Chapter: Medical Surgical Nursing: Management of Patients With Coronary Vascular Disorders
Angina Pectoris - Coronary Artery Disease
ANGINA PECTORIS
Angina
pectoris is a clinical syndrome usually characterized by episodes or paroxysms
of pain or pressure in the anterior chest. The cause is usually insufficient
coronary blood flow. The insufficient flow results in a decreased oxygen supply
to meet an increased myocardial demand for oxygen in response to physical
exertion or emotional stress. In other words, the need for oxygen exceeds the
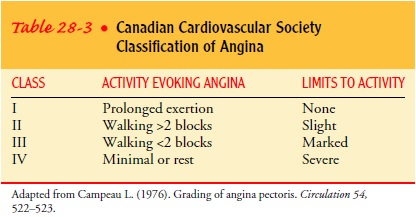
supply. The severity of angina is based on the precipitating activity and its
effect on the activities of daily living (Table 28-3).
Pathophysiology
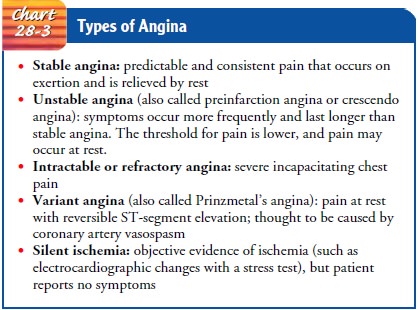
Angina is usually caused by atherosclerotic disease. Almost in-variably, angina is associated with a significant obstruction of a major coronary artery. The characteristics of the various types of angina are listed in Chart 28-3.
Identifying angina requires ob-taining a thorough history. Effective treatment
begins with re-ducing the demands placed on the heart and teaching the patient
about the condition. Several factors are associated with typical anginal pain:
·
Physical exertion, which can
precipitate an attack by in-creasing myocardial oxygen demand
·
Exposure to cold, which can cause
vasoconstriction and an elevated blood pressure, with increased oxygen demand
·
Eating a heavy meal, which increases
the blood flow to the mesenteric area for digestion, thereby reducing the blood
supply available to the heart muscle (In a severely com-promised heart,
shunting of blood for digestion can be suf-ficient to induce anginal pain.)
· Stress or any emotion-provoking situation, causing the re-lease of adrenaline and increasing blood pressure, which may accelerate the heart rate and increase the myocardial workload Atypical angina is not associated with the listed factors. It may occur at rest.
Clinical Manifestations
Ischemia
of the heart muscle may produce pain or other symp-toms, varying in severity
from a feeling of indigestion to a choking or heavy sensation in the upper
chest that ranges from discomfort to agonizing pain accompanied by severe
apprehension and a feeling of impending death. The pain is often felt deep in
the chest behind the upper or middle third of the sternum (retrosternal area). Typically,
the pain or discomfort is poorly localized and may radiate to the neck, jaw,
shoulders, and inner aspects of the upper arms, usually the left arm. The
patient often feels tight-ness or a heavy, choking, or strangling sensation
that has a vise-like, insistent quality. The patient with diabetes mellitus may
not have severe pain with angina because the neuropathy that ac-companies
diabetes can interfere with neuroreceptors, dulling the patient’s perception of
pain.
A
feeling of weakness or numbness in the arms, wrists, and hands may accompany
the pain, as may shortness of breath, pallor, diaphoresis, dizziness or
lightheadedness, and nausea and vomiting. These symptoms may also appear alone
and still rep-resent myocardial ischemia. When these symptoms appear alone,
they are called angina-like symptoms. Anxiety may accompany angina. An
important characteristic of angina is that it abates or subsides with rest or
nitroglycerin.
Gerontologic Considerations
The
elderly person with angina may not exhibit the typical pain profile because of
the diminished responses of neurotransmitters that occur in the aging process.
Often, the presenting symptom in the elderly is dyspnea. If they do have pain,
it is atypical pain that radiates to both arms rather than just the left arm.
Sometimes, there are no symptoms (“silent” CAD), making recognition and
diagnosis a clinical challenge. Elderly patients should be encour-aged to
recognize their chest pain–like symptom (eg, weakness) as an indication that
they should rest or take prescribed medica-tions. Noninvasive stress testing
used to diagnose CAD may not be as useful in elderly patients because of other
conditions (eg, peripheral vascular disease, arthritis, degenerative disk
disease, physical disability, foot problems) that limit the patient’s ability
to exercise.
Assessment and Diagnostic Findings
The
diagnosis of angina is often made by evaluating the clinical manifestations of
ischemia and the patient’s history. A 12-lead ECG and blood laboratory values
help in making the diagnosis. The patient may undergo an exercise or
pharmacologic stress test in which the heart is monitored by ECG,
echocardiogram, or both. The patient may also be referred for an
echocardiogram, nuclear scan, or invasive procedures (cardiac catheterization
and coronary artery angiography).
