Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Hypoparathyroidism - Management of Patients With Parathyroid Disorders
HYPOPARATHYROIDISM
The
most common cause of hypoparathyroidism is inadequate secretion of parathyroid
hormone after interruption of the blood supply or surgical removal of
parathyroid gland tissue during thy-roidectomy, parathyroidectomy, or radical
neck dissection. Atro-phy of the parathyroid glands of unknown cause is a less
common cause of hypoparathyroidism.
Pathophysiology
Symptoms
of hypoparathyroidism are caused by a deficiency of parathormone that results
in elevated blood phosphate (hyper-phosphatemia) and decreased blood calcium
(hypocalcemia) lev-els. In the absence of parathormone, there is decreased
intestinal absorption of dietary calcium and decreased resorption of cal-cium
from bone and through the renal tubules. Decreased renal excretion of phosphate
causes hypophosphaturia, and low serum calcium levels result in hypocalciuria.
Clinical Manifestations
Hypocalcemia causes irritability of the neuromuscular system and contributes to the chief symptom of hypoparathyroidism—tetany. Tetany is a general muscle hypertonia, with tremor and spasmodic or uncoordinated contractions occurring with or without efforts to make voluntary movements. Symptoms of latent tetany are numbness, tingling, and cramps in the extremities, and the patient complains of stiffness in the hands and feet.
In overt tetany, the signs
include bronchospasm, laryngeal spasm, carpopedal spasm (flexion of the elbows
and wrists and extension of the carpopha-langeal joints), dysphagia,
photophobia, cardiac dysrhythmias, and seizures. Other symptoms include
anxiety, irritability, de-pression, and even delirium. ECG changes and
hypotension also may occur.
Assessment and Diagnostic Findings
A
positive Trousseau’s sign or a positive Chvostek’s sign suggests latent tetany.
Trousseau’s sign is positive when
carpopedal spasm is induced by occluding the blood flow to the arm for 3
minutes with a blood pressure cuff. Chvostek’s
sign is positive when a sharp tapping over the facial nerve just in front
of the parotid gland and anterior to the ear causes spasm or twitching of the
mouth, nose, and eye.
The
diagnosis of hypoparathyroidism often is difficult because of the vague
symptoms, such as aches and pains. Therefore, lab-oratory studies are
especially helpful. Tetany develops at serum calcium levels of 5 to 6 mg/dL
(1.2 to 1.5 mmol/L) or lower. Serum phosphate levels are increased, and x-rays
of bone show in-creased density. Calcification is detected on x-rays of the
sub-cutaneous or paraspinal basal ganglia of the brain.
Medical Management
The
goal of therapy is to raise the serum calcium level to 9 to 10 mg/dL (2.2 to
2.5 mmol/L) and to eliminate the symptoms of hypoparathyroidism and
hypocalcemia. When hypocalcemia and tetany occur after a thyroidectomy, the
immediate treat-ment is to administer calcium gluconate intravenously. If this
does not decrease neuromuscular irritability and seizure activ-ity immediately,
sedative agents such as pentobarbital may be administered.
Parenteral
parathormone can be administered to treat acute hypoparathyroidism with tetany.
The high incidence of allergic re-actions to injections of parathormone,
however, limits its use to acute episodes of hypocalcemia. The patient
receiving parathor-mone is monitored closely for allergic reactions and changes
in serum calcium levels.
Because
of neuromuscular irritability, the patient with hypocalcemia and tetany
requires an environment that is free ofnoise, drafts, bright lights, or sudden
movement. Tracheostomy or mechanical ventilation may become necessary, along
with bronchodilating medications, if the patient develops respiratory distress.
Therapy
for the patient with chronic hypoparathyroidism is determined after serum
calcium levels are obtained. A diet high in calcium and low in phosphorus is
prescribed. Although milk, milk products, and egg yolk are high in calcium,
they are restricted because they also contain high levels of phosphorus.
Spinach also is avoided because it contains oxalate, which would form
insolu-ble calcium substances. Oral tablets of calcium salts, such as cal-cium
gluconate, may be used to supplement the diet. Aluminum hydroxide gel or
aluminum carbonate (Gelusil, Amphojel) also is administered after meals to bind
phosphate and promote its excretion through the gastrointestinal tract.
Variable
dosages of a vitamin D preparation—dihydrotachys-terol (AT 10 or Hytakerol),
ergocalciferol (vitamin D), cholecal-ciferol (vitamin D)—are usually required
and enhance calcium absorption from the gastrointestinal tract.
Nursing Management
Nursing
management of the patient with possible acute hypo-parathyroidism includes the
following:
· Care of postoperative
patients having thyroidectomy, para-thyroidectomy, and radical neck dissection
is directed toward detecting early signs of hypocalcemia and anticipat-ing
signs of tetany, seizures, and respiratory difficulties.
· Calcium gluconate is
kept at the bedside, with equipment necessary for intravenous administration.
If the patient has a cardiac disorder, is subject to dysrhythmias, or is
receiv-ing digitalis, calcium gluconate is administered slowly and cautiously.
· Calcium and digitalis
increase systolic contraction and also potentiate each other; this may produce
potentially fatal dysrhythmias. Consequently, the cardiac patient requires
continuous cardiac monitoring and careful assessment.
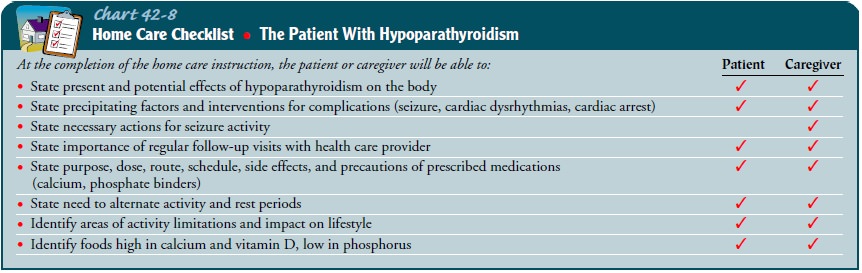
An important aspect of nursing care is teaching about med-ications and diet therapy. The patient needs to know the reason for high calcium and low phosphate intake and the symptoms of hypocalcemia and hypercalcemia; he or she should know to contact the physician immediately if these symptoms occur (Chart 42-8).
Related Topics