Chapter: Medical Surgical Nursing: Management of Patients With Coronary Vascular Disorders
Coronary Atherosclerosis - Coronary Artery Disease
Coronary Artery Disease
Coronary
artery disease (CAD) is the most prevalent type of cardio-vascular disease. For
this reason, it is important for nurses to be-come familiar with the various
types of coronary artery conditions and the methods for assessing, preventing,
and treating these dis-orders medically and surgically.
CORONARY ATHEROSCLEROSIS
The
most common heart disease in the United States is athero-sclerosis, which is an abnormal accumulation of lipid, or
fatty,substances and fibrous tissue in the vessel wall. These substances create
blockages or narrow the vessel in a way that reduces blood flow to the
myocardium. Studies (Mehta et al., 1998) indicate that atherosclerosis involves
a repetitious inflammatory response to artery wall injury and an alteration in
the biophysical and bio-chemical properties of the arterial walls. An
association between an infection (eg, gingivitis) and the later development of
heart disease is being explored, as is the administration of antibiotics to
prevent heart disease. Although authorities disagree about how atherosclerosis
begins, they agree that atherosclerosis is a pro-gressive disease that can be
curtailed and, in some cases, reversed.
Pathophysiology
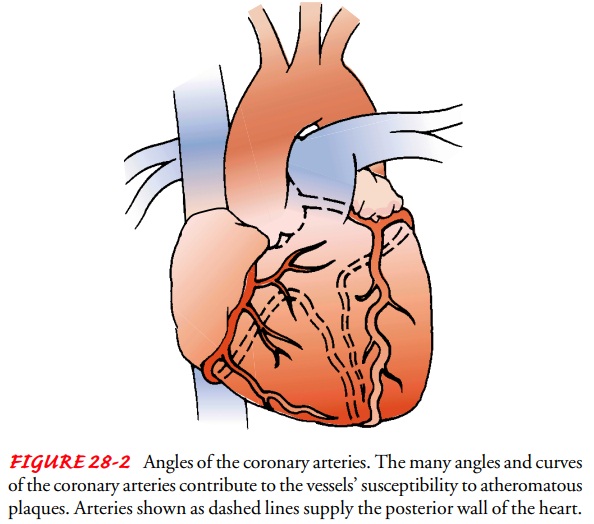
Atherosclerosis
begins as fatty streaks, lipids that are deposited in the intima of the
arterial wall. Although they are thought to be the precursors of
atherosclerosis, fatty streaks are common, even in childhood. Moreover, not all
develop into more advanced le-sions. The reason why some fatty streaks continue
to develop is unknown, although genetic and environmental factors are
in-volved. The continued development of atherosclerosis involves an
inflammatory response. T lymphocytes and monocytes (that become macrophages)
infiltrate the area to ingest the lipids and then die; this causes smooth
muscle cells within the vessel to pro-liferate and form a fibrous cap over the
dead fatty core. These de-posits, called atheromas
or plaques, protrude into the lumen of the vessel, narrowing it and obstructing
blood flow (Fig. 28-1). If the fibrous cap of the plaque is thick and the lipid
pool remains relatively stable, it can resist the stress from blood flow and
vessel movement. If the cap is thin, the lipid core may grow, causing it to
rupture and hemorrhage into the plaque, allowing a thrombus to develop. The
thrombus may obstruct blood flow, leading to sudden cardiac death or an acute myocardial infarction (MI), which is
the death of heart tissue.
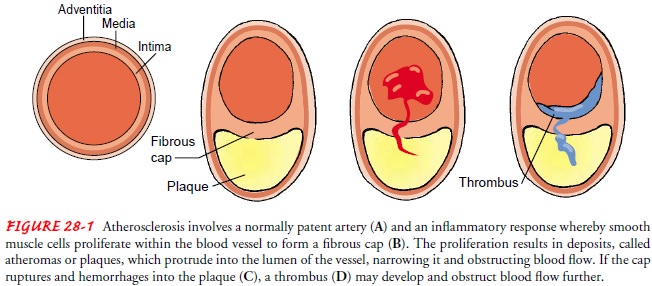
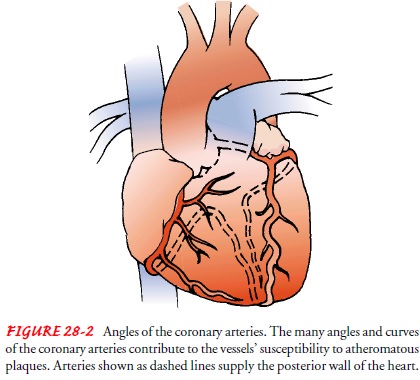
The anatomic structure of the coronary arteries makes them particularly susceptible to the mechanisms of atherosclerosis. As Figure 28-2 shows, they twist and turn as they supply blood to the heart, creating sites susceptible to atheroma development. Although heart disease is most often caused by atherosclerosis of the coronary arteries, other phenomena decrease blood flow to the heart. Examples include vasospasm (sudden constriction or nar-rowing) of a coronary artery, myocardial trauma from internal or external forces, structural disease, congenital anomalies, de-creased oxygen supply (eg, from acute blood loss, anemia, or low blood pressure), and increased demand for oxygen (eg, from rapid heart rate, thyrotoxicosis, or ingestion of cocaine).
Clinical Manifestations
Coronary atherosclerosis produces symptoms and complications according to the location and degree of narrowing of the arterial lumen, thrombus formation, and obstruction of blood flow to the myocardium. This impediment to blood flow is usually progres-sive, causing an inadequate blood supply that deprives the muscle cells of oxygen needed for their survival. The condition is known as ischemia. Angina pectoris refers to chest pain that is brought about by myocardial ischemia. Angina pectoris usually is caused by significant coronary atherosclerosis. If the decrease in blood supply is great enough, of long enough duration, or both, irre-versible damage and death of myocardial cells, or MI, may result. Over time, irreversibly damaged myocardium undergoes degeneration and is replaced by scar tissue, causing various degrees of myo-cardial dysfunction.
Significant myocardial damage may cause inadequate cardiac output,
and the heart cannot support the body’s needs for blood, which is called heart
failure (HF). A de-crease in blood supply from CAD may even cause the heart to
stop abruptly, an event that is called sudden
cardiac death.
The
most common manifestation of myocardial ischemia is acute onset of chest pain.
However, an epidemiologic study of the people in Framingham, Massachusetts,
showed that nearly 15% of men and women who had MIs were totally asymptomatic
(Kannel, 1986). Another study found that 33% of those diag-nosed with MI did
not present to the emergency room with chest pain (Canto et al., 2000; Ishihara
et al., 2000). Those without chest pain tend to be older or women, or to have
diabetes or a his-tory of heart failure. Women have been found to have more
atyp-ical symptoms of myocardial ischemia (eg, shortness of breath, nausea,
unusual fatigue) than men (Meischke et al., 1999). The incidence of prodromal
angina (ie, angina a few hours to days be-fore the MI) was found to be
significantly lower in patients older than 70 years of age (Ishihara et al.,
2000). Other clinical mani-festations of CAD may be abnormalities signaled by
changes on the electrocardiogram (ECG), high levels of cardiac enzymes,
dysrhythmias, and sudden death.