CAD
is believed to result from inflammation of the arterial endothelium. C-reactive
protein (CRP) is a marker for inflam-mation of vascular endothelium. High blood
levels of CRP have been associated with increased coronary artery calcification
and risk of an acute cardiovascular event (eg, MI) in seemingly healthy
in-dividuals (Ridker et al., 2002; Wang et al., 2002). There is inter-est in
using CRP blood levels as an additional risk factor for cardiovascular disease
in clinical use and research, but the clini-cal value of CRP levels has not
been fully established. The ability of CRP to predict cardiovascular disease
when adjusted for other risk factors, how CRP levels can guide patient
management, and if patient outcomes improve when using CRP levels must be
es-tablished before CRP levels are used routinely for patient care (Mosca,
2002).
An
elevated blood level of homocysteine, an amino acid, has also been proposed as
an independent risk factor for cardio-vascular disease. However, studies have
not supported the relation-ship between mild to moderate elevations of
homocysteine and atherosclerosis (Homocysteine Studies Collaboration, 2002). No
study has yet shown that reducing homocysteine levels reduces the risk of CAD.
Medical Management
The
objectives of the medical management of angina are to de-crease the oxygen
demand of the myocardium and to increase the oxygen supply. Medically, these
objectives are met through phar-macologic therapy and control of risk factors.
Revascularization
procedures to restore the blood supply to the myocardium include percutaneous coronary interventional(PCI) procedures
(eg, percutaneous transluminal coronary
angioplasty [PTCA], intracoronary stents, and atherectomy),CABG, and
percutaneous transluminal myocardial revascular-ization (PTMR).
PHARMACOLOGIC THERAPY
Among
medications used to control angina are nitroglycerin, beta-adrenergic blocking
agents, calcium channel blockers, and antiplatelet agents.
Nitroglycerin.
Nitrates
remain the mainstay for treatment ofangina pectoris. A vasoactive agent,
nitroglycerin (Nitrostat, Nitrol, Nitrobid IV) is administered to reduce
myocardial oxygen consumption, which decreases ischemia and relieves pain.
Nitro-glycerin dilates primarily the veins and, in higher doses, also dilates
the arteries. It helps to increase coronary blood flow by preventing
vasospasm and increasing perfusion through the col-lateral vessels.
Dilation
of the veins causes venous pooling of blood through-out the body. As a result,
less blood returns to the heart, and fill-ing pressure (preload) is reduced. If
the patient is hypovolemic (does not have adequate circulating blood volume),
the decrease in filling pressure can cause a significant decrease in cardiac
out-put and blood pressure.
Nitrates
in higher doses also relax the systemic arteriolar bed and lower blood pressure
(decreased afterload). Nitrates may in-crease blood flow to diseased coronary
arteries and through col-lateral coronary arteries, arteries that have been
underused until the body recognizes poorly perfused areas. These effects
decrease myo-cardial oxygen requirements and increase oxygen supply, bringing
about a more favorable balance between supply and demand.
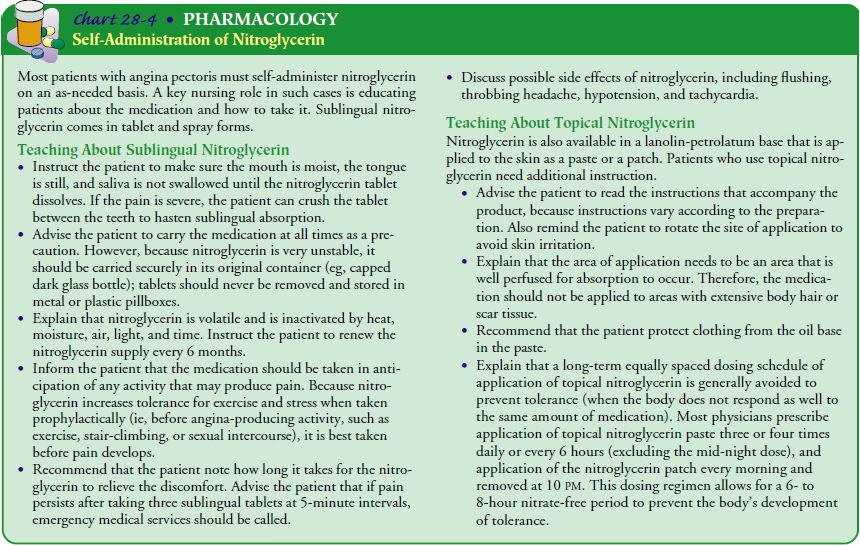
Nitroglycerin
may be given by several routes: sublingual tablet or spray, topical agent, and
intravenous administration. Sublingual nitroglycerin is generally placed under
the tongue or in the cheek (buccal pouch) and alleviates the pain of ischemia
within 3 min-utes. Topical nitroglycerin is also fast acting and is a
convenient way to administer the medication. Both routes are suitable for
pa-tients who self-administer the medication. Chart 28-4 provides more
information.
