Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Corticosteroid Therapy
Corticosteroid Therapy
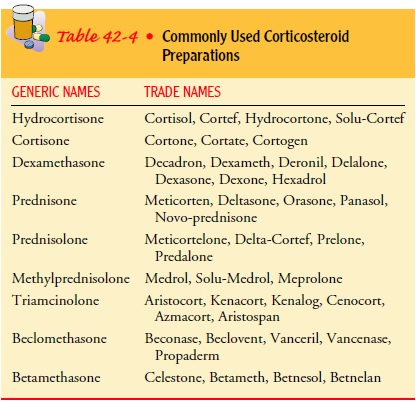
Corticosteroids
are used extensively for adrenal insufficiency and are also widely used in
suppressing inflammation and auto-immune reactions, controlling allergic
reactions, and reducing the rejection process in transplantation. Commonly used
cor-ticosteroid preparations are listed in Table 42-4. Their anti-inflammatory
and antiallergy actions make corticosteroids effec-tive in treating rheumatic
or connective tissue diseases, such as rheumatoid arthritis and systemic lupus
erythematosus. They are also frequently used in the treatment of asthma,
multiple sclero-sis, and other autoimmune disorders.
High doses appear to allow patients to tolerate high degrees of stress. Such antistress action may be caused by the ability of cor-ticosteroids to aid circulating vasopressor substances in keeping the blood pressure elevated; other effects, such as maintenance of the serum glucose level, also may keep blood pressure elevated.
SIDE EFFECTS
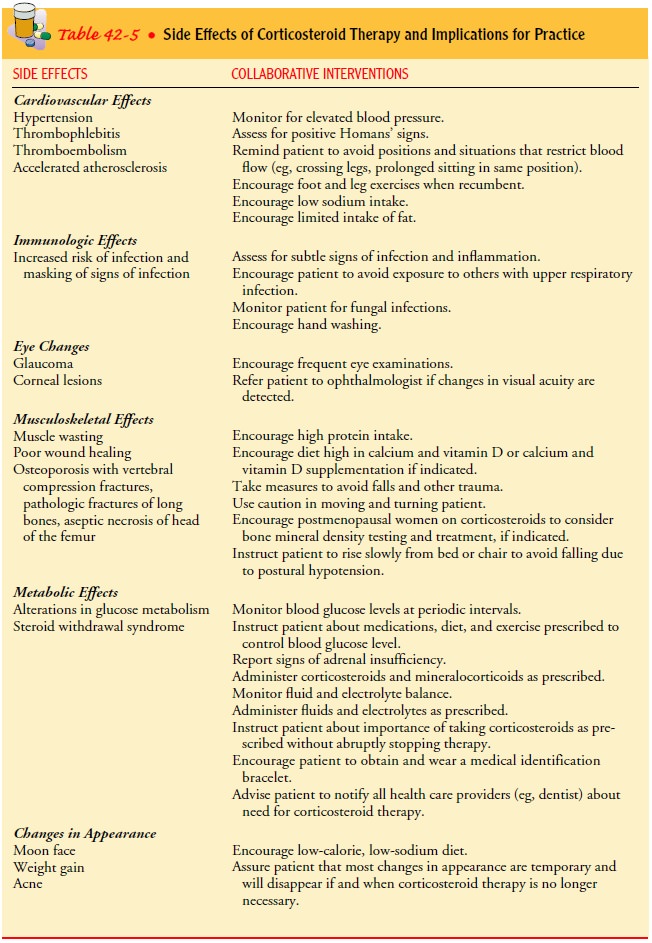
Although
the synthetic corticosteroids are safer for some patients because of relative
freedom from mineralocorticoid activity, most natural and synthetic
corticosteroids produce similar kinds of side effects. The dose required for
anti-inflammatory and anti-allergy effects also produces metabolic effects,
pituitary and adrenal gland suppression, and changes in the function of the
central nervous system. Thus, although corticosteroids are highly effective
therapeutically, they may also be very dangerous. Dosages of these medications
are frequently altered to allow high concentrations when necessary and then
tapered in an attempt to avoid undesirable effects. This requires that patients
be ob-served closely for side effects and that the dose be reduced when high
doses are no longer required. Suppression of the adrenal cortex may persist up
to a year after a course of corticosteroids of only 2 weeks’ duration.
THERAPEUTIC USES OF CORTICOSTEROIDS
The
dosage of corticosteroids is determined by the nature and chronicity of the
illness as well as the patient’s other medical problems. Rheumatoid arthritis,
bronchial asthma, and multi-ple sclerosis are chronic disorders that
corticosteroids do not cure; however, these medications may be useful when
other measures do not provide adequate control of symptoms. In ad-dition,
corticosteroids may be used to treat acute exacerbations of these disorders.
In
such situations, the adverse effects of corticosteroids are weighed against the
patient’s current problems. These medica-tions may be used for a period but
then are gradually reduced or tapered as the symptoms subside. The nurse plays
an im-portant role in providing encouragement and understanding during the
times the patient may experience (or is apprehensive about experiencing)
recurrence of symptoms while taking smaller doses.
Treatment of Acute Conditions
Acute
flare-ups and crises are treated with large doses of corti-costeroids. Examples
include emergency treatment for bronchial obstruction in status asthmaticus and
septic shock from sep-ticemia caused by gram-negative bacteria. Other measures,
such as anti-infective agents or medications, are also used with
corti-costeroids to treat shock and other major symptoms. At times,
corticosteroids are continued past the acute flare-up stage to pre-vent serious
complications.
Eye Treatment
A
different problem exists when corticosteroids are used in treat-ing eye
infections. Outer eye infection can be treated by topical application of eye
drops because these do not cause systemic tox-icity. However, long-term
application may cause an increase in intraocular pressure, which leads to
glaucoma in some patients. In some patients, prolonged use of corticosteroids
leads to cataract formation.
Dermatologic Disorders
Topical
administration of corticosteroids in the form of creams, ointments, lotions,
and aerosols is especially effective in many dermatologic disorders. It may be
more effective in some condi-tions to use occlusive dressings around the
affected part to achieve maximum absorption of the medication. Penetration and
ab-sorption are also increased if the medication is applied when the skin is
hydrated or moist (eg, immediately after bathing).
Absorption
of topical agents varies with body location. For ex-ample, absorption is
greater through the layers of skin on the scalp, face, and genital area than on
the forearm; as a result, use of topical agents on these sites increases the
risk for side effects of the medication. The availability of over-the-counter
topical cor-ticosteroids increases the risk for side effects in patients who
are unaware of their potential risks. Excessive use of these agents,
es-pecially on large surface areas of inflamed skin, can lead to de-creased
therapeutic effects and increased side effects.
DOSAGE
Attempts
have been made to determine the best time to ad-minister pharmacologic doses of
steroids. When symptoms have been controlled on a 6-hour or 8-hour program, a
once-daily or every-other-day schedule may be implemented. In keeping with the
natural secretion of cortisol, the best time of the day for the total
corticosteroid dose is in the early morning from 7 to 8 AM. Large-dose therapy at 8 AM, when the gland is most active, pro-duces maximal
suppression of the gland. A large 8 AM dose is more
physiologic because it allows the body to escape effects of the steroids from 4
PM to 6 AM, when serum levels are normally low, hence
minimizing cushingoid effects. If symptoms of the disorder being treated are
suppressed, alternate-day therapy is helpful in reducing pituitary-adrenal
suppression in patients re-quiring prolonged therapy. Some patients report discomfort
as-sociated with symptoms of their primary illness on the second day;
therefore, it is important to explain to patients that this regimen is
necessary to minimize side effects and suppression of adrenal function.
TAPERING
Corticosteroid
dosages are reduced gradually (tapered) to allow normal adrenal function to
return and to prevent steroid-induced adrenal insufficiency. Up to 1 year or
more after use of corticosteroids, the patient is still at risk for adrenal
insufficiency in times of stress. For example, if surgery for any reason is
necessary, the patient is likely to require intravenous corticosteroids during
and after surgery to reduce the risk for acute adrenal crisis. Patients
re-ceiving corticosteroids must have an adequate supply of medica-tion on hand,
so that they do not miss a scheduled dose and increase their risk for adrenal
insufficiency. Table 42-5 provides an overview of the effects of corticosteroid
therapy and their nurs-ing implications.
Related Topics