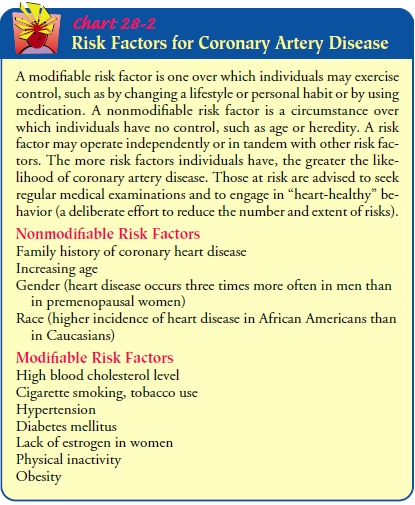
Risk Factors
Epidemiologic
studies point to several factors that increase the probability that heart
disease will develop. Major risk factors in-clude use of tobacco, hypertension,
elevated blood lipid levels, fam-ily history of premature cardiovascular
disease (first-degree relative with cardiovascular disease at age 55 or younger
for men and at age 65 or younger for women) and age (>45 years for men;
>55 years for women). The Third Report of the Expert Panel on Detection,
Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment
Panel III [ATP III]; 2001) represents the up-dated clinical guidelines for
cholesterol testing and management. ATP III addresses primary prevention (preventing the occurrence of CAD) and secondary prevention (preventing the progression
of CAD).
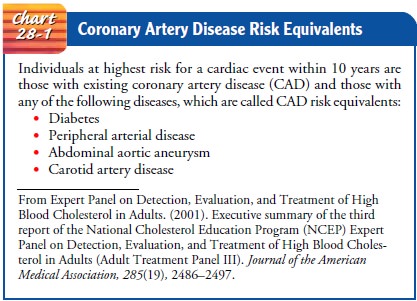
ATP
III is the standard for cholesterol management. ATP III continues to identify
elevated low-density lipoprotein (LDL) cholesterol
as the primary target of cholesterol-lowering therapy. Those at highest risk
for having a cardiac event within 10 years are those with existing CAD or those
with diabetes, peripheral ar-terial disease, abdominal aortic aneurysm, or
carotid artery dis-ease. The latter diseases are called CAD risk equivalents,
because patients with these diseases have the same risk for a cardiac event as
patients with CAD (Chart 28-1). The possibility of having a cardiac event
within 10 years is also determined by points given to several factors, such as
age, level of total cholesterol, level of LDL, level of high-density lipoprotein (HDL), systolic blood pressure, and
tobacco use. If the total points add up to more than 15 for men or 23 for
women, the person has a greater than 20% risk for a cardiac event within 10
years. A composite of lipid and nonlipid risk factors of metabolic origin,
called metabolic syn-drome, is
another risk factor for CAD. Metabolic syndrome in-cludes abdominal obesity, an
elevated triglyceride level, low HDL level, elevated blood pressure, and
impaired function of insulin.
Measurement
of other emerging risk factors, such as elevations of Lipoprotein(a) [Lp(a)],
remnant lipoproteins, small LDL, fibrinogen, homocysteine, and impaired fasting
plasma glucose (110–125 mg/dL), is optional and are not routinely recom-mended
(ATP III, 2001). For example, the Homocysteine Studies Collaboration (2002)
found that lower levels of homocysteine, an amino acid, were modestly
associated with reduced risk of ischemic heart disease and stroke. The results
of these retrospective studies suggest that homocysteine may promote
atherosclerosis. A meta-analysis of prospective studies was done that showed a
sig-nificant association between homocysteine levels and ischemic heart disease
as well as between homocysteine and stroke (Wald, Law, & Morris, 2002). The
authors recommend a daily intake of approximately 0.8 mg of folic acid to
decrease blood homocys-teine levels and reduce the risk of ischemic heart
disease and CVA (brain attack, stroke). The American Heart Association has
stated that until the results of large-scale randomized trials become
avail-able, routine testing of homocysteine concentrations cannot be justified
(Malinow, Bostom, & Krauss, 1999).
Prevention
Four
modifiable risk factors—cholesterol abnormalities, cigarette smoking (tobacco
use), hypertension, and diabetes mellitus— have been cited as major risk
factors for CAD and its consequent complications. As a result, they receive
much attention in health promotion programs (Chart 28-2).
CONTROLLING CHOLESTEROL ABNORMALITIES
The
association of a high blood cholesterol level with heart dis-ease is well
established and accepted. The metabolism of fats is important in understanding
the development of heart disease.
