Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Nursing Process: The Patient With CushingŌĆÖs Syndrome
NURSING
PROCESS: THE PATIENT WITHCUSHINGŌĆÖS SYNDROME
Assessment
The
health history and examination focus on the effects on the body of high
concentrations of adrenal cortex hormones and on the inability of the adrenal
cortex to respond to changes in cortisol and aldosterone levels. The history
includes informa-tion about the patientŌĆÖs level of activity and ability to
carry out routine and self-care activities. The skin is observed and as-sessed
for trauma, infection, breakdown, bruising, and edema. Changes in physical
appearance are noted, and the patientŌĆÖs re-sponses to these changes are
elicited. The nurse assesses the patientŌĆÖs mental function, including mood,
responses to ques-tions, awareness of environment, and level of depression. The
family is often a good source of information about gradual changes in the
patientŌĆÖs physical appearance as well as emo-tional status.
Diagnosis
NURSING DIAGNOSES
Based
on all the assessment data, the major nursing diagnoses of the patient with
CushingŌĆÖs syndrome include the following:
┬Ę Risk for injury related
to weakness
┬Ę Risk for infection
related to altered protein metabolism and inflammatory response
┬Ę Self-care deficit
related to weakness, fatigue, muscle wast-ing, and altered sleep patterns
┬Ę Impaired skin integrity
related to edema, impaired healing, and thin and fragile skin
┬Ę Disturbed body image
related to altered physical appear-ance, impaired sexual functioning, and
decreased activity level
┬Ę Disturbed thought
processes related to mood swings, irri-tability, and depression
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on assessment data, potential complications may include the following:
┬Ę Addisonian crisis
┬Ę Adverse effects of
adrenocortical activity
Planning and Goals
The
major goals for the patient include decreased risk for injury, decreased risk
for infection, increased ability to carry out self-care activities, improved
skin integrity, improved body image, im-proved mental function, and absence of
complications.
Nursing Interventions
DECREASING RISK FOR INJURY
Establishing
a protective environment will help to prevent falls, fractures, and other
injuries to bones and soft tissues. The patient who is very weak may require
assistance from the nurse in ambu-lating to prevent falls or bumping into sharp
corners of furniture. Foods high in protein, calcium, and vitamin D are
recommended to minimize muscle wasting and osteoporosis. Referral to a
di-etitian may assist the patient in selecting appropriate foods that are also
low in sodium and calories.
DECREASING RISK FOR INFECTION
The
patient should avoid unnecessary exposure to others with infections. The nurse
frequently assesses the patient for subtle signs of infection because the
anti-inflammatory effects of cor-ticosteroids may mask the common signs of
inflammation and infection.
PREPARING THE PATIENT FOR SURGERY
The
patient is prepared for adrenalectomy, if indicated, and the postoperative
course. If CushingŌĆÖs syndrome is a result of a pituitary tumor, a
transsphe-noidal hypophysectomy may be performed. Dia-betes mellitus and peptic
ulcer are common in the patient with CushingŌĆÖs syndrome. Therefore, insulin
therapy and medication to treat peptic ulcer may be initiated if needed.
Before, during, and after surgery, blood glucose monitoring and assessment of stools
for blood are carried out to monitor for appropriate inter-vention. If the
patient has other symptoms of CushingŌĆÖs syn-drome, these are considered in the
preoperative preparation. For example, if the patient has experienced weight
gain, special in-struction is given about postoperative breathing exercises.
ENCOURAGING REST AND ACTIVITY
Weakness,
fatigue, and muscle wasting make it difficult for the patient with CushingŌĆÖs
syndrome to carry out normal activities. Yet the nurse should encourage
moderate activity to prevent com-plications of immobility and promote increased
self-esteem. In-somnia often contributes to the patientŌĆÖs fatigue. It is
important to help the patient plan and space rest periods throughout the day.
Efforts are made to promote a relaxing, quiet environment for rest and sleep.
PROMOTING SKIN INTEGRITY
Meticulous
skin care is necessary to avoid traumatizing the pa-tientŌĆÖs fragile skin. Use
of adhesive tape is avoided because it can irritate the skin and tear the
fragile tissue when the tape is re-moved. The nurse frequently assesses the
skin and bony promi-nences and encourages and assists the patient to change
positions frequently to prevent skin breakdown.
IMPROVING BODY IMAGE
If the
cause of CushingŌĆÖs syndrome can be treated successfully, the major physical
changes disappear in time. The patient may benefit from discussion of the
effect the changes have had on his or her self-concept and relationships with
others. Weight gain and edema may be modified by a low-carbohydrate, low-sodium
diet, and a high-protein intake may reduce some of the other bothersome
symptoms.
IMPROVING THOUGHT PROCESSES
Explanations
to the patient and family members about the cause of emotional instability are
important in helping them cope with the mood swings, irritability, and
depression that may occur. Psy-chotic behavior may occur in a few patients and
should be re-ported. The nurse encourages the patient and family members to
verbalize their feelings and concerns.
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
Addisonian Crisis
The
patient with CushingŌĆÖs syndrome whose symptoms are treated by withdrawing
corticosteroids, by adrenalectomy, or by removing a pituitary tumor is at risk
for adrenal hypofunction and addisonian crisis. If high levels of circulating
adrenal hor-mones have suppressed the function of the adrenal cortex, atro-phy
of the adrenal cortex is likely. If the circulating hormone level is decreased
rapidly because of surgery or by abruptly stop-ping corticosteroid agents,
manifestations of adrenal hypofunc-tion and addisonian crisis may develop.
Therefore, the patient with CushingŌĆÖs syndrome is monitored closely for
hypotension; rapid, weak pulse; rapid respiratory rate; pallor; and extreme
weakness. Efforts are made to identify factors that may have led to the crisis.
The
patient with CushingŌĆÖs syndrome who experiences highly stressful events, such
as trauma or emergency surgery, is at in-creased risk for addisonian crisis
because of long-term suppression of the adrenal cortex. The patient may require
intravenous ad-ministration of fluid and electrolytes and corticosteroids
before, during, and after treatment or surgery. If addisonian crisis oc-curs,
the patient is treated for circulatory collapse and shock.
Adverse Effects of Adrenocortical Activity
The
nurse assesses fluid and electrolyte status by monitoring laboratory values and
daily weights. Because of the increased risk for glucose intolerance and
hyperglycemia, blood glucose monitoring is initiated. The nurse reports
elevated blood glu-cose levels to the physician so that treatment can be
prescribed if indicated.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
patient with CushingŌĆÖs syndrome and the patientŌĆÖs family require teaching and
support to enable them to prevent problems associated with the syndrome and to
manage those that cannot be prevented. The nurse presents information verbally
and in writing. If the disorder is a result of corticosteroid use for
treat-ment of a chronic disease, the patient and family need to under-stand
that stopping the corticosteroid use abruptly and without medical supervision
is likely to result in acute adrenal insuffi-ciency and reappearance of the
underlying symptoms of the chronic disease. The nurse emphasizes the need to
ensure an ad-equate supply of the corticosteroid, because running out of the
medication and skipping doses can precipitate addisonian crisis. Refer to the
later discussion, Therapeutic Uses of Corticosteroids, for more information.
The
nurse stresses the need for dietary modifications to ensure adequate calcium
intake without increasing the risk for hyper-tension, hyperglycemia, and weight
gain. The patient and family may be taught to monitor blood pressure, blood
glucose levels, and weight. Wearing a medical alert bracelet and notifying
other health providers (eg, dentist) are important to alert others that the
patient has CushingŌĆÖs syndrome (Chart 42-11).
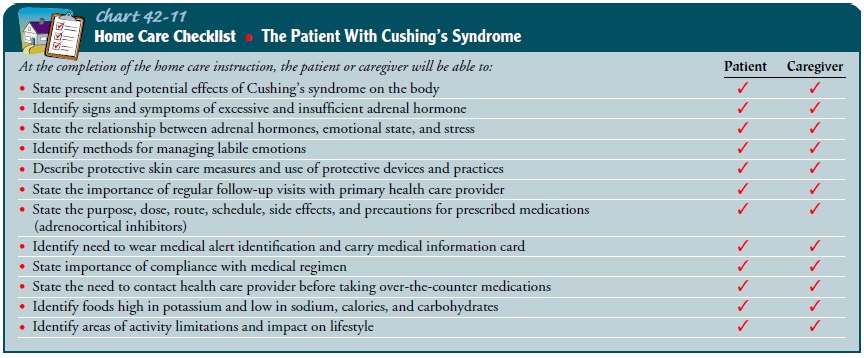
Continuing Care
The
need for follow-up depends on the origin and duration of the disease and its
management. The patient who has been treated by adrenalectomy or removal of a
pituitary tumor requires close monitoring to ensure that adrenal function has
returned to nor-mal and to ensure adequacy of circulating adrenal hormones. The
patient who requires continued corticosteroid therapy is moni-tored to ensure
understanding of the medications and the need for a dosage that treats the
underlying disorder while minimizing the side effects. Home care referral may
be indicated to ensure a safe environment that minimizes stress and risk for
falls and other side effects. The home care nurse assesses the patientŌĆÖs
physical and psychological status and reports changes to the physician. The
nurse also assesses the patientŌĆÖs understanding of the med-ication regimen and
the patientŌĆÖs compliance with the regimen, and reinforces previous teaching
about the medications and the importance of taking them as prescribed. The
nurse emphasizes the importance of regular medical follow-up, the side effects
and toxic effects of medications, and the need to wear medical iden-tification
with AddisonŌĆÖs and CushingŌĆÖs disease. Additionally, the nurse reminds the
patient and family about the importance of health promotion activities and
recommended health screening, including bone mineral density testing.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Decreases risk for
injury
a)
Is free of fractures or soft tissue injuries
b)
Is free of ecchymotic areas
2) Decreases risk for
infection
a)
Experiences no temperature elevation, redness,
pain, or other signs of infection and inflammation
b) Avoids contact with others who have infections
3) Increases participation
in self-care activities
a)
Plans activities and exercises to allow alternating
peri-ods of rest and activity
b)
Reports improved well-being
c)
Is free of complications of immobility
4) Attains/maintains skin
integrity
a)
Has intact skin, without evidence of breakdown or
infection
b)
Exhibits decreased edema in extremities and trunk
c)
Changes position frequently and inspects bony
promi-nences daily
5) Achieves improved body
image
a)
Verbalizes feelings about changes in appearance,
sexual function, and activity level
b)
States that physical changes are a result of
excessive corticosteroids
6) Exhibits improved mental
functioning
7) Absence of complications
a)
Exhibits normal vital signs and weight and is free
of symptoms of addisonian crisis
b)
Identifies signs and symptoms of adrenocortical
hypo-function that should be reported and measures to take in case of severe
illness and stress
c)
Identifies strategies to minimize complications of
CushingŌĆÖs syndrome
d)
Complies with recommendations for follow-up
appoint-ments and health screening.
Related Topics