Chapter: Medical Surgical Nursing: Assessment of Renal and Urinary Tract Function
Assessment of Renal and Urinary Tract Function
Assessment
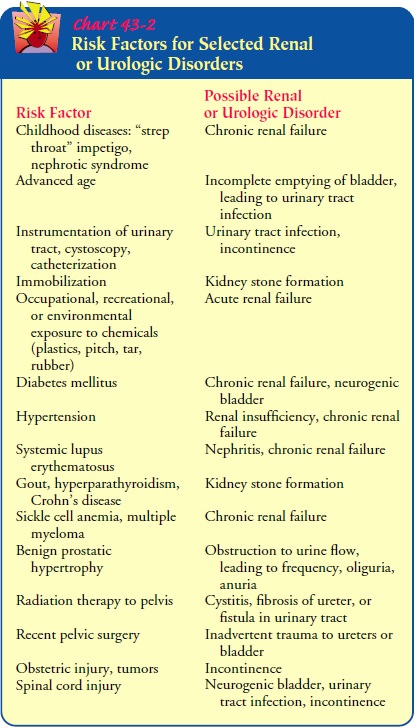
Obtaining
a comprehensive health history, which includes an assessment of risk factors,
is the first step in assessing a patient with upper or lower urinary tract
dysfunction. Various diseases or clinical situations can place a patient at
increased risk for urinary tract dysfunction. Data collection about previous
health problems or diseases provides the health care team with useful
information for evaluating the patient’s current urinary status. Risk factors
for specific disorders and kidney and lower urinary tract dysfunction are
discussed in Chart 43-2.
HEALTH HISTORY
Obtaining a urologic health history requires excellent communication skills because many patients are embarrassed or uncomfortable discussing genitourinary function or symptoms. It is important to use language the patient can understand and to avoid medical jargon. It is also important to review risk factors, particularly with those at risk. For example, the nurse needs to be aware that multiparous women delivering their children vaginally are at high risk for stress urinary incontinence, which if severe enough can also lead to urge incontinence. Elderly women and persons with neurologic disorders such as diabetic neuropathy, multiple sclerosis, or Parkinson’s disease often have incomplete emptying of the bladder with urinary stasis, which may result in urinary tract infection or increasing bladder pressure leading to overflow incontinence, hydronephrosis, pyelonephritis, or renal insufficiency.
Persons
with a family history of urinary tract problems are at increased risk for renal
disorders. Persons with diabetes who have consistent hypertension are at risk
for renal dysfunction (Bakris, Williams, Dworkin et al., 2000). Older men are
at risk for pros-tatic enlargement, which causes urethral obstruction and which
can result in urinary tract infections and renal failure (Degler, 2000).
Moreover, many persons with a history of systemic lupus erythematosus (SLE)
develop lupus nephritis (Smith, Fortune-Faulkner & Spurbeck, 2000). When
obtaining the health history, the nurse should inquire about the following:
·
The patient’s chief concern or reason for seeking
health care, the onset of the problem, and its effect on the patient’s quality
of life
·
The location, character, and duration of pain, if
present, and its relationship to voiding; factors that precipitate pain, and
those that relieve it
·
History of urinary tract infections, including past
treatment or hospitalization for urinary tract infection
·
Fever or chills
·
Previous renal or urinary diagnostic tests or use
of indwelling urinary catheters
· Dysuria and when it occurs during voiding (at
initiation ortermination of voiding)
· Hesitancy, straining, or
pain during or after urination
· Urinary incontinence
(stress incontinence, urge inconti-nence, overflow incontinence, or functional
incontinence)
· Hematuria or change in
color or volume of urine
· Nocturia and its date of onset
· Renal calculi (kidney
stones), passage of stones or gravel in urine
· Female patients: number
and type (vaginal or cesarean) of deliveries; use of forceps; vaginal
infection, discharge, or irritation; contraceptive practices
·
Presence or history of genital lesions or sexually
transmitted diseases
· Habits: use of tobacco,
alcohol, or recreational drugs
· Any prescription and
over-the-counter medications (includ-ing those prescribed for renal or urinary
problems)
Gerontologic Considerations
A
thorough medication history is especially important for elderly patients, for
whom the increased occurrence of chronic illness often necessitates
polypharmacy (concurrent use of multiple med-ications). Aging affects the way
the body absorbs, metabolizes,and excretes drugs, thus placing the elderly
patient at risk for ad-verse reactions, including compromised renal function.