Fats,
which are insoluble in water, are encased in water-soluble lipoproteins to
allow them to be transported within a circulatory system that is water-based.
Four elements of fat metabolism—total cholesterol, LDL, HDL, and
triglycerides—are primary factors affecting the development of heart disease (Fig.
28-3). Cholesterol and the lipoproteins are synthesized by the liver or
ingested as part of the diet. All adults 20 years of age or older should have a
fasting lipid profile (total cholesterol, LDL, HDL, and triglyceride)
per-formed at least once every 5 years and more often if the profile is
abnormal. Patients who have had an acute event (MI), percuta-neous coronary
intervention (PCI), or coronary artery
bypassgraft (CABG) require assessment of the LDL-cholesterol levelwithin 60
to 365 days after the event (LDL levels may be low im-mediately after the acute
event). Subsequently, lipids should be monitored every 6 weeks until the
desired level is achieved and then every 4 to 6 months (Expert Panel on
Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults,
2001).
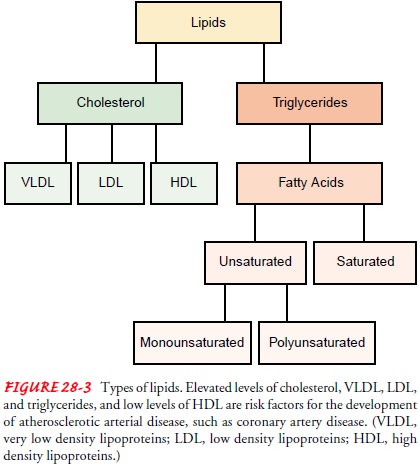
LDL
exerts a harmful effect on the arterial wall and accelerates atherosclerosis.
In contrast, HDL promotes the use of total cho-lesterol by transporting LDL to
the liver, where it is biodegraded and then excreted. The desired goal is to
have low LDL values and high HDL values. The desired level of LDL depends on
the patient:
·
Less than 160 mg/dL for patients
with one or no risk factors
·
Less than 130 mg/dL for patients
with two or more risk factors
· Less than 100 mg/dL for patients with CAD or a CAD risk equivalent
Serum
cholesterol and LDL levels can usually be controlled by diet and physical
activity. Depending on the patient’s LDL level and risk of coronary heart
disease, medication therapy may also be prescribed.
The
level of HDL should exceed 40 mg/dL and should ideally be more than 60 mg/dL. A
high HDL level is a strong negative risk factor (is protective) for heart
disease.
Triglyceride
is another fatty substance, made up of fatty acids, that is transported through
the blood by a lipoprotein. Although an elevated triglyceride level (>200
mg/dL) may be ge-netic in origin, it also can be caused by obesity, physical
inactivity, excessive alcohol intake, high-carbohydrate diets, diabetes
mellitus, kidney disease, and certain medications, such as birth control pills,
corticosteroids, and beta-adrenergic blockers when given in higher doses.
Management of elevated triglyceride focuses on weight reduction and increased
physical activity. Med-ications such as nicotinic acid and fibric acids (eg,
fenofibrate [Tricor], clofibrate [Atromid-S]) may also be prescribed,
espe-cially if the triglyceride level is above 500 mg/dL (Expert Panel on
Detection, Evaluation, and Treatment of High Blood Cho-lesterol in Adults,
2001).
Lipoprotein(a),
or Lp(a), is a component of LDL and is at-tached to a special protein called
apo(a). The level of Lp(a) is pri-marily determined by genetics. An elevated
level of Lp(a) has been associated with a higher risk of CAD. However, clinical
tri-als have not yet identified methods that lower the level of Lp(a) and have
not demonstrated that lower levels of Lp(a) reduce the risk of CAD; therefore
Lp(a) is not routinely monitored (Danesh, et al., 2000; Gibbons et al., 1999).
Dietary Measures.
Table 28-1 provides recommendations of theTherapeutic Lifestyle
Changes (TLC) diet (Expert Panel on De-tection, Evaluation, and Treatment of
High Blood Cholesterol in Adults, 2001). However, these recommendations may
need to be adjusted to match the individual patient who has other nutri-tional
needs, such as the requirements for pregnancy or diabetes. To assist in
following the appropriate TLC diet, the patient should be referred to a
registered dietitian. Other TLC recom-mendations are weight loss, cessation of
tobacco use, and in-creased physical activity.
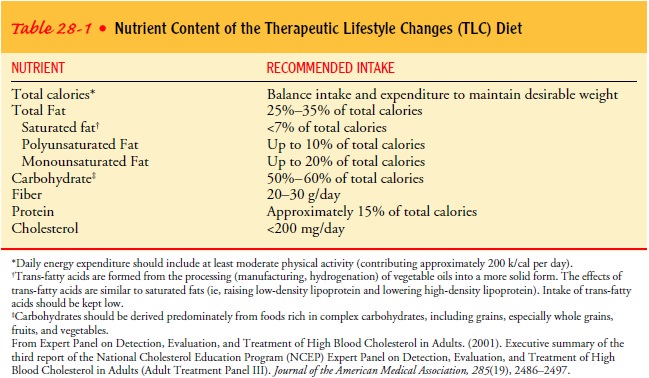
Soluble
dietary fiber may also help lower cholesterol levels. Soluble fibers, which are
found in fresh fruit, cereal grains, veg-etables, and legumes, enhance the
excretion of metabolized cho-lesterol. The ability of fiber to reduce serum
cholesterol continues to be investigated. Intake of at least 20 to 30 grams of
fiber each day is recommended (Expert Panel on Detection, Evaluation, and
Treatment of High Blood Cholesterol in Adults, 2001).
Many resources are available to assist people who are attempt-ing to control their cholesterol levels. The National Heart, Lung, and Blood Institute (NHLBI) and its National Cholesterol Edu-cation Program (NCEP), the American Heart Association, and the American Diabetic Association, as well as CAD support groups and reliable Internet sources, are a few examples of the available re-sources.
Cookbooks and recipes
that include the nutritional break-down of foods can be included as resources
for patients. Dietary control has been made easier because food manufacturers
are re-quired to provide comprehensive nutritional data on product la-bels. The
label information of interest to a person attempting to eat a heart-healthy
diet is as follows:
·
Serving size, expressed in household
measures
·
Amount of total fat per serving
·
Amount of saturated fat per serving
·
Amount of cholesterol per serving
·
Amount of fiber per serving
Physical Activity.
Regular, moderate physical activity increasesHDL levels and
reduces triglyceride levels. The goal for the aver-age person is a total of 30
minutes of exercise, three to four times per week. The nurse helps patients set
realistic goals for physical activity. For example, the inactive patient should
start with activ-ity that lasts 3 minutes, such as parking farther from a
building to increase the walking time. For sustained activity, patients should
begin with a 5-minute warm-up period to stretch and prepare the body for the
exercise. They should end the exercise with a 5-minute cool-down period in
which they gradually reduce the intensity of the activity to prevent a sudden
decrease in cardiac output. Pa-tients should be instructed to engage in an
activity or variety of activities that interest them, to maintain motivation.
They should also be taught to exercise to an intensity that does not preclude
their ability to talk; if they cannot have a conversation, they should slow
down or switch to a less intensive activity. When the weather is hot and humid,
the patient should be advised to exercise dur-ing the early morning or indoors
and wear loose-fitting clothing. When the weather is cold, the patient should
be instructed to layer clothing and to wear a hat. The nurse can also advise
the pa-tient to avoid adverse weather conditions by participating in local
community programs, such as those held at shopping malls. The nurse should
inform patients to stop any activity if they develop chest pain, unusual
shortness of breath, dizziness, lightheadedness, or nausea.
Medications.
Medications (Table 28-2) are used in some instancesto control
cholesterol levels. If diet alone cannot normalize serum cholesterol levels,
several medications have a synergistic effect with the prescribed diet.
Lipid-lowering medications can reduce CAD mortality in patients with elevated
lipid levels and in those with normal lipid levels. The lipid-lowering agents
affect the different lipid components and are usually grouped into four types:
·
3-Hydroxy-3-methylglutaryl coenzyme
A (HMG-CoA) re-ductase inhibitors or statins (eg, lovastatin [Mevacor],
prava-statin [Pravachol], simvastatin [Zocor]; see Table 28-2) block
cholesterol synthesis, lower LDL and triglyceride levels, and increase HDL
levels. These medications are frequently the initial medication therapy for
significantly elevated choles-terol and LDL levels. Because of their effect on
the liver, results of hepatic function tests are monitored.
·
Nicotinic acids (niacin [Niacor,
Niaspan]; see Table 28-2) decrease lipoprotein synthesis, lower LDL and
triglyceride levels, and increase HDL levels. The dose of niacin needs to be
titrated weekly to achieve therapeutic dosage. Niacin is the medication most
often used for minimally elevated cho-lesterol and LDL levels or as an adjunct
to a statin when the lipid goal has not been achieved and the triglycerides are
elevated. Side effects include gastrointestinal upset, gout, and flushing.
Because of its effect on the liver, hepatic function is monitored.
·
Fibric acid or fibrates (eg,
clofibrate [Atromid-S], fenofibrate [Ticor]; see Table 28-2) decrease the
synthesis of cholesterol, reduce triglyceride levels, and increase HDL levels.
Because they have the potential to increase LDLs, fibrates are the medications
of choice for patients with triglyceride levels above 400 mg/dL. Because of the
risk of myopathy and acute renal failure, fibrates should be used with caution
in patients who are also taking a statin.
·
Bile acid sequestrants or resins
(eg, cholestyramine [LoCholest, Questran, Prevalite]; see Table 28-2) bind
cho-lesterol in the intestine, increase its breakdown, and lower LDL levels
with minimal effect on HDLs and no effect (or minimal increase) on triglyceride
levels. These medications are more often used as adjunct therapy when statins
alone have not been effective in controlling lipid levels and the triglyceride
levels are less than 200 mg/dL. Significant side effects, such as gastric
distention and constipation, can occur from using these medications.
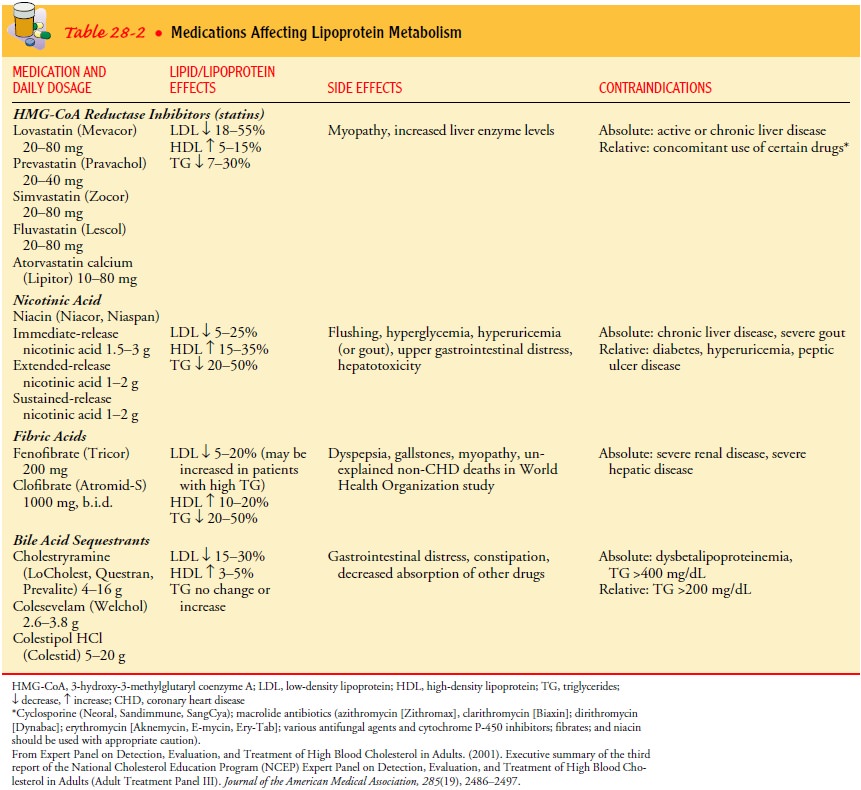
Medication
therapy is reserved for at-risk patients and is not regarded as a substitute
for dietary modification. All of these med-ications have been shown to reduce
major coronary events (Ex-pert Panel on Detection, Evaluation, and Treatment of
High Blood Cholesterol in Adults, 2001). Some of these may be used in
combination to achieve synergistic effects. For example, LDL cholesterol can be
lowered more effectively by adding a low dose of resin to a dose of niacin or
statins, or both, than a maximum dose of an individual agent.
Patients
with elevated cholesterol levels should be monitored for adherence to the
medical plan, the effect of cholesterol-lowering medications, and the
development of side effects from cholesterol-lowering medications. Lipid levels
are obtained and adjustments made to the diet and medication every 6 weeks
until the lipid goal or maximum dose is achieved and then every 6 months
thereafter.
PROMOTING CESSATION OF TOBACCO USE
Cigarette
smoking contributes to the development and severity of CAD in three ways.
First, the inhalation of smoke increases the blood carbon monoxide level,
causing hemoglobin, the oxygen-carrying component of blood, to combine more
readily with car-bon monoxide than with oxygen. A decreased amount of available
oxygen may decrease the heart’s ability to pump.
Second,
the nicotinic acid in tobacco triggers the release of cat-echolamines, which
raise the heart rate and blood pressure. Nico-tinic acid can also cause the
coronary arteries to constrict. Smokers have a tenfold increase in risk for
sudden cardiac death. The in-crease in catecholamines may be a factor in the
increased incidence of sudden cardiac death.
Third,
use of tobacco causes a detrimental vascular response and increases platelet
adhesion, leading to a higher probability of thrombus formation. A person with
increased risk for heart dis-ease is encouraged to stop tobacco use through any
means possi-ble: counseling, consistent motivation and reinforcement messages,
support groups, and medications. Some people have found com-plementary therapies
(eg, acupuncture, guided imagery, hypnosis) to be helpful. People who stop
smoking reduce their risk of heart disease by 30% to 50% within the first year,
and the risk contin-ues to decline as long as they refrain from smoking.
Exposure to other smokers’ smoke (passive or second-hand smoke) is believed to cause heart disease in nonsmokers. Oral contraceptive use by women who smoke is inadvisable because these medications significantly increase the risk of CAD and sud-den cardiac death.
Cessation
of tobacco use results in a lower rate of cardiac events. Patients should be
advised to participate in an educa-tional class, support group, or behavioral
program. Use of med-ications such as the nicotine patch (Nicotrol, Nicoderm CQ,
Habitrol) or bupropion (Zyban) may assist with stopping use of tobacco, but do
have the same systemic effects: catecholamine release (increasing heart rate
and blood pressure) and increased platelet adhesion. These medications should
be used for the shortest time and at the lowest effective doses.
MANAGING HYPERTENSION
Hypertension
is defined as blood pressure measurements that re-peatedly exceed 140/90 mm Hg.
Long-standing elevated blood pressure may result in increased stiffness of the
vessel walls, lead-ing to vessel injury and a resulting inflammatory response
within the intima. Hypertension can also increase the work of the left
ventricle, which must pump harder to eject blood into the arter-ies. Over time,
the increased workload causes the heart to enlarge and thicken (ie,
hypertrophy), a condition that may eventually lead to cardiac failure.
Early
detection of high blood pressure and adherence to a therapeutic regimen can
prevent the serious consequences associ-ated with untreated elevated blood
pressure.