A
continuous or intermittent intravenous infusion of nitro-glycerin may be
administered to the hospitalized patient with re-curring signs and symptoms of
ischemia or after a revascularization procedure. The amount of nitroglycerin
administered is based on the patient’s symptoms while avoiding side effects
such as hy-potension. It usually is not given if the systolic blood pressure is
90 mm Hg or less. Generally, after the patient is symptom free, the
nitroglycerin may be switched to a topical preparation within 24 hours.
Beta-Adrenergic Blocking Agents.
Beta-blockers such as propran-olol (Inderal), metoprolol
(Lopressor, Toprol), and atenolol (Tenormin) appear to reduce myocardial oxygen
consumption by blocking the beta-adrenergic sympathetic stimulation to the
heart. The result is a reduction in heart rate, slowed conduction of an impulse
through the heart, decreased blood pressure, and reduced myocardial contractility (force of contraction)
that es-tablishes a more favorable balance between myocardial oxygen needs
(demands) and the amount of oxygen available (supply). This helps to control
chest pain and delays the onset of ischemia during work or exercise.
Beta-blockers reduce the incidence of recurrent angina, infarction, and cardiac
mortality. The dose can be titrated to achieve a resting heart rate of 50 to 60
beats per minute.
Cardiac side effects and possible contraindications include hy-potension, bradycardia, advanced atrioventricular block, and de-compensated heart failure. If a beta-blocker is given intravenously for an acute cardiac event, the ECG, blood pressure, and heart rate are monitored closely after the medication has been administered. Because some beta-blockers also affect the beta-adrenergic recep-tors in the bronchioles, causing bronchoconstriction, they are con-traindicated in patients with significant pulmonary constrictive diseases, such as asthma. Other side effects include worsening of hyperlipidemia, depression, fatigue, decreased libido, and mask-ing of symptoms of hypoglycemia. Patients taking beta-blockers are cautioned not to stop taking them abruptly, because angina may worsen and MI may develop. Beta-blocker therapy needs to be decreased gradually over several days before discontinuing it. Patients with diabetes who take beta-blockers are instructed to as-sess their blood glucose levels more often and to observe for signs and symptoms of hypoglycemia.
Calcium Channel Blocking Agents.
Calcium channel blockers(calcium ion antagonists) have different
effects. Some decrease sinoatrial node automaticity and atrioventricular node
conduc-tion, resulting in a slower heart rate and a decrease in the strength of
the heart muscle contraction (negative inotropic effect). These effects
decrease the workload of the heart. Calcium channel block-ers also relax the
blood vessels, causing a decrease in blood pres-sure and an increase in
coronary artery perfusion. Calcium channel blockers increase myocardial oxygen
supply by dilating the smooth muscle wall of the coronary arterioles; they
decrease myocardial oxygen demand by reducing systemic arterial pressure and
the workload of the left ventricle.
The
calcium channel blockers most commonly used are am-lodipine (Norvasc),
verapamil (Calan, Isoptin, Verelan), and dilti-azem (Cardizem, Dilacor,
Tiazac). They may be used by patients who cannot take beta-blockers, who
develop significant side effects from beta-blockers or nitrates, or who still
have pain despite beta-blocker and nitroglycerin therapy. Calcium channel
blockers are used to prevent and treat vasospasm, which commonly occurs after
an invasive interventional procedure. Use of short-acting nifedi-pine
(Procardia) was found to be poorly tolerated and to increase the risk of MI in
patients with hypertension and the risk of death in patients with acute coronary syndrome (Braunwald et
al., 2000; Furberg et al., 1996; Ryan et al., 1999).
First-generation
calcium channel blockers should be avoided or used with great caution in people
with heart failure, because they decrease myocardial contractility. Amlodipine
(Norvasc) and felodipine (Plendil) are the calcium channel blockers of choice
for patients with heart failure. Hypotension may occur after the intra-venous
administration of any of the calcium channel blockers. Other side effects that
may occur include atrioventricular blocks, bradycardia, constipation, and
gastric distress.
Antiplatelet and Anticoagulant Medications.
Antiplatelet med-ications are administered to prevent platelet
aggregation, which impedes blood flow.
Aspirin.