Other
key information to obtain while gathering the health history includes an
assessment of the patient’s psychosocial sta-tus, level of anxiety, perceived
threats to body image, available support systems, and sociocultural patterns.
Obtaining this in-formation during the initial and subsequent nursing
assessments enables the nurse to uncover special needs, misunderstandings, lack
of knowledge, and need for patient teaching. Pain, changes in voiding, and
gastrointestinal symptoms are particularly sug-gestive of urinary tract
disease. Dysfunction of the kidney can produce a complex array of symptoms
throughout the body.
Unexplained Anemia
Gradual kidney dysfunction can be insidious in its presentation, al-though fatigue is a common symptom. Fatigue, shortness of breath, and exercise intolerance all result from the condition known as “anemia of chronic disease.” Although hematocrit has been the blood test of choice when assessing a patient for anemia, the 2001 Kidney Disease Outcomes Quality Initiative: Management of Ane-mia Guidelines recommend that anemia be quantified using he-moglobin level rather than hematocrit, because that measurement is a better assessment of circulating oxygen (Eschbach, 2001).
Pain
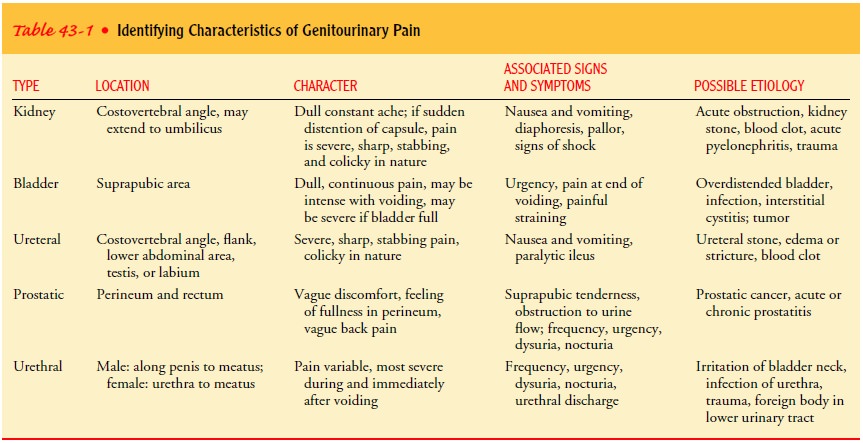
Genitourinary
pain is usually caused by distention of some por-tion of the urinary tract
because of obstructed urine flow or in-flammation and swelling of tissues.
Severity of pain is related to the sudden onset rather than the extent of
distention.
Table
43-1 lists the various types of genitourinary pain, char-acteristics of the
pain, associated signs and symptoms, and possi-ble causes. However, kidney
disease does not always involve pain. It tends to be diagnosed because of other
symptoms that cause a patient to seek health care, such as pedal edema,
shortness of breath, and changes in urine elimination (Kuebler, 2001).
