Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Hyperthyroidism - Management of Patients With Thyroid Disorders
HYPERTHYROIDISM
Hyperthyroidism
is the second most prevalent endocrine disor-der, after diabetes mellitus. Graves’ disease, the most common type
of hyperthyroidism, results from an excessive output of thy-roid hormones
caused by abnormal stimulation of the thyroid gland by circulating
immunoglobulins. It affects women eight times more frequently than men, with
onset usually between the second and fourth decades (Tierney et al., 2001). It
may appear after an emotional shock, stress, or an infection, but the exact
sig-nificance of these relationships is not understood. Other common causes of
hyperthyroidism include thyroiditis and excessive in-gestion of thyroid
hormone.
Clinical Manifestations
Patients
with well-developed hyperthyroidism exhibit a charac-teristic group of signs
and symptoms (sometimes referred to as thyrotoxicosis).
The presenting symptom is often nervousness.These patients are often
emotionally hyperexcitable, irritable, and apprehensive; they cannot sit
quietly; they suffer from pal-pitations; and their pulse is abnormally rapid at
rest as well as on exertion. They tolerate heat poorly and perspire unusually
freely. The skin is flushed continuously, with a characteristic salmon color,
and is likely to be warm, soft, and moist. Elderly patients, however, may
report dry skin and diffuse pruritus. A fine tremor of the hands may be
observed. Patients may exhibit exophthalmos
(bulging eyes), which produces a startled facialexpression.
Other
manifestations include an increased appetite and di-etary intake, progressive
weight loss, abnormal muscular fatiga-bility and weakness (difficulty in
climbing stairs and rising from a chair), amenorrhea, and changes in bowel
function. The pulse rate ranges constantly between 90 and 160 beats/min; the
sys-tolic, but characteristically not the diastolic, blood pressure is
elevated; atrial fibrillation may occur; and cardiac decompen-sation in the
form of heart failure is common, especially in el-derly patients. Osteoporosis
and fracture are also associated with hyperthyroidism.
Cardiac
effects may include sinus tachycardia or dysrhyth-mias, increased pulse
pressure, and palpitations; it has been sug-gested that these changes may be related
to increased sensitivity to catecholamines or to changes in neurotransmitter
turnover. Myocardial hypertrophy and heart failure may occur if the
hyper-thyroidism is severe and untreated.
The
course of the disease may be mild, characterized by re-missions and
exacerbations and terminating with spontaneous re-covery in a few months or
years. Conversely, it may progress relentlessly, with the untreated person
becoming emaciated, in-tensely nervous, delirious, and even disoriented;
eventually, the heart fails.
Symptoms
of hyperthyroidism may occur with the release of excessive amounts of thyroid
hormone as a result of inflamma-tion after irradiation of the thyroid or
destruction of thyroid tis-sue by tumor. Such symptoms may also occur with
excessive administration of thyroid hormone for treatment of hypothy-roidism.
Long-standing use of thyroid hormone in the absence of close monitoring may be
a cause of symptoms of hyperthy-roidism. It is also likely to result in
premature osteoporosis, par-ticularly in women.
Assessment and Diagnostic Findings
The thyroid gland invariably is enlarged to
some extent. It is soft and may pulsate; a thrill often can be palpated, and a
bruit is heard over the thyroid arteries. These are signs of greatly in-creased
blood flow through the thyroid gland. In advanced cases, the diagnosis is made
on the basis of the symptoms and an in-crease in serum T4 and an
increased 123I or 125I uptake by the thy-roid in excess
of 50%.
Gerontologic Considerations
Although
hyperthyroidism is much less common in elderly peo-ple than hypothyroidism,
patients older than 60 years account for 10% to 15% of the cases of
thyrotoxicosis. Although some older patients develop typical signs and symptoms
of thyrotoxicosis, in most an atypical picture is present, which is often
subclinical (Toft, 2001).
Elderly
patients commonly present with vague and nonspecific signs and symptoms, making
disorders hard to detect. Symptoms such as tachycardia, fatigue, mental
confusion, weight loss, change in bowel habits, and depression can be
attributed to age and other illnesses common to elderly people. In addition,
the patient may report cardiovascular symptoms and difficulty climbing stairs
or rising from a chair because of muscle weakness. New or worsen-ing heart failure
or angina is more likely to occur in elderly than in younger patients. The
elderly patient may experience a single man-ifestation, such as atrial
fibrillation, anorexia, or weight loss. These signs and symptoms may mask the
underlying thyroid disease.