Aspirin
prevents platelet activation and reduces the in-cidence of MI and death in
patients with CAD. A 160- to 325-mg dose of aspirin should be given to the
patient with angina as soon as the diagnosis is made (eg, in the emergency room
or physician’s office) and then continued with 81 to 325 mg daily. Although it
may be one of the most important medications in the treatment of CAD, aspirin
may be overlooked because of its low cost and common use. Patients should be
advised to continue aspirin even if concurrently taking nonsteroidal
anti-inflammatory drugs (NSAIDs) or other analgesics. Because aspirin may cause
gastro-intestinal upset and bleeding, treatment of Helicobacter pylori and the use of H2-blockers (eg, cimetidine
[Tagamet], famotidine [My-lanta AR, Pepcid], ranitidine [Zantac]) or misoprostol
(Cytotec) should be considered to allow continued aspirin therapy.
Clopidogrel and Ticlopidine.
Clopidogrel (Plavix) or ticlopidine(Ticlid) is given to patients
who are allergic to aspirin or given in addition to aspirin in patients at high
risk for MI. Unlike aspirin, these medications take a few days to achieve their
antiplatelet effect. They also cause gastrointestinal upset, including nausea,
vomiting, and diarrhea, and they decrease the neutrophil level.
Heparin.
Unfractionated
heparin prevents the formation of newblood clots. Use of heparin alone in
treating patients with unstable angina reduces the occurrence of MI. If the
patient’s signs and symptoms indicate a significant risk for a cardiac event,
the patient is hospitalized and may be given an intravenous bolus of heparin
and started on a continuous infusion or given an intravenous bolus every 4 to 6
hours. The amount of heparin administered is based on the results of the
activated partial thromboplastin time (aPTT). Heparin therapy is usually considered
therapeutic when the aPTT is 1.5 to 2 times the normal aPTT value.
A
subcutaneous injection of low-molecular-weight heparin (LMWH; enoxaparin
[Lovenox] or dalteparin [Fragmin]) may be used instead of intravenous
unfractionated heparin to treat patients with unstable angina or non–ST-segment
elevation MIs. LMWH provides more effective and stable anticoagulation,
potentially reducing the risk of rebound ischemic events, and it eliminates the
need to monitor aPTT results (Cohen, 2001). LMWH may be beneficial before and
during PCIs and for ST-segment elevation MIs.
Because
unfractionated heparin and LMWH increase the risk of bleeding, the patient is
monitored for signs and symptoms of external and internal bleeding, such as low
blood pressure, an in-creased heart rate, and a decrease in serum hemoglobin
and hematocrit values. The patient receiving heparin is placed on bleeding
precautions, which include:
·
Applying pressure to the site of any
needle puncture for a longer time than usual
·
Avoiding intramuscular injections
·
Avoiding tissue injury and bruising
from trauma or use of constrictive devices (eg, continuous use of an automatic
blood pressure cuff)
A
decrease in platelet count or skin lesions at heparin injection sites may
indicate heparin-induced thrombocytopenia (HIT), an antibody-mediated reaction
to heparin that may result in throm-bosis (Hirsh et al., 2001). Patients who
have received heparin within the past 3 months and those who have been
receiving un-fractionated heparin for 5 to 15 days are at high risk for HIT.
GPIIb/IIIa Agents.
Intravenous
GPIIb/IIIa agents (abciximab[ReoPro], tirofiban [Aggrastat], eptifibatide
[Integrelin]) are indi-cated for hospitalized patients with unstable angina and
as adjunct therapy for PCI. These agents prevent platelet aggregation by
blocking the GPIIb/IIIa receptors on the platelet, preventing adhesion of
fibrinogen and other factors that crosslink platelets to each other and thereby
allow platelets to form a thrombus (clot). As with heparin, bleeding is the
major side effect, and bleeding pre-cautions should be initiated.
Oxygen Administration.
Oxygen therapy is usually initiated atthe onset of chest pain in
an attempt to increase the amount of oxygen delivered to the myocardium and to
decrease pain. Oxy-gen inhaled directly increases the amount of oxygen in the
blood. The therapeutic effectiveness of oxygen is determined by observ-ing the
rate and rhythm of respirations. Blood oxygen saturation is monitored by pulse
oximetry; the normal oxygen saturation (SpO2) level is greater than 93%. Studies are being conducted to assess
the use of oxygen in patients without respiratory distress and its effect on
outcome.
ALTERNATIVE THERAPIES
Researchers
have reported significant improvement in the exer-cise endurance of patients
with angina who were treated with acupuncture as well as with an intravenous
infusion of a combina-tion of ginseng (Panax
quinquefolium), astragalus (Astragalus
mem-branaceus), and angelica (Angelica
sinensis) (Ballegaard et al., 1991;Reichter et al., 1991). Coenzyme Q10 was
advocated for prevent-ing the occurrence and progression of heart failure
(Khatta et al., 2000). However, there have not been large, randomized,
placebo-controlled studies that identify the direct beneficial effect from these
therapies.
Related Topics