Chapter: Medical Surgical Nursing: Management of Patients With Coronary Vascular Disorders
Nursing Process: The Patient Who Has Had Cardiac Surgery
NURSING PROCESS: THE PATIENT WHO HAS HAD CARDIAC SURGERY
Initial
postoperative care focuses on achieving or maintaining hemodynamic stability
and recovery from general anesthesia. Care may be provided in the
postanesthesia care unit or inten-sive care unit. After hemodynamic stability
and recovery from general anesthesia have been achieved, the patient is
transferred to a surgical stepdown unit with telemetry. Care focuses on wound
care, progressive activity, and nutrition. Education about medications and risk
factor modification is emphasized (see Plan of Nursing Care: Care of the
Patient After Cardiac Surgery). Dis-charge from the hospital usually occurs 3
to 5 days after CABG or 1 to 3 days after MIDCAB. Patients can expect fewer
symptoms from CAD and an improved quality of life. CABG has been shown to
increase the life span of high-risk patients—those with left main artery
blockages, left ventricular dysfunction with multivessel blockages,
three-vessel blockages with one being the left anterior descending artery, and
diabetes (Eagle et al., 1999).
The
immediate postoperative period for the patient who has undergone cardiac
surgery presents many challenges to the health care team. All efforts are made
to facilitate the transition from the operating room to the critical care unit
or PACU with min-imal risk. Specific information about the operation and
impor-tant factors about postoperative management are communicated by the
surgical team and anesthesia personnel to the critical care nurse, who then
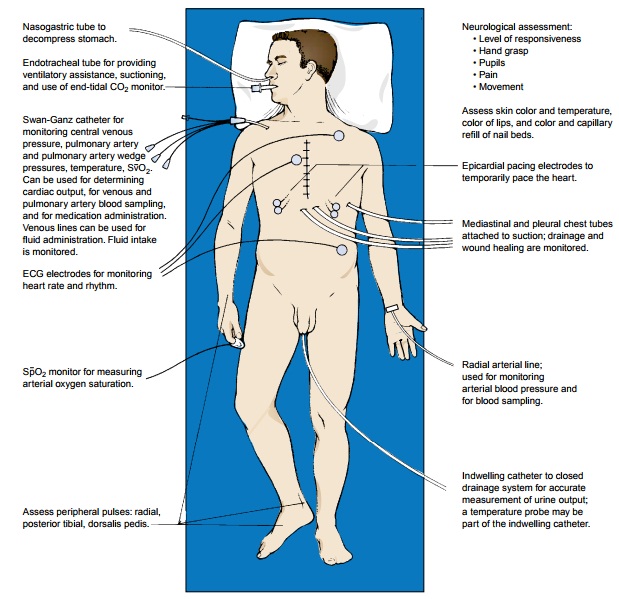
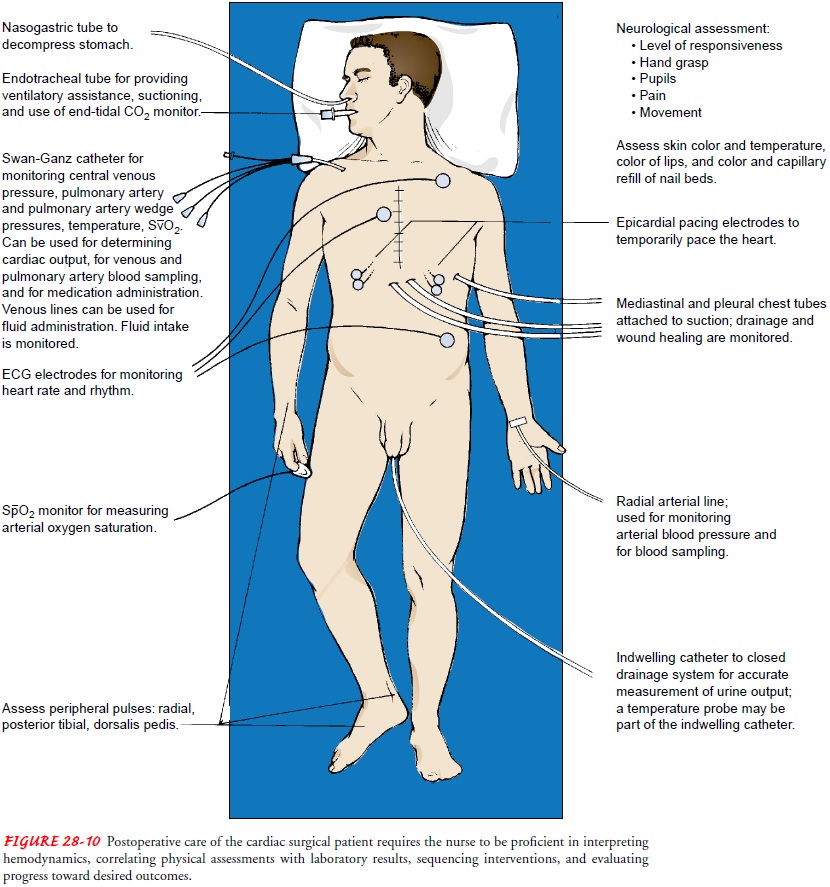
