Chapter: Medical Surgical Nursing: Management of Patients With Coronary Vascular Disorders
Nursing Process: The Patient Awaiting Cardiac Surgery
NURSING PROCESS: THE PATIENT AWAITING CARDIAC SURGERY
The
cardiac surgery patient has many of the same needs and requires the same
perioperative care as other surgical patients. The patient and family are
experiencing a major life crisis. The association of the heart with life and
death intensifies their emotional and psychological needs. Patients frequently
are ad-mitted the same day as the procedure. For these patients, the nurse must
prioritize needs carefully; in the time allowed, the nurse focuses on the needs
that have the highest priority.
Before
surgery, physical and psychological assessments establish the baselines for
future reference. The patient’s understanding of the surgical procedure,
informed consent, and adherence to treatment protocols are evaluated. Helping
the patient to cope, understand the procedure, and maintain dignity are nursing
responsibilities.
The
preoperative phase of cardiac surgery begins before hos-pitalization. The nurse
assesses the patient for other disorders, such as diabetes, hypertension, and
respiratory, gastrointestinal, and hematologic diseases, and documents their
treatment.
The
nurse clarifies how the medication regimen is to be al-tered before surgery,
such as tapering corticosteroids and digoxin, decreasing or discontinuing
anticoagulants, and maintaining med-ications for treatment of blood pressure,
angina, diabetes, and dysrhythmias. The nurse also clarifies the need to
maintain activ-ity patterns, a healthy diet, healthful sleep habits, and
cessation of smoking to minimize the risks of surgery.
Assessment
Patients
with nonacute heart disease may be admitted to the hos-pital the day of or the
day before the surgery. Most of the pre-operative evaluation is completed
before the patient enters the hospital. Many surgeons’ offices or hospitals
mail an informa-tion packet to the patient’s home.
A history and physical examination are performed by nursing and medical personnel. A chest x-ray, ECG, laboratory tests, blood typing and crossmatching, and autologous blood donation (pa-tient’s own blood) may also be performed. The health assessment focuses on obtaining baseline physiologic, psychological, and social information. The patient’s and family’s learning needs are identi-fied and addressed as necessary. Of particular importance are the patient’s usual functional level, coping mechanisms, and support systems. These are important because the support of the family or significant others will affect the patient’s postoperative course and rehabilitation. Discharge plans are influenced by the lifestyle de-mands of the home situation and the physical environment of the home.
HEALTH HISTORY
The
preoperative history and health assessment should be thor-ough and well
documented because they provide a basis for post-operative comparison. A
systematic assessment of all systems is performed, with emphasis on cardiovascular
functioning.
Functional
status of the cardiovascular system is determined by reviewing the patient’s
symptoms, including past and pres-ent experiences with chest pain,
hypertension, palpitations, cyanosis, breathing difficulty (dyspnea), leg pain
that occurs with walking (intermittent claudication), orthopnea, paroxys-mal
nocturnal dyspnea, and peripheral edema. Because alterations in cardiac output
can affect renal, respiratory, gastrointestinal, in-tegumentary, hematologic,
and neurologic functioning, a history ofthese systems is also reviewed. The
patient’s history of major ill-nesses, previous surgeries, medication
therapies, and use of drugs, alcohol, and tobacco is also obtained.
PHYSICAL ASSESSMENT
A
complete physical examination is performed, with special em-phasis on the
following:
·
General appearance and behavior
·
Vital signs
·
Nutritional and fluid status,
weight, and height
·
Inspection and palpation of the
heart, noting the point of maximal impulse, abnormal pulsations, and thrills
·
Auscultation of the heart, noting
pulse rate, rhythm, and qual-ity; S3
and S4, snaps, clicks, murmurs, and
friction rub
·
Jugular venous pressure
·
Peripheral pulses
·
Peripheral edema
PSYCHOSOCIAL ASSESSMENT
The
psychosocial assessment and the assessment of the patient’s and family’s
learning needs are as important as the physical exam-ination. Anticipation of
cardiac surgery is a source of great stress to the patient and family. They
will be anxious and fearful and often have many unanswered questions. Their anxiety
usually increases with the patient’s admission to the hospital and the
immediacy of surgery. An assessment of the level of anxiety is important. If it
is low, it may indicate denial. If it is extremely high, it may in-terfere with
the use of effective coping mechanisms and with pre-operative teaching.