Changes in Voiding
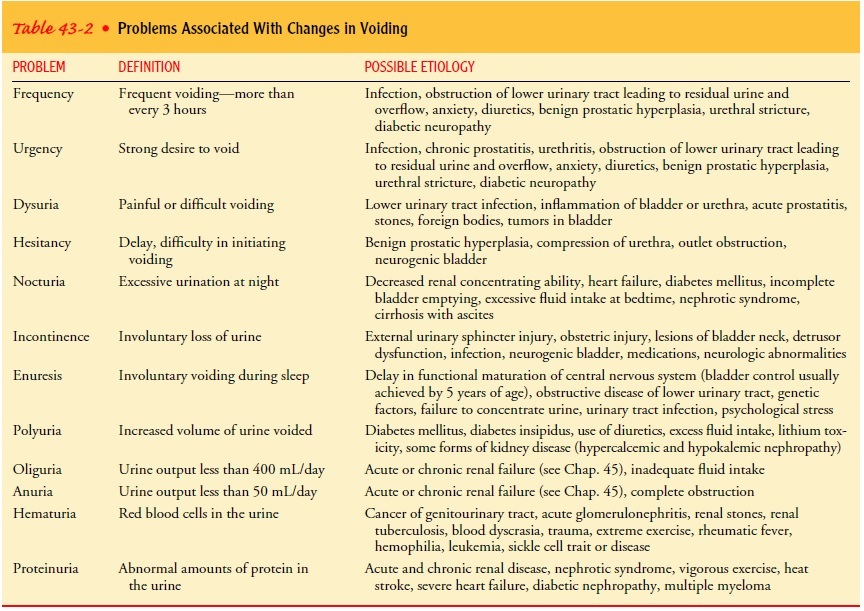
Voiding
(micturition) is normally a painless function occurring ap-proximately eight
times in a 24-hour period. The average person voids 1,200 to 1,500 mL of urine
in 24 hours, although this amount varies depending on fluid intake, sweating,
environmental temper-ature, vomiting, or diarrhea. Common problems associated
with voiding include frequency,
urgency, dysuria, hesitancy, inconti-nence, enuresis, polyuria, oliguria, and hematuria. These problems
and others are described in Table 43-2. Increased urinary urgency and frequency
coupled with decreasing urine volumes strongly sug-gest urine retention.
Depending on the acuity of the onset of these symptoms, immediate bladder
emptying via catheterization and evaluation are necessary to prevent kidney
dysfunction (Gray, 2000a).
Gastrointestinal Symptoms
Gastrointestinal
symptoms may occur with urologic conditions because of shared autonomic and
sensory innervation and reno-intestinal reflexes. The anatomic relation of the
right kidney to the colon, duodenum, head of the pancreas, common bile duct,
liver, and gallbladder may cause gastrointestinal disturbances. The prox-imity
of the left kidney to the colon (splenic flexure), stomach,pancreas, and spleen
may also result in intestinal symptoms. The most common signs and symptoms
include nausea, vomiting, di-arrhea, abdominal discomfort, and abdominal
distention. Uro-logic symptoms can mimic such disorders as appendicitis, peptic
ulcer disease, or cholecystitis, thus making diagnosis difficult, es-pecially
in the elderly, because of decreased neurologic innerva-tion to this area
(Kuebler, 2001; Wade-Elliot, 1999).
PHYSICAL EXAMINATION
Several
body systems can affect upper and lower urinary tract dys-function, and that
dysfunction can affect several end organs; therefore, a head-to-toe assessment
is indicated. Areas of empha-sis include the abdomen, suprapubic region,
genitalia and lower back, and lower extremities.
Direct
palpation of the kidneys may help determine their size and mobility. The
correct position for palpation is presented in Figure 43-5. It may be possible
to feel the smooth, rounded lower pole of the kidney between the hands,
although the right kidney is easier to feel because it is somewhat lower than
the left one. In obese patients, palpation of the kidneys is generally more
difficult.

Renal
dysfunction may produce tenderness over the costover-tebral angle, which is the
angle formed by the lower border of the 12th, or bottom, rib and the spine. The
abdomen (just slightly to the right and left of midline in both upper
quadrants) is auscul-tated to assess for bruits (low-pitched murmurs that
indicate renal artery stenosis or an aortic aneurysm). The abdomen is also
as-sessed for the presence of peritoneal fluid, which may occur with kidney
dysfunction.