Spontaneous
remission of hyperthyroidism is rare in elderly patients. Measurement of TSH is
indicated in elderly patients with unexplained physical or mental
deterioration.
Medical Management
Treatment
of hyperthyroidism is directed toward reducing thy-roid hyperactivity to
relieve symptoms and remove the cause of important complications. Treatment
depends on the cause of the hyperthyroidism and may require a combination of
therapeutic approaches.
PHARMACOLOGIC THERAPY
Two
forms of pharmacotherapy are available for treating hyper-thyroidism and
controlling excessive thyroid activity: (1) use of irradiation by
administration of the radioisotope 123I or 131I for destructive effects on the thyroid
gland and (2) antithyroid med-ications that interfere with the synthesis of
thyroid hormones and other agents that control manifestations of
hyperthyroidism. Sur-gical removal of most of the thyroid gland is a
nonpharmacologic alternative.
Radioactive Iodine Therapy.
The goal of radioactive iodine ther-apy
(123I or 131I) is to destroy the overactive thyroid
cells. Use of radioactive iodine is the most common treatment in elderly
pa-tients. Almost all the iodine that enters and is retained in the body
becomes concentrated in the thyroid gland. Therefore, the radio-active isotope
of iodine is concentrated in the thyroid gland, where it destroys thyroid cells
without jeopardizing other radiosensitive tissues. Over a period of several
weeks, thyroid cells exposed to the radioactive iodine are destroyed, resulting
in reduction of the hyperthyroid state and inevitably hypothyroidism.
The
patient is instructed about what to expect with this taste-less, colorless
radioiodine, which may be administered by the radi-ologist. A single oral dose
of the agent is administered, based on 80 to 160 ÎĽCi/g estimated thyroid
weight. About 70% to 85% of pa-tients are cured by one dose of radioactive
iodine. An additional 10% to 20% require two doses; rarely is a third dose
necessary. Use of an ablative dose of radioactive iodine initially causes an
acute re-lease of thyroid hormone from the thyroid gland and may cause an
increase of symptoms. The patient is observed for signs of thyroidstorm; propranolol is useful in controlling these symptoms.
After
treatment with radioactive iodine, the patient is followed closely until the
euthyroid state is reached. In 3 to 4 weeks, symptoms of hyperthyroidism
subside. Because the incidence of hypo-thyroidism after this form of treatment
is very high (ie, more than 90% at 10 years), close follow-up is required to
evaluate thyroid function. Thyroid hormone replacement is necessary; small
doses are usually prescribed, with the dose gradually increased over a period
of months (up to about 1 year) until the FT4 and TSH lev-els stabilize within normal ranges.
Radioactive
iodine has been used to treat toxic adenomas and multinodular goiter and most
varieties of thyrotoxicosis (rarely per-manently successful); it is preferred
for treating patients beyond the childbearing years with diffuse toxic goiter.
It is contraindicated in pregnancy and in nursing mothers because radioiodine
crosses the placenta and is secreted in breast milk. A major advantage of
treat-ment with radioactive iodine is that it avoids many of the side ef-fects
associated with antithyroid medications. However, many patients and their
families fear medications that are radioactive. Be-cause of this fear, many
patients elect to take antithyroid medica-tions rather than radioactive iodine.
