Chapter: Medical Surgical Nursing: Assessment of Renal and Urinary Tract Function
Anatomy of the Upper and Lower Urinary Tracts
ANATOMY
OF THE UPPER AND LOWER URINARY TRACTS
The
urinary system—the structures of which precisely maintain the internal chemical
environment of the body—perform various excretory, regulatory, and secretory
functions.
Kidneys
The
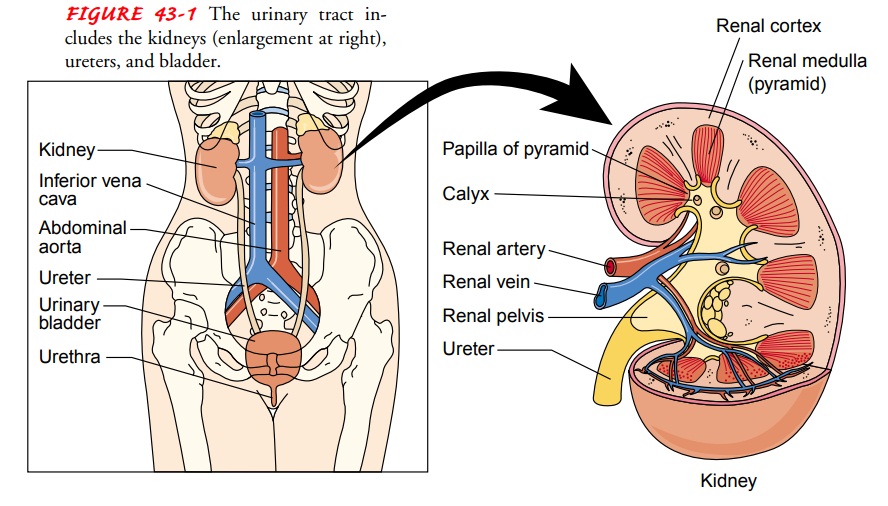
kidneys are a pair of brownish-red structures located retroperitoneally (behind
and outside the peritoneal cavity) on the posterior wall of the abdomen from
the 12th thoracic vertebra to the 3rd lumbar vertebra in the adult (Fig. 43-1).
An adult kidney weighs 120 to 170 g (about 4.5 oz) and is 12 cm (about 4.5
inches) long, 6 cm wide, and 2.5 cm thick. The kidneys are well protected by
the ribs, muscles, Gerota’s fascia, perirenal fat, and the renal capsule, which
surround each kidney.
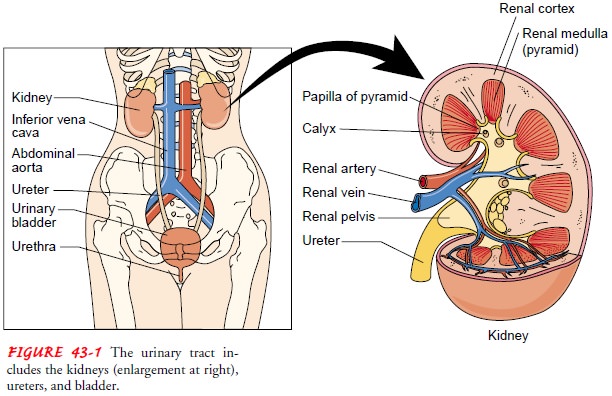
The
kidney consists of two distinct regions, the renal parenchyma and the renal
pelvis. The renal parenchyma is divided into the cortex and the medulla. The
cortex contains the glomeruli,proximal and distal tubules, and cortical
collecting ducts and their adjacent peritubular capillaries. The medulla
resembles conical pyramids. The pyramids are situated with the base facing the
concave surface of the kidney and the apex facing the hilum, or
pelvis.
Each kidney contains approximately 8 to 18 pyramids.The pyramids drain into 4
to 13 minor calices that, in turn, drain into 2 to 3 major calices that open
directly into the renal pelvis.
The
hilum, or pelvis, is the concave portion of the kidneythrough which the renal
artery enters and the renal vein exits. The renal artery (arising from the
abdominal aorta) divides into smaller and smaller vessels, eventually forming
the afferent arteriole. The afferent arteriole branches to form the glomerulus,
which is the capillary bed responsible for glomerular filtration. Blood leaves
the glomerulus through the efferent arteriole and flows back to the inferior
vena cava through a network of capillaries and veins.Each kidney contains about
1 million nephrons, the functional units of the kidney.
Each
kidney is capable of providing adequate renal function if the opposite kidney
becomes nonfunctional. The nephron consists of a glomerulus containing afferent
and efferent arterioles, Bowman’s capsule, proximal tubule, loop of Henle,
distal tubule, and collecting ducts (Fig. 43-2). Collecting ducts converge into
papillae, which empty into the minor calices, which drain into three major
calices that open directly into the renal pelvis.