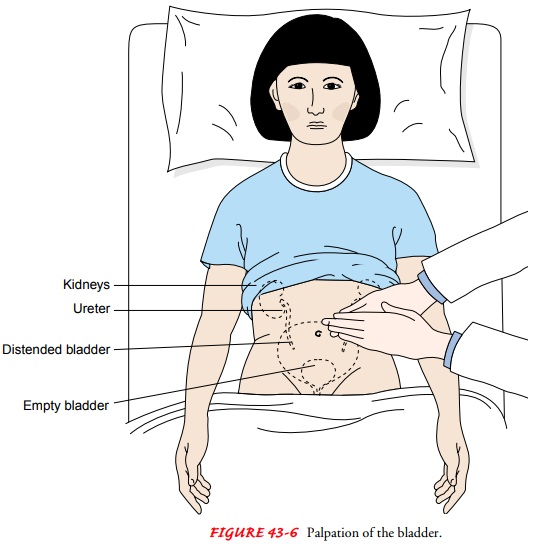
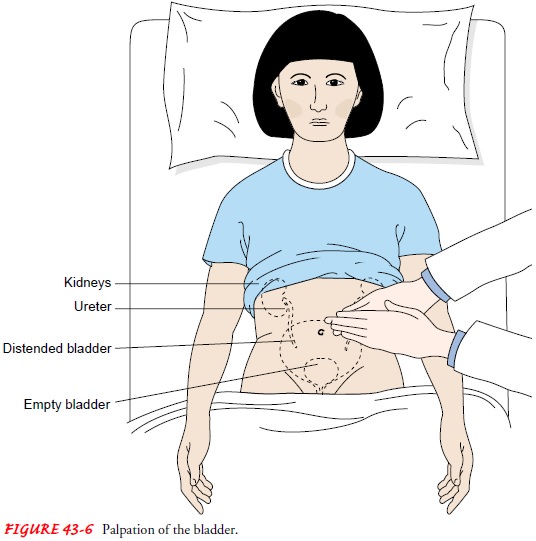
The
bladder should be percussed after the patient voids to check for residual
urine. Percussion of the bladder begins at the midline just above the umbilicus
and proceeds downward. The sound changes from tympanic to dull when percussing
over the bladder. The bladder, which can be palpated only if it is moderately
dis-tended, feels like a smooth, firm, round mass rising out of the ab-domen,
usually at midline (Fig. 43-6). Dullness to percussion of the bladder following
voiding indicates incomplete bladder emptying.
In
older men, benign prostatic hyperplasia (BPH) is a common cause of urinary
dysfunction. Because the signs and symptoms of prostate cancer can mimic those
of BPH, the prostate gland is pal-pated by digital rectal examination (DRE) as
part of the yearly physical examination in men ages 50 and older (45 if there
is a family history of prostate cancer). In addition, a blood specimen is
obtained to test the prostate specific antigen (PSA) level annu-ally; the
results of the DRE and PSA are then correlated. Blood is drawn for PSA before
the DRE because manipulation of the prostate can cause the PSA level to rise
temporarily. The inguinal area is examined for enlarged nodes, an inguinal or
femoral her-nia, or varicocele (varicose veins of the spermatic cord) (American
Foundation for Urological Disease, 2000; Degler, 2001).
In
women, the vulva, urethral meatus, and vagina are exam-ined. The urethra is
palpated for diverticula and the vagina is assessed for adequate estrogen effect
and any of five types of her-niation (Goolsby, 2001). Urethrocele is the
bulging of the ante-rior vaginal wall into the urethra. Cystocele is the
herniation of the bladder wall into the vaginal vault. The cervix bulging into
the vaginal vault is referred to as pelvic prolapse. Enterocele is her-niation
of the bowel into the posterior vaginal wall, and rectocele is the herniation
of the rectum into the vaginal wall. These pro-lapses are graded depending on
the degree of herniation.
The
woman is asked to cough and perform a Valsalva maneu-ver to assess the
urethra’s system of muscular and ligament sup-port. If urine leakage occurs,
the index and middle fingers of the examiner’s gloved hand are used to support
either side of the urethra as the woman is asked to repeat these maneuvers.
This is called the Marshall-Boney maneuver.
If no
urine leakage is detected when external support is pro-vided to the urethra,
poor pelvic floor support—referred to as urethral hypermobility—is identified
as the suspected cause of the urinary incontinence. Stress urinary incontinence
(SUI) is graded based on its severity. Grade 1 and Grade 2 SUI relate to the
degree of urethral hypermobility. Grade 3, the most severe form of SUI, refers
to the inability of the urethral walls to remain compressed with abdominal
pressure such as a cough or Valsalva maneuver. Grade 3 is referred to as
intrinsic sphincter deficiency (ISD) (Albaugh, 1999).
If
some residual leakage of urine is noted despite support, ISD is suspected.
Urethral hypermobility may be suspected when Q-tip test results are positive.
The Q-tip test involves gently placing a well-lubricated Q-tip into the urethra
until resistance is no longer noted, then gently pulling back on the Q-tip
until resistance is felt. The female patient is asked to cough and perform the
Val-salva maneuver. If there is an upward (positive deflection) of the visible
part of the Q-tip, urethral hypermobility is at least one of the causes for the
type of incontinence referred to as stress in-continence.
The patient is assessed for edema and changes in body weight. Edema may be observed, particularly in the face and dependent parts of the body, such as the ankles and sacral areas, and suggests fluid retention. An increase in body weight commonly accompa-nies edema. A 1-kg weight gain equals approximately 1,000 mL of fluid.
The
deep tendon reflexes of the knee are assessed for quality and symmetry. This is
an important part of testing for neurolog-ical causes of bladder dysfunction
because the sacral area, which innervates the lower extremities, is the same
peripheral nerve area responsible for urinary continence. The gait pattern of
the indi-vidual with bladder dysfunction is also noted, as well as the
pa-tient’s ability to walk toe-to-heel. These tests evaluate possible
supraspinal causes for urinary incontinence (Appell, 1999).
Gerontologic Considerations
Upper and lower urinary tract function
changes with age. The GFR decreases with age starting between ages 35 and 40. A
yearly decline of about 1 mL/min continues thereafter. Tubular function,
in-cluding reabsorption and concentrating ability, is also reduced with
increasing age. Although renal function usually remains adequate despite these
changes, renal reserve is decreased and may reduce the kidneys’ ability to
respond effectively to drastic or sudden physio-logic changes. This steady
decrease in glomerular filtration, com-bined with the use of multiple
medications whose metabolites clear the body via the kidneys, puts the older
individual at higher risk for adverse drug effects and drug-to-drug
interactions (Schafer, 2001).
Structural
or functional abnormalities that occur with aging may prevent complete emptying
of the bladder. This may be dueto decreased bladder wall contractility, due to
myogenic or neu-rogenic causes, or structurally, related to bladder outlet
obstruc-tion, as in BPH. Vaginal and urethral tissues atrophy (become thinner)
in aging women due to decreased estrogen levels. This causes decreased blood supply
to the urogenital tissues, causing urethral and vaginal irritation and urinary
incontinence.
Urinary
incontinence is the most common reason for admis-sion to skilled nursing
facilities. Many older individuals and their families are unaware that urinary
incontinence stems from many causes. The nurse needs to inform the patient and
family that with appropriate evaluation, urinary incontinence can often be
managed at home and in many cases can be eliminated (Degler, 2000). Many
treatments are available for urinary incontinence in the elderly, including
noninvasive, behavioral interventions that the individual or the caregiver can
carry out (Kincade, Peckous Busby-Whitehead, 2001).
Preparation
of the elderly patient for diagnostic tests must be managed carefully to
prevent dehydration, which might precipi-tate renal failure in a patient with
marginal renal reserve. Limita-tions in mobility may affect an elderly
patient’s ability to void adequately or to consume an adequate volume of
fluids. The pa-tient may limit fluid intake to minimize the frequency of
voiding or the risk of incontinence. Teaching the patient and family about the
dangers of an inadequate fluid intake is an important role of the nurse caring
for the elderly patient.
Related Topics