CONTROLLING DIABETES MELLITUS
The
relationship between diabetes mellitus and heart disease has been
substantiated. For 65% to 75% of patients with diabetes, car-diovascular
disease is listed as the cause of death (Braunwald et al., 2001; Grundy et al.,
1999). Hyperglycemia fosters dyslipidemia, increased platelet aggregation, and
altered red blood cell function, which can lead to thrombus formation. It has
been suggested that
these
metabolic alterations impair endothelial cell–dependent vasodilation and smooth
muscle function; treatment with insulin (eg, Humalog, Humulin, Novolin) and
metformin (Glucophage) has demonstrated improvement in endothelial function:
im-proved endothelial-dependent dilation (Gaenzer et al., 2002). Diabetes is
considered equivalent to existing CAD in its risk of a cardiac event within 10
years (Expert Panel on Detection, Evaluation, and Treatment of High Blood
Cholesterol in Adults, 2001).
Gender and Estrogen Level
Because
heart disease had been considered to primarily affect white men, the disease
was not as readily recognized and treated in women. However, in 1999 in the
United States, 512,904 women died because of cardiovascular disease whereas
42,144 women died from breast cancer and 246,006 women died from any form of
cancer (American Heart Association, 2002). Women tend to have a higher
incidence of complications from CAD (American Heart Association, 2002).
African-American women have a mortality rate nearly twice that of Caucasian
women (Office for Social Environment and Health Research at West Virginia
Uni-versity, 2001). Women tend not to recognize the symptoms as early as men
and to wait longer to report their symptoms and seek medical assistance
(Meischke et al., 1999; Penque et al., 1998). In the past, women were less
likely than men to be referred for coronary artery diagnostic procedures, to
receive medical therapy (eg, thrombolytic
therapy to break down the blood clots that cause acute MI, or nitroglycerin),
and to be treated with invasive interventions, eg, angioplasty (Sheifer et al.,
2000). It is antici-pated that with better education of the general public and
health care professionals, gender and racial differences will have less
in-fluence on the diagnosis, treatment, and incidence of complica-tions of
heart disease in the future.
In
women younger than age 55, the incidence of CAD is sig-nificantly lower than in
men. However, after age 55, the inci-dence in women is approximately equal to
that in men. The age difference of the incidence of CAD in women may be related
to estrogen. Although hormone
replacement therapy (HRT) for menopausal women had been promoted as
prevention for CAD, research studies do not support HRT as an effective means
of CAD prevention (Hulley et al., 1998; Mosca, 2000). HRT has de-creased
postmenopausal symptoms and the risk for osteoporosis-related bone fractures,
but HRT also has been associated with an increased risk for CAD, breast cancer,
deep vein thrombosis, cerebrovascular accident (CVA, brain attack, stroke), and
pul-monary embolism. The Women’s Health Initiative (Gebbie, 2002) demonstrated
that long-term HRT may have more risks than benefits, and that HRT should not
be initiated or continued for primary prevention of CAD.
Behavior Patterns
Most
clinicians believe that stress and certain behaviors contribute to the
pathogenesis of CAD and a cardiac event, especially in women. Psychological and
epidemiologic studies describe behav-iors that characterize people who are
prone to heart disease: exces-sive competitiveness, a sense of time urgency or
impatience, aggressiveness, and hostility (Dembroski et al., 1989; Friedman
Rosenman, 1959; Krantz et al., 2000). A person with these behaviors is
classified as type A coronary-prone.
The
type A coronary-prone classification may not be as sig-nificant as was once
thought; evidence of its precise role remains inconclusive (Rozanski et al.,
1999). To be on the safer side, how-ever, such a person may be wise to alter
behaviors and responses to triggering events and to reduce other risk factors.
Nurses can assist these people by teaching them cognitive restructuring and
relaxation techniques. Because people who are depressed have worse outcomes,
these patients should be assessed for signs and symptoms of depression and, if
diagnosed, appropriately treated.
Related Topics