Gerontologic Considerations
The
use of radioactive iodine is generally recommended for treatment of
thyrotoxicosis in elderly patients unless an enlarged thyroid gland is pressing
on the airway. The hypermetabolic state of thyrotoxicosis must be controlled by
antithyroid medications before radioactive iodine is administered because
radiation may precipitate thyroid storm by increasing the release of hormone
from the thyroid gland. Thyroid storm, if it occurs, has a mortal-ity rate of
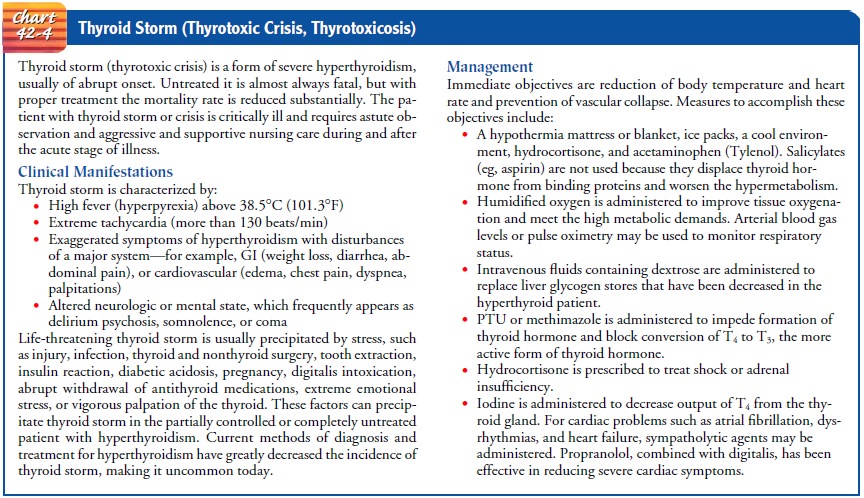
10% in elderly patients (Chart 42-4).
Antithyroid Medications.
The
objective of pharmacotherapy is toinhibit one or more stages in thyroid hormone
synthesis or hor-mone release; another goal may be to reduce the amount of
thy-roid tissue, with resulting decreased thyroid hormone production.
Antithyroid
agents block the utilization of iodine by inter-fering with the iodination of
thyrosine and the coupling of iodothyrosines in the synthesis of thyroid
hormones. This pre-vents the synthesis of thyroid hormone. The most commonly
used medications are propylthiouracil (Propacil, PTU) or me-thimazole
(Tapazole) until the patient is euthyroid (ie, neither hyperthyroid nor
hypothyroid). These medications block ex-trathyroidal conversion of T4 to T3. Because antithyroid
med-ications do not interfere with release or activity of previously formed
thyroid hormones, it may take several weeks for relief of symptoms. At this
time the maintenance dose is established, fol-lowed by a gradual withdrawal of
the medication over the next several months.
Therapy
is determined on the basis of clinical criteria, includ-ing changes in pulse
rate, pulse pressure, body weight, size of the goiter, and results of
laboratory studies of thyroid function.
Toxic
complications of antithyroid medications are relatively uncommon; nevertheless,
the importance of periodic follow-up is emphasized because medication
sensitization, fever, rash, urti-caria, or even agranulocytosis and
thrombocytopenia (decrease in granulocytes and platelets) may develop. With any
sign of infec-tion, especially pharyngitis and fever or the occurrence of mouth
ulcers, the patient is advised to stop the medication, notify the physician
immediately, and undergo hematologic studies. Rash, arthralgias, and fever
occur in 5% of patients. Agranulocytosis, the most serious toxic side effect,
occurs in 1 of every 200 pa-tients. Its incidence is higher in patients older
than 40 years. It generally occurs within the first 3 months of therapy but may
occur up to 1 year after it is started.
Patients
taking antithyroid medications are instructed not to use decongestants for
nasal stuffiness because they are poorly tol-erated. Antithyroid medications
are contraindicated in late preg-nancy because they may produce goiter and
cretinism in the fetus.
Thyroid
hormone is occasionally administered with antithyroid medications to put the
thyroid gland at rest. In this approach, hypothyroidism from excess antithyroid
medication is avoided, as is stimulation of the thyroid gland by TSH. Thyroid
hormone is available as thyroglobulin (Proloid) and levothyroxine sodium
(Synthroid). These slow-acting preparations take about 10 days to achieve their
full effect. Liothyronine sodium (Cytomel) has a more rapid onset, and its
action is of short duration.
Gerontologic Considerations
If
antithyroid agents are used in elderly patients, the patient must be monitored
closely because elderly patients are more likely to de-velop granulocytopenia.
The dosage of other medications to treat other chronic illnesses in elderly
patients may need to be modified because of the altered rate of metabolism in
hyperthyroidism.
Adjunctive Therapy.