assumes responsibility for the patient’s care. Figure 28-10 presents a graphic
overview of the many aspects of postoperative care for the cardiac surgical
patient.
Assessment
When
the patient is admitted to the critical care unit or PACU and for at least
every 12 hours thereafter, a complete assessment of all systems is performed to
determine the postoperative status of the patient compared with the
preoperative baseline and to identify anticipated changes since surgery. The
following param-eters are assessed:
Neurologic status: level
of responsiveness, pupil size and reactionto light, reflexes, facial symmetry,
movement of extremities, and hand grip strength
Cardiac status: heart
rate and rhythm, heart sounds, arterialblood pressure, central venous pressure
(CVP), pulmonary artery pressure, pulmonary artery wedge pressure (PAWP), left
atrial pressure, waveforms from the invasive blood pres-sure lines, cardiac
output or index, systemic and pulmonary vascular resistance, pulmonary artery
oxygen saturation (SvO2) if
available, mediastinal chest tube drainage, and pacemaker status and function
Respiratory status: chest
movement, breath sounds, ventilatorsettings (eg, rate, tidal volume, oxygen
concentration, mode such as synchronized intermittent mandatory ventilation,
positive end-expiratory pressure, pressure support), respira-tory rate,
ventilatory pressure, arterial oxygen saturation (SaO2),
percutaneous oxygen saturation (SpO2),
end-tidal CO2, pleural chest tube drainage,
arterial blood gases
Peripheral vascular status: peripheral
pulses; color of skin,nailbeds, mucosa, lips, and earlobes; skin temperature;
edema; condition of dressings and invasive lines
Renal function: urinary
output; urine specific gravity and os-molality may be assessed