Questions may be asked to obtain the following information:
·
Meaning of the surgery to the
patient and family
·
Coping mechanisms that are being
used
·
Measures used in the past to deal
with stress
·
Anticipated changes in lifestyle
·
Support systems in effect
·
Fears regarding the present and the
future
·
Knowledge and understanding of the
surgical procedure, postoperative course, and long-term rehabilitation
The
nurse allows adequate time for the patient and family to express their fears.
The fears most often expressed are fear of the unknown, fear of pain, fear of
body image change, and fear of dying. During the assessment, the nurse
determines how much the patient and family know about the impending surgery and
the expected postoperative events. They are encouraged to ask questions and to
indicate how much information they wish to re-ceive. Some patients prefer not
to have detailed information, whereas others want to know as much as possible.
Patients are ap-proached as unique individuals with their own specific learning
needs, learning styles, and levels of understanding.
Patients
requiring emergency heart surgery may have cardiac catheterization and surgery
within several hours of admission. The nurse will have little opportunity to
assess and meet their emotional and learning needs before surgery. As a result,
patients will need extra help after surgery to adjust to the situation.
Diagnosis
NURSING DIAGNOSES
The
nursing diagnoses for patients awaiting cardiac surgery vary according to each
patient’s cardiac disease and symptoms. Most patients have a nursing diagnosis
of decreased cardiac output. Preoperative nursing diagnoses for most patients
may include:
·
Fear related to the surgical
procedure, its uncertain outcome, and the threat to well-being
·
Deficient knowledge regarding the
surgical procedure and the postoperative course
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
The
stress of impending cardiac surgery may precipitate compli-cations that require
collaborative management with the physi-cian. Based on the assessment data,
potential complications that may develop include:
·
Angina or anginal pain equivalent
·
Severe anxiety requiring an
anxiolytic (anxiety-reducing) medication
·
Cardiac arrest
Planning and Goals
The
major goals of the patient may include reducing fear, learn-ing about the
surgical procedure and postoperative course, and avoiding complications.
Nursing Interventions
During
the preoperative phase of cardiac surgery, the nurse devel-ops a plan of care
that includes emotional support and teaching for the patient and family.
Establishing rapport, answering questions, listening to fears and concerns,
clarifying misconceptions, and pro-viding information about what to expect are
interventions the nurse uses to prepare the patient and family emotionally for
the surgery and for the postoperative events.
REDUCING FEAR
The
patient and family are provided time and opportunities to express their fears.
If there is fear of the unknown, other surgical experiences that the patient
has had can be compared with the impending surgery. It is often helpful to
describe to the patient the sensations that are expected. If the patient has
already had a cardiac catheterization, the similarities and differences between
that procedure and the surgery may be compared. The patient is encouraged to
talk about any concerns related to previous experiences.
A
discussion of the patient’s fears about pain is initiated. A comparison is made
between the pain experienced with cardiac surgery and other pain experiences.
The preoperative sedation, the anesthetic, and the postoperative pain
medications are described. The nurse reassures the patient that the fear of
pain is normal, that some pain will be experienced, that medication to relieve
pain will be provided, and that the patient will be closely observed. The
pa-tient is encouraged to take pain medication before the pain be-comes severe.
Positioning and relaxation will make the pain more tolerable. Patients who have
a fear of scarring from surgery are en-couraged to discuss this concern, and
misconceptions are cor-rected. It may be helpful to indicate that the health
care team members will keep the patient informed about the healing process.
The
patient and family are encouraged to talk about their fear of the patient
dying. They should be reassured that this fear is nor-mal. For those who only
hint about this concern despite efforts to encourage them to talk about their
fear, coaching may be helpful (eg, “Are you worrying about not making it
through surgery? Most people who have heart surgery at least think about the
pos-sibility of dying.”). After the fear is expressed, the patient and family
can be helped to explore their feelings.