Iodine or
iodide compounds, once the onlytherapy available for patients with
hyperthyroidism, are no longer used as the sole method of treatment. Such
compounds decrease the release of thyroid hormones from the thyroid gland and
reduce the vascularity and size of the thyroid. Compounds such as potas-sium
iodide (KI), Lugol’s solution, and saturated solution of potas-sium iodide
(SSKI) may be used in combination with antithyroid agents or beta-adrenergic
blockers to prepare the patient with hyper-thyroidism for surgery. These agents
reduce the activity of the thy-roid hormone and the vascularity of the thyroid
gland, making the surgical procedure safer. Solutions of iodine and iodide
compounds are more palatable in milk or fruit juice and are administered
through a straw to prevent staining of the teeth. These compoundsreduce the metabolic
rate more rapidly than antithyroid medica-tions, but their action does not last
as long.
Beta-adrenergic blocking agents are important
in controlling the sympathetic nervous system effects of hyperthyroidism. For
example, propranolol (Inderal) is used to control nervousness, tachycardia,
tremor, anxiety, and heat intolerance. The patient continues taking propranolol
until the FT4
is within the normal range and the TSH level approaches normal.
Gerontologic Considerations
Use of
beta-adrenergic blocking agents (eg, propranolol [Inderal]) may be indicated to
decrease the cardiovascular and neurologic signs and symptoms of
thyrotoxicosis. These agents must be used with extreme caution in elderly
patients to minimize adverse effects on cardiac function that may produce heart
failure.
SURGICAL MANAGEMENT
Surgery to remove thyroid tissue was once the
primary method of treating hyperthyroidism; today, surgery is reserved for
spe-cial circumstances—for example, in pregnant women allergic to antithyroid
medications, patients with large goiters, or patients unable to take
antithyroid agents. Surgery for treatment of hyper-thyroidism is performed soon
after the thyroid function has re-turned to normal (4 to 6 weeks).
The
surgical removal of about five sixths of the thyroid tissue (subtotal
thyroidectomy) practically ensures a prolonged remis-sion in most patients with
exophthalmic goiter. Its use today is reserved for large goiters, presence of
obstructive symptoms, preg-nant women, or when there is a need for rapid
normalization of thyroid function (Argueta & Whitaker, 2000; Fatourechi,
2000). Before surgery, propylthiouracil is administered until signs of
hyperthyroidism have disappeared. A beta-adrenergic blocking agent
(propranolol) may be used to reduce the heart rate and other signs and symptoms
of hyperthyroidism; however, this does not create a euthyroid state. Iodine
(Lugol’s solution or potassium io-dide) may be prescribed in an effort to
reduce blood loss; however, the effectiveness of this is unknown. Patients
receiving iodine medication must be monitored for evidence of iodine toxicity
(iodism), which requires immediate withdrawal of the medication. Symptoms of
iodism include swelling of the buccal mucosa, ex-cessive salivation, coryza,
and skin eruptions.
Recurrent Hyperthyroidism
No
treatment for thyrotoxicosis is without side effects, and all three treatments
(radioactive iodine therapy, antithyroid med-ications, and surgery) share the
same complications: relapse or recurrent hyperthyroidism and permanent
hypothyroidism. The rate of relapse increases in patients who had very severe
disease, a long history of dysfunction, ocular and cardiac symptoms, large
goiter, and relapse after previous treatment. The relapse rate after
radioactive iodine therapy depends on the dose used in treatment. Patients
receiving a lower dose of radioactive iodine are more likely to require
subsequent treatment than those being treated with a higher dose.
Hypothyroidism occurs in almost 80% of pa-tients at 1 year and in 90% to 100%
by 5 years for both the mul-tiple low-dose and single high-dose methods.
Although
rates of relapse and the occurrence of hypothy-roidism vary, relapse with
antithyroid medications is about 45% by 1 year after completion of therapy and
almost 75% by 5 years later (Larson et al., 2000). Discontinuation of
antithyroid med-ications before therapy is complete usually results in relapse
within 6 months in most patients. The incidence of relapse with subtotal
thyroidectomy is 19% at 18 months; an incidence of hypothy-roidism of 25% has
been reported at 18 months after surgery. The risk for these complications
illustrates the importance of long-term follow-up of patients treated for
hyperthyroidism.
Related Topics