Fluid and electrolyte status: intake,
output from all drainagetubes, all cardiac output parameters, and the following
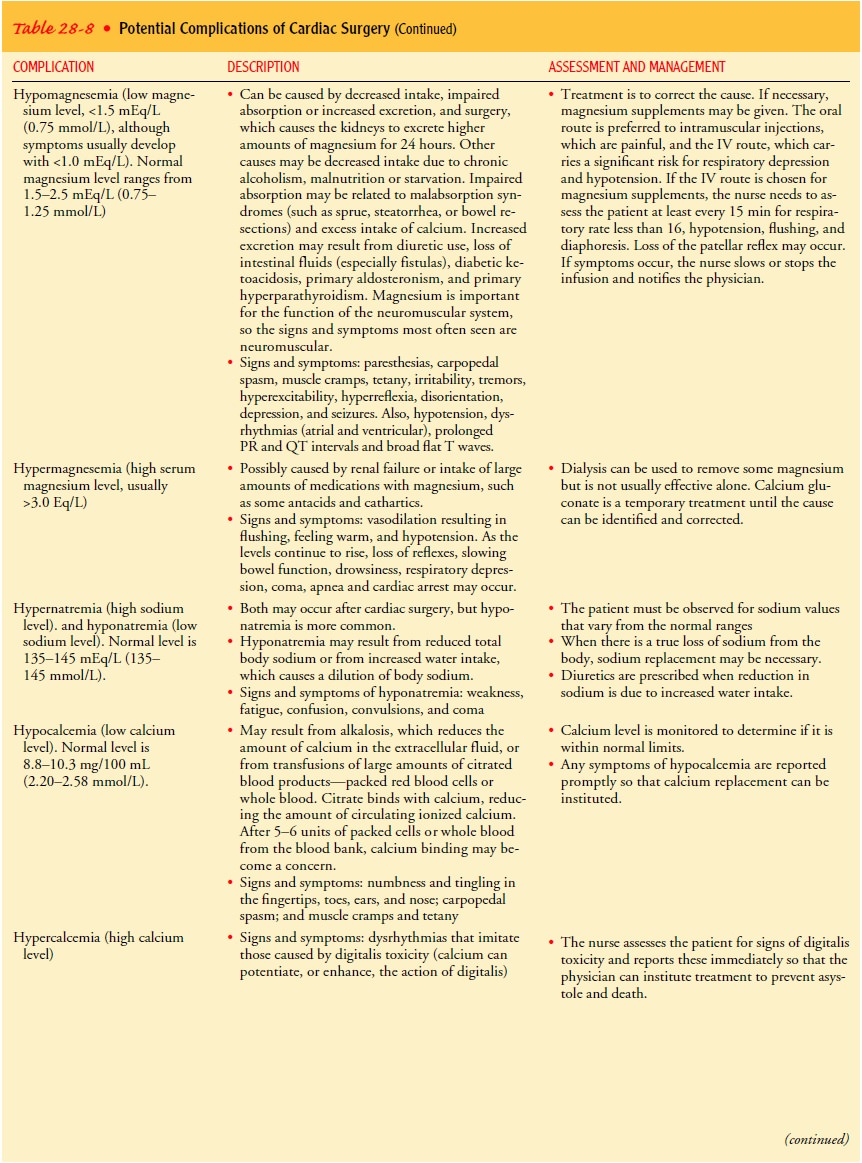
indications of electrolyte imbalance:
·
Hypokalemia:
digitalis toxicity, dysrhythmias, ECGchanges (U wave,
atrioventricular block, flat or inverted T waves)
·
Hyperkalemia:
mental confusion, restlessness, nausea,weakness,
paresthesias of extremities, dysrhythmias, ECG changes (tall, peaked T waves;
increased ampli-tude, widening QRS complex; prolonged QT interval)
·
Hypomagnesemia:
paresthesias, carpopedal spasm, musclecramps, tetany,
irritability, tremors, hyperexcitability, hyperreflexia, cardiac dysrhythmias,
ECG changes (pro-longed PR and QT intervals; broad, flat T waves),
dis-orientation, depression, hypotension, seizures
·
Hypermagnesemia:
vasodilation, hypotension, hypore-flexia, slow
gastrointestinal motility (hypoactive bowel sounds), lethargy, respiratory
depression, coma, apnea, cardiac arrest
·
Hyponatremia:
weakness, fatigue, confusion, seizures,coma
·
Hypocalcemia:
paresthesias, carpopedal spasm, musclecramps, tetany
·
Hypercalcemia:
digitalis toxicity, asystole
Pain: nature,
type, location, duration (incisional pain must bedifferentiated from anginal
pain); apprehension; response to analgesics
Some
patients who have had a MIDCAB using a midsternal incision or an internal
mammary artery CABG experience ulnar nerve paresthesia on the same side of the
body as the graft. The paresthesia may be temporary or permanent. Patients who
have had CABG using the gastroepiploic artery may experience an ileus for a
longer period after surgery and have abdominal pain at the site of the incision
and pain at the site of the chest incision.
