Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
CushingŌĆÖs Syndrome - Management of Patients With Adrenal Disorders
CUSHINGŌĆÖS
SYNDROME
CushingŌĆÖs
syndrome results from excessive, rather than deficient, adrenocortical
activity. The syndrome may result from excessive administration of
corticosteroids or ACTH or from hyperplasia of the adrenal cortex.
Pathophysiology
CushingŌĆÖs
syndrome is commonly caused by use of corticosteroid medications and is
infrequently due to excessive corticosteroid pro-duction by the adrenal cortex
(Tierney et al., 2001). However, overproduction of endogenous corticosteroids
may be caused by several mechanisms, including a tumor of the pituitary gland
that produces ACTH and stimulates the adrenal cortex to increase its hormone
secretion despite adequate amounts being produced. Primary hyperplasia of the
adrenal glands in the absence of a pi-tuitary tumor is less common. Another
less common cause of CushingŌĆÖs syndrome is the ectopic production of ACTH by
ma-lignancies; bronchogenic carcinoma is the most common type of these
malignancies. Regardless of the cause, the normal feedback mechanisms that
control the function of the adrenal cortex be-come ineffective, and the usual
diurnal pattern of cortisol is lost.
The
signs and symptoms of CushingŌĆÖs syndrome are primarily a result of
oversecretion of glucocorticoids and androgens (sex hor-mones), although
mineralocorticoid secretion also may be affected.
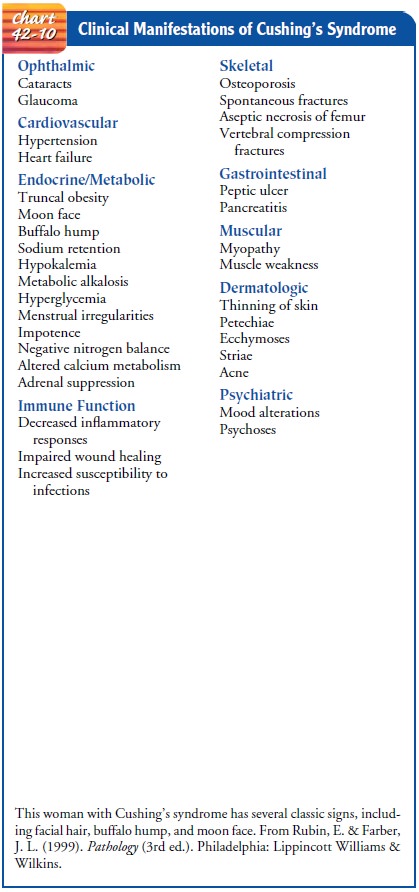
Clinical Manifestations
When
overproduction of the adrenal cortical hormone occurs, ar-rest of growth,
obesity, and musculoskeletal changes occur along with glucose intolerance. The
classic picture of CushingŌĆÖs syn-drome in the adult is that of central-type
obesity, with a fatty ŌĆ£buffalo humpŌĆØ in the neck and supraclavicular areas, a
heavy trunk, and relatively thin extremities. The skin is thin, fragile, and
easily traumatized; ecchymoses (bruises) and striae develop. The patient
complains of weakness and lassitude. Sleep is disturbed because of altered
diurnal secretion of cortisol.
Excessive
protein catabolism occurs, producing muscle wast-ing and osteoporosis.
Kyphosis, backache, and compression frac-tures of the vertebrae may result.
Retention of sodium and water occurs as a result of increased mineralocorticoid
activity, produc-ing hypertension and heart failure.
The
patient develops a ŌĆ£moon-facedŌĆØ appearance and may ex-perience increased oiliness
of the skin and acne. There is increased susceptibility to infection.
Hyperglycemia or overt diabetes may develop. The patient may also report weight
gain, slow healing of minor cuts, and bruises.
Women
ages 20 to 40 years are five times more likely than men to develop CushingŌĆÖs
syndrome. In females of all ages, viril-ization may occur as a result of excess
androgens. Virilization is characterized by the appearance of masculine traits
and the re-cession of feminine traits. There is an excessive growth of hair on
the face (hirsutism), the breasts atrophy, menses cease, the clitoris enlarges,
and the voice deepens. Libido is lost in men and women.
Changes
occur in mood and mental activity; psychosis may develop. Distress and
depression are common and are increased by the severity of the physical changes
that occur with this syn-drome. If CushingŌĆÖs syndrome is a consequence of
pituitary tumor, visual disturbances may occur because of pressure of the
growing tumor on the optic chiasm. Chart 42-10 summarizes the changes
associated with CushingŌĆÖs syndrome.
Assessment and Diagnostic Findings
Indicators
of CushingŌĆÖs syndrome include an increase in serum sodium and blood glucose
levels and a decreased serum concen-tration of potassium, a reduction in the
number of blood eosinophils, and disappearance of lymphoid tissue.
Measure-ments of plasma and urinary cortisol levels are obtained. Several blood
samples may be collected to determine whether the normal diurnal variation in
plasma levels is present; this variation is fre-quently absent in adrenal
dysfunction. If several blood samples are required, they must be collected at
the times specified and the time of collection must be noted on the requisition
slip.
An
overnight dexamethasone suppression test is the most widely used screening test
for diagnosis of pituitary and adrenal causes of CushingŌĆÖs syndrome. It can be
performed on an outpa-tient basis. Dexamethasone (1 mg) is administered orally
at 11 pm, and a plasma cortisol level is obtained at 8 the next morn-ing.
Suppression of cortisol to less than 5 mg/dL indicates that the
hypothalamic-pituitary-adrenal axis is functioning properly. Stress, obesity,
depression, and medications such as antiseizure agents, estrogen, and rifampin
can falsely elevate cortisol levels. Other diagnostic studies include a 24-hour
urinary free cortisol level and a high-dose or low-dose dexamethasone
suppression test. High-dose and low-dose suppression tests are similar to the
overnight test but vary in dosage and timing.
Measurement
of plasma ACTH by radioimmunoassay is used in conjunction with the high-dose
suppression test to distinguish pituitary tumors from ectopic sites of ACTH
production as the cause of CushingŌĆÖs syndrome. Elevation of both ACTH and
cor-tisol level indicates pituitary or hypothalamic disease. Low ACTH with a
high cortisol level indicates adrenal disease. A CT scan, ultrasound, or MRI
may be performed to localize adrenal tissue and detect tumors of the adrenal
gland.
Medical Management
If
CushingŌĆÖs syndrome is caused by pituitary tumors rather than tumors of the
adrenal cortex, treatment is directed at the pituitary gland. Surgical removal
of the tumor by transsphenoidal hypo-physectomy is the treatment of choice and
has a 90% success rate (Rakel & Bope, 2001). Radiation of the pitu-itary
gland also has been successful, although it may take several months for control
of symptoms. Adrenalectomy is the treatment of choice in patients with primary
adrenal hypertrophy.
Postoperatively,
symptoms of adrenal insufficiency may begin to appear 12 to 48 hours after
surgery because of reduction of the high levels of circulating adrenal
hormones. Temporary replace-ment therapy with hydrocortisone may be necessary for
several months until the adrenal glands begin to respond normally to the bodyŌĆÖs
needs. If both adrenal glands have been removed (bilateral adrenalectomy),
lifetime replacement of adrenal cortex hormones is necessary.
Adrenal
enzyme inhibitors (eg, metyrapone, aminoglutethi-mide, mitotane, ketoconazole)
may be used to reduce hyper-adrenalism if the syndrome is caused by ectopic
ACTH secretion by a tumor that cannot be eradicated. Close monitoring is
neces-sary because symptoms of inadequate adrenal function may result and
because of possible side effects of these medications.
If
CushingŌĆÖs syndrome is a result of the administration of cor-ticosteroids, an
attempt is made to reduce or taper the medica-tion to the minimum dosage needed
to treat the underlying disease process (eg, autoimmune and allergic diseases
and rejec-tion of transplanted organs). Frequently, alternate-day therapy
decreases the symptoms of CushingŌĆÖs syndrome and allows re-covery of the
adrenal glandsŌĆÖ responsiveness to ACTH.
Related Topics