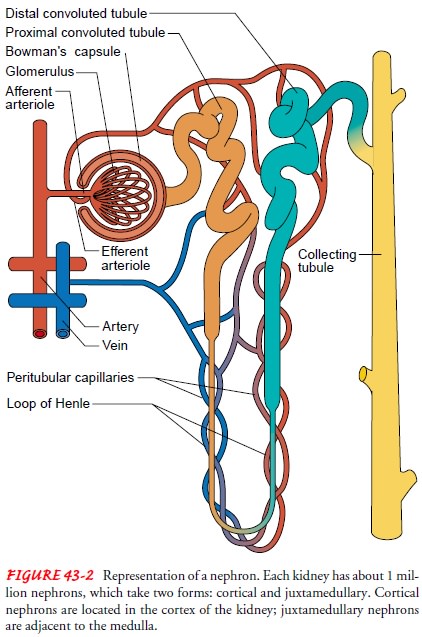
Nephrons
are structurally divided into two types: cortical an juxtamedullary. Cortical
nephrons are found in the cortex of the kidney, and juxtamedullary nephrons sit
adjacent to the medulla. The juxtamedullary nephrons are distinguished by their
long loops of Henle and the vasa recta, long capillary loops that dip into the
medulla of the kidney.
The
glomerulus is composed of three filtering layers: the capillary endothelium,
the basement membrane, and the epithelium.The glomerular membrane normally
allows filtration of fluid and small molecules yet limits passage of larger
molecules, such as blood cells and albumin. Kidney function begins to decrease
at a rate of approximately 1% each year beginning at approximately age 30.
Ureters, Bladder, and Urethra
Urine, which is formed within the nephrons, flows into the ureter, a long fibromuscular tube that connects each kidney to the bladder. The ureters are narrow, muscular tubes, each 24 to 30 cm long, that originate at the lower portion of the renal pelvis and terminate in the trigone of the bladder wall. There are three narrowed areas of each ureter: the ureteropelvic junction, the ureteral segment near the sacroiliac junction, and the ureterovesical junction.
The angling of the ureterovesical junction is the primary means of providing antegrade, or downward, movement of urine, also re-ferred to as efflux of urine. This angling prevents vesicoureteral reflux, which is the retrograde, or backward, movement of
urinefrom the bladder, up the ureter, toward the kidney. During void-ing (micturition), increased intravesical
pressure keeps the uretero-vesical junction closed and keeps urine within the
ureters. As soon as micturition is completed, intravesical pressure returns to
its nor-mal low baseline value, allowing efflux of urine to resume. There-fore,
the only time that the bladder is completely empty is in the last seconds of
micturition before efflux of urine resumes.
The
three areas of narrowing within the ureters have a propen-sity toward
obstruction because of renal calculi (kidney stones) or stricture. Obstruction
of the ureteropelvic junction is the most serious because of its close
proximity to the kidney and the risk of associated kidney dysfunction. The left
ureter is slightly shorter than the right. The lining of the ureters is made up
of transitional cell epithelium called urothelium. As in the bladder, the
urothe-lium prevents reabsorption of urine. The movement of urine from the
renal pelves through the ureters into the bladder is fa-cilitated by
peristaltic waves (occurring about one to five times per minute) from
contraction of the smooth muscle in the ureter wall (Walsh, Retik, Vaughan
& Wein, 1998).
The
urinary bladder is a muscular, hollow sac located just be-hind the pubic bone.
Adult bladder capacity is about 300 to 600 mL of urine. In infancy, the bladder
is found within the ab-domen. In adolescence and through adulthood, the bladder
as-sumes its position in the true pelvis. The bladder is characterized by its
central, hollow area called the vesicle, which has two inlets (the ureters) and
one outlet (the urethrovesical junction), which is surrounded by the bladder
neck. The wall of the bladder com-prises four layers. The outermost layer is
the adventitia, which is made up of connective tissue. Immediately beneath the
adventi-tia is a smooth muscle layer known as the detrusor. Beneath the
detrusor is a smooth muscle tunic known as the lamina propria, which serves as
an interface between the detrusor and the inner-most layer, the urothelium. The
urothelium layer is specialized, transitional cell epithelium, containing a
membrane that is im-permeable to water. The urothelium prevents the
reabsorption of urine stored in the bladder. The bladder neck contains bundles
of involuntary smooth muscle that form a portion of the urethral sphincter
known as the internal sphincter. The portion of the sphincteric mechanism that
is under voluntary control is the ex-ternal urinary sphincter at the anterior
urethra, the segment most distal from the bladder (Walsh et al., 1998).
The
urethra arises from the base of the bladder: In the male, it passes through the
penis; in the female, it opens just anterior to the vagina. In the male, the
prostate gland, which lies just below the bladder neck, surrounds the urethra
posteriorly and laterally.
Related Topics