By
alleviating undue anxiety and fear, preparing the patient emotionally for
surgery decreases the chance of preoperative problems, promotes smooth
anesthesia induction, and enhances the patient’s involvement in care and
recovery after surgery. Preparing the family for the events to come helps them
to cope, be supportive to the patient, and participate in postoperative and
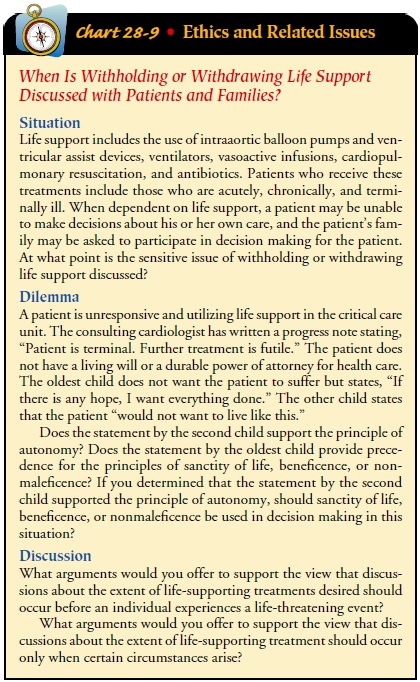
rehabilitative care (Chart 28-9).
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Angina may occur because of increased stress and anxiety related to the forthcoming surgery. The patient who develops angina usually responds to normal angina therapy, most commonly nitro-glycerin. Some patients require oxygen and intravenous nitro-glycerin drips (see the Angina Pectoris section).
For
patients with extreme anxiety or fear and for whom emo-tional support and
education are not successful, medication therapy may be helpful. The anxiolytic
agents most commonly used before cardiac surgery are lorazepam (Ativan) and
diazepam (Valium).
If
cardiac arrest occurs in the preoperative period, advanced cardiac life support
is provided.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patient
and family teaching is based on assessed learning needs. Teaching usually
includes information about hospitalization, surgery (eg, preoperative and
postoperative care, length of surgery, pain and discomfort that can be
expected, visiting hours, and pro-cedures in the critical care unit), the
recovery phase (eg, length of hospitalization, what to expect from home care
and rehabilitation, when normal activities such as housework, shopping, and
work can be resumed), and ongoing lifestyle habits. Any changes made in medical
therapy and preoperative preparations need to be explained and reinforced.
The
patient is informed that physical preparation usually in-volves several showers
or scrubs with an antiseptic solution. A sedative may be prescribed the night
before and the morning ofsurgery. Most cardiac surgical teams use prophylactic
antibiotic therapy, and the antibiotic therapy is initiated before surgery.
If
no preadmission teaching has been done and the preopera-tive hospitalization
period is very short, teaching the patient and family together may be most
effective. Anxiety often increases with the admission process and impending
surgery. Teaching the patient and family together capitalizes on their
established sup-port relationship. Teaching in this phase should be directed
pri-marily by the patient’s and family’s questions. Too much detail may only
increase anxiety.
The
patient may be offered a tour of the critical care unit, the postanesthesia
care unit, or both. (In some hospitals, the patient initially goes to the
postanesthesia care unit.) The patient recov-ering from anesthesia may be
reassured by having already seen the surroundings and having met someone from
the unit. The pa-tient and family are informed about the equipment, tubes, and
lines that will be present after surgery and their purposes. They should know
to expect monitors, several intravenous lines, chest tubes, and a urinary
catheter. Explaining the purpose and the approximate time that these devices
will be in place helps to re-assure the patient. Most patients will remain
intubated and on mechanical ventilation for 2 to 24 hours after surgery. They
need to be aware that this prevents them from talking, and they should be
reassured that the staff will be able to assist them with other means of
communication.
The
nurse takes care to answer the patient’s questions about postoperative care and
procedures. Deep breathing and huffing (or coughing), use of the incentive
spirometer, and foot exercises are explained and practiced by the patient
before surgery. The family’s questions at this time usually focus on the length
of the surgery, who will discuss the results of the procedure with them after
surgery and when this may occur, where to wait during the surgery, the visiting
procedures for the critical care unit, and how they can support the patient
before surgery and in the critical care unit.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1)
Demonstrates reduced fear
a)
Identifies fears
b)
Discusses fears with family
c)
Uses past experiences as a focus for
comparison
d)
Expresses positive attitude about
outcome of surgery
e)
Expresses confidence in measures to
be used to relieve pain
2)
Learns about the surgical procedure
and postoperative course
a)
Identifies the purposes of the
preoperative preparation procedure
b)
Tours the critical care unit, if
desired
c)
Identifies limitations expected
after surgery
d)
Discusses expected immediate
postoperative environment (eg, tubes, machines, nursing surveillance)
e)
Demonstrates expected activities
after surgery (eg, deep breathing, huffing [coughing], foot exercises)
3)
Shows no evidence of complications
a)
Reports anginal pain is relieved
with medications and rest
b)
Takes medications as prescribed
Related Topics