Assessment also includes observing all equipment and tubes to determine whether they are functioning properly: endotracheal tube, ventilator, end-tidal CO2 monitor, SpO2 monitor, pulmonary artery catheter, SvO2 monitor, arterial and intravenous lines, intravenous infusion devices and tubing, cardiac monitor, pacemaker, chest tubes, and urinary drainage system.
As
the patient regains consciousness and progresses through the postoperative
period, the nurse expands the assessment to in-clude parameters indicative of
psychological and emotional sta-tus. The patient may exhibit behavior that
reflects denial or depression or may experience postcardiotomy psychosis.
Charac-teristic signs of psychosis include transient perceptual illusions,
vi-sual and auditory hallucinations, disorientation, and paranoid delusions.
The
family’s needs also should be assessed. The nurse ascertains how they are
coping with the situation; determines their psycho-logical, emotional, and
spiritual needs; and finds out whether they are receiving adequate information
about the patient’s condition.
ASSESSING FOR COMPLICATIONS
The
patient is continuously assessed for indications of impending complications
(Table 28-8). The nurse and the surgeon function collaboratively to identify
early signs and symptoms of complica-tions and to institute measures to reverse
their progression.
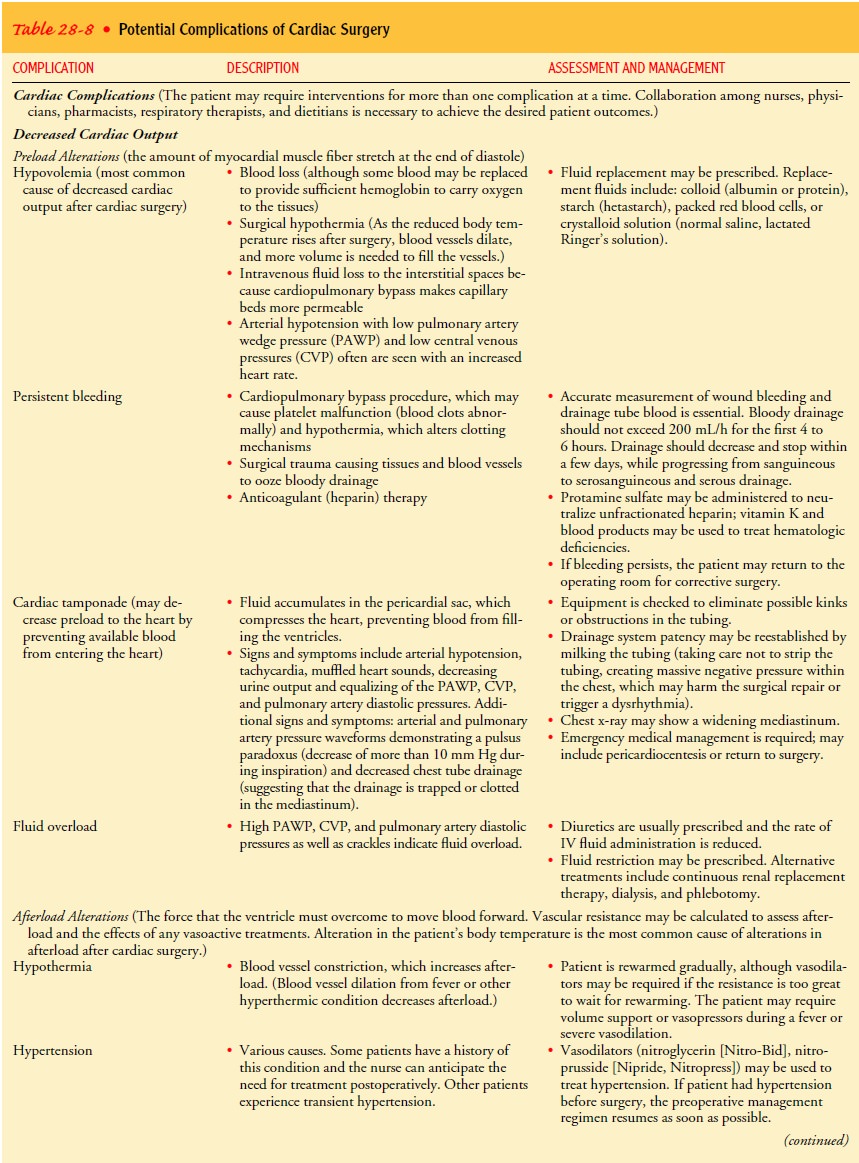
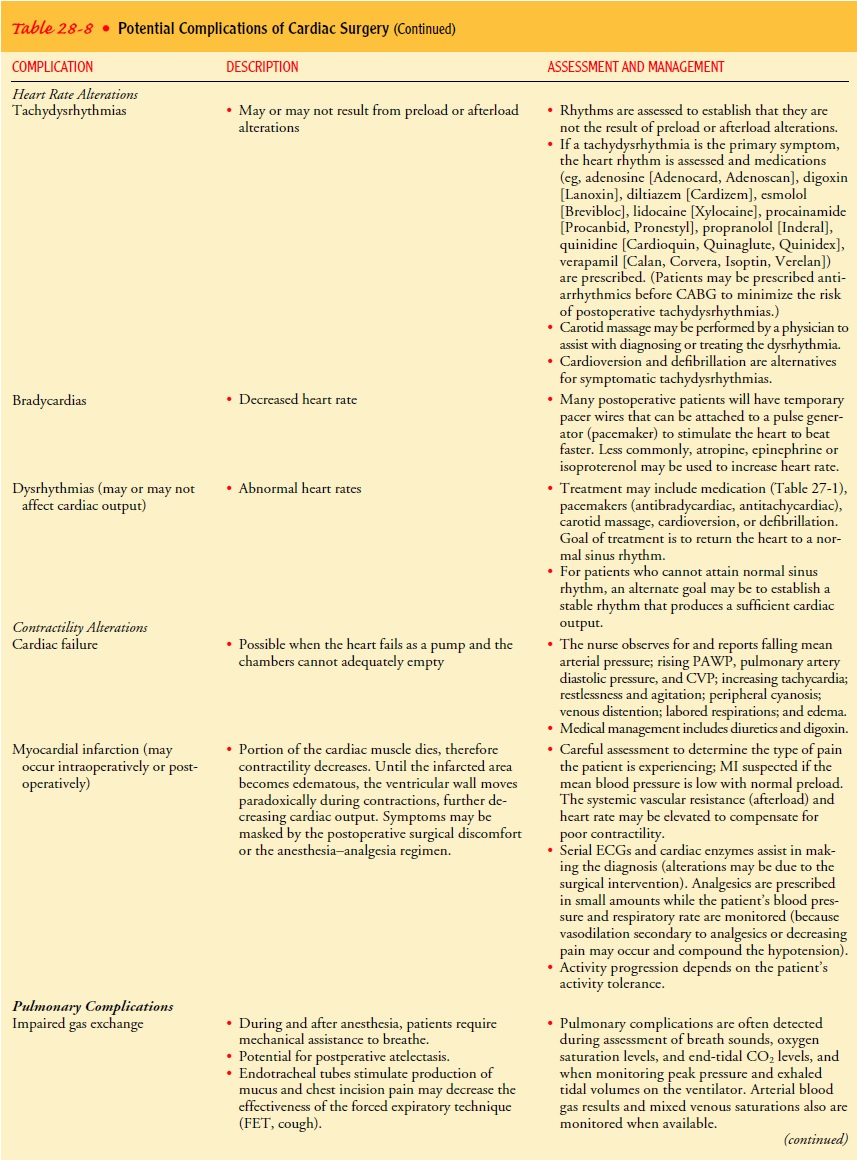
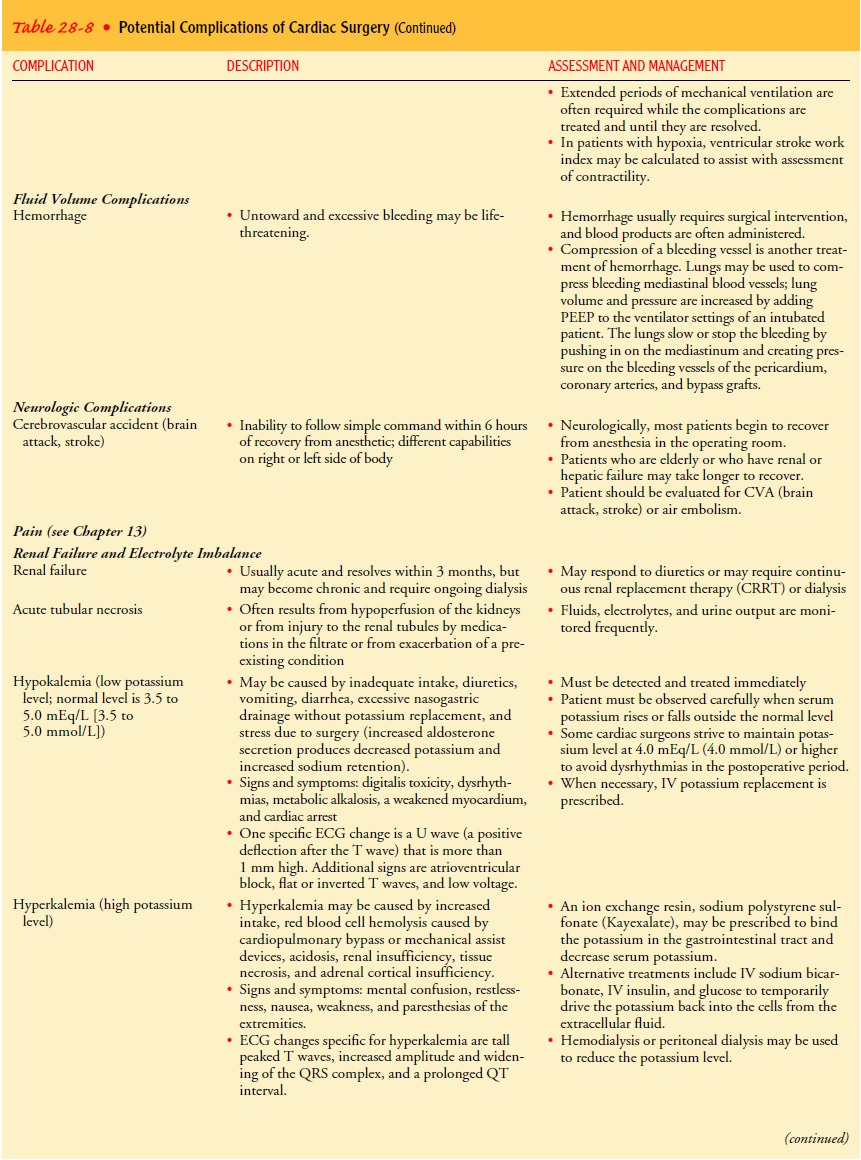
Decreased Cardiac Output
A
decrease in cardiac output is always a threat to the patient who has had
cardiac surgery. It can have a variety of causes:
Preload alterations: too
little or too much blood volume re-turning to the heart because of hypovolemia,
persistent bleeding, cardiac tamponade, or fluid overload
Afterload alteration: hypertension
and arterioles that are tooconstricted or too dilated because of alterations in
body temperature or use of vasoconstrictors
and vasodilators
Heart rate alterations: too
fast, too slow, or dysrhythmias
Contractility alterations: cardiac
failure, MI, electrolyte imbal-ances, hypoxia
Fluid Volume and Electrolyte Imbalance
The
risk for fluid and electrolyte imbalance may occur after car-diac surgery.
