weeks if alcohol is avoided. The second stage is the
occurrence of alcoholic hepatitis when groups of liver cells die. This leads to
inflammation and can be fatal. In the third stage, the patient may develop
cirrhosis, a condition seen in 10% to 15% of alcoholics (Figure 12.15 (A) and (B)).
Approximately half of all cases of cirrhosis are due to alcoholic liver
disease. Cirrhosis occurs when fibrous structures and scar tissue are produced
around the dead cells. This impairs many of the biochemical functions of the
liver, for example, cirrhotic liver cannot convert ammonia to urea and the
concentration of ammonia in the blood rises. Ammonia is toxic to the nervous
system and can cause comaand death. Ethanol also directly affects the central
nervous system (CNS). For example, it enhances the inhibitory affects of F aminobutyric acid (GABA) at the GABAA
receptor and the functions of some 5-hydroxytryptamine receptors, in addition
to numerous other membrane proteins. The resulting depressive effects of these
activities are well known.
Chronic liver damage invariably results in malnutrition, partly
due to malabsorption and partly because the metabolism of nutrients by the
liver is defective. However, many alcoholics are malnourished because of
dietary inadequacies. While ethanol supplies most of their energy needs they
may be ingesting insufficient amounts of other nutrients, particularly proteins
and vitamins . In addition, chronic alcohol ingestion can damage the mucosal
lining of the GIT and pancreas as well as the liver . Alcoholics require
increased amounts of vitamins and some trace elements because of the metabolic
load experienced and their increased excretion. For example, niacin, although
not strictly a vitamin since it can be formed, albeit very inefficiently, from
tryptophan , is necessary to form the coenzymes, NAD+ and NADP+.
A borderline deficiency of niacin leads to glossitis
(redness) of the tongue while a pronounced deficiency leads to pellagra, with
dermatitis, diarrhea and dementia. In developed countries, pellagra is rarely
encountered other than in alcoholics, given their severe malabsorption
problems, hence dietary supplies of niacin and tryptophan are required. A
severe zinc deficiency also occurs primarily in alcoholics, especially those
suffering from cirrhosis. Heavy drinkers frequently suffer from GIT varicose
veins and diarrhea caused by a variety of factors, including ethanol-exacerbated
lactase deficiency and interference with normal peristalsis. Steatorrhea is
also common, due to deficiencies in folic acid and bile salts in the GIT .
The obvious treatment for alcoholic liver disease and cirrhosis
is abstinence. Given the addictive nature of ethanol, this may be difficult to
maintain. Unfortunately, patients presenting with severe alcoholic hepatitis
have a high mortality even when abstinence is successful. Although a number of
pharmacological treatments have been attempted as therapies, none has been
successful. However, supportive nutritional management in cases of acute and
chronic liver disease is essential to achieve electrolyte, vitamin and protein
replenishments. The only treatment for advanced cirrhosis is a liver transplant
.
The major enzyme involved in ethanol metabolism, alcohol
dehydrogenase, has a broad specificity and can catalyze the oxidation of a
range of alcohols. This allows ethanol to be used as a competitive inhibitor of
the enzyme in the treatment of poisoning by other alcohols, such as methanol
and ethylene glycol.
Related Topics