Nursing assessment for these complications includes monitoring of intake and
output, weight, PAWP, left atrial pres-sure and CVP readings, hematocrit
levels, distention of neck veins, edema, liver size, breath sounds (eg, fine
crackles, wheezing), and electrolyte levels. Changes in serum electrolytes are
reported promptly so that treatment can be instituted. Especially important are
dangerously high or dangerously low levels of potassium, mag-nesium, sodium,
and calcium.
Impaired Gas Exchange
Impaired
gas exchange is another possible complication after car-diac surgery. All body
tissues require an adequate supply of oxy-gen and nutrients for survival. To
achieve this after surgery, an endotracheal tube with ventilator assistance may
be used for 24 or more hours. The assisted ventilation is continued until the
pa-tient’s blood gas measurements are acceptable and the patient demonstrates
the ability to breathe independently. Patients who are stable after surgery may
be extubated as early as 2 to 4 hours after surgery, which reduces their
anxiety regarding their limited ability to communicate.
The
patient is continuously assessed for signs of impaired gas exchange:
restlessness, anxiety, cyanosis of mucous mem-branes and peripheral tissues,
tachycardia, and fighting the ven-tilator. Breath sounds are assessed often to
detect fluid in the lungs and monitor lung expansion. Arterial blood gas values
are monitored. Arterial blood gases, SpO2,
SaO2, and end-tidal CO2
are assessed for decreased oxygen and increased carbon dioxide.
Impaired Cerebral Circulation
Brain
function depends on a continuous supply of oxygenated blood. The brain does not
have the capacity to store oxygen and must rely on adequate continuous
perfusion by the heart. It is im-portant to observe the patient for any
symptoms of hypoxia: rest-lessness, headache, confusion, dyspnea, hypotension,
and cyanosis. An assessment of the patient’s neurologic status includes level
of consciousness, response to verbal commands and painful stimuli, pupil size
and reaction to light, facial symmetry, movement of ex-tremities, hand grip
strength, presence of pedal and popliteal pulses, and temperature and color of
extremities. Any indication of a changing status is documented, and abnormal
findings are re-ported to the surgeon because they may signal the beginning of
a complication. Hypoperfusion or microemboli may produce cen-tral nervous
system injury after cardiac surgery.
Diagnosis
NURSING DIAGNOSES
Based
on the assessment data and the type of surgical procedure performed, major
nursing diagnoses of the patient may include:
·
Decreased cardiac output related to
blood loss, compro-mised myocardial function, and dysrhythmias
·
Impaired gas exchange related to
trauma of extensive chest surgery
·
Risk for deficient fluid volume (and
electrolyte imbalance) related to alteration in circulating blood volume
·
Disturbed sensory perception (visual
or auditory) related to excessive environmental stimuli (critical care environment,
surgical experience), insufficient sleep, psychological stress, altered sensory
integration, and electrolyte imbalances
·
Acute pain related to surgical
trauma and pleural irritation caused by chest tubes
·
Ineffective tissue perfusion (renal,
cerebral, cardiopulmonary, gastrointestinal, peripheral) related to decreased
cardiac output, hemolysis, vasopressor drug therapy, venous stasis,
embolization, underlying atherosclerotic disease, effects of vasopressors, or
coagulation problems
·
Ineffective thermoregulation related
to infection or post-pericardiotomy syndrome
·
Deficient knowledge about self-care
activities
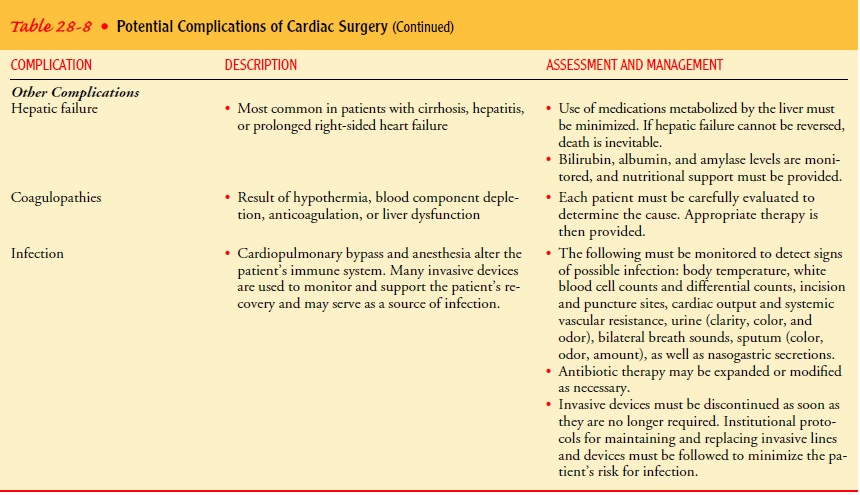
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications that may
develop include:
·
Cardiac complications: heart
failure, MI, stunned myo-cardium, dysrhythmias, tamponade, cardiac arrest
·
Pulmonary complications: pulmonary
edema, pulmonary emboli, pleural effusions, pneumothorax or hemothorax,
respiratory failure, acute respiratory distress syndrome
·
Hemorrhage
·
Neurologic complications: CVA (brain
attack, stroke), air emboli
·
Renal failure, acute or chronic
·
Electrolyte imbalances
·
Hepatic failure
·
Coagulopathies
·
Infection, sepsis
Planning and Goals
The
major goals for the patient include restoration of cardiac out-put, adequate
gas exchange, maintenance of fluid and electrolyte balance, reduction of
symptoms of sensory-perception alterations, relief of pain, maintenance of
adequate tissue perfusion, mainte-nance of normal body temperature, learning
self-care activities, and absence of complications.
Nursing Interventions
RESTORING CARDIAC OUTPUT
Nursing
management of the patient involves continuously ob-serving the patient’s
cardiac status and notifying the surgeon of any changes that indicate decreased
cardiac output. The nurse and the surgeon then work collaboratively to correct
the problem.
In
evaluating the patient’s cardiac status, the nurse primarily determines the
effectiveness of cardiac output through clinical observations and routine measurements:
serial readings of blood pressure, heart rate, CVP, arterial pressure, and left
atrial or pul-monary artery pressure.
Renal
function is related to cardiac function, as blood pressure and heart rate drive
glomerular filtration; therefore, urinary out-put is measured and recorded.
Urine output of less than 25 mL/hr may indicate a decrease in cardiac output.
Urine specific gravity may also be assessed (normal: 1.010 to 1.025), as may
urine osmolality. Inadequate fluid volume may be manifested by low urinary
output and high specific gravity, whereas overhydration is manifested by high
urine output with low specific gravity.
The
growth and function of body cells depend on adequate cardiac output to provide
a continuous supply of oxygenated blood to meet the changing demands of the
organs and body sys-tems. Because the buccal mucosa, nailbeds, lips, and
earlobes are sites with rich capillary beds, they should be observed for
cyanosis or duskiness as possible signs of reduced heart action. Moist or dry
skin may indicate vasodilation or vasoconstriction, respec-tively. Distention
of the neck veins or of the dorsal surface of the hand raised to heart level
may signal a changing demand or di-minishing capacity of the heart. If cardiac
output has fallen, the skin becomes cool, moist, and cyanotic or mottled.
Dysrhythmias,
which may arise when poor perfusion of the heart exists, also serve as
important indicators of cardiac function. The most common dysrhythmias
encountered during the post-operative period are atrial fibrillation,
bradycardias, tachycardias, and ectopic beats. Continuous observation of the
cardiac moni-tor for various dysrhythmias is an essential part of patient care
and management.
Any
indications of decreased cardiac output are reported promptly to the physician.
These assessment data and results of diagnostic tests are used by the physician
to determine the cause of the problem. After a diagnosis has been made, the
physician and the nurse work collaboratively to restore cardiac output and prevent
further complications. When indicated, the physician prescribes blood
components, fluids, digitalis or other antidys-rhythmics, diuretics,
vasodilators, or vasopressors. When additional surgery is necessary, the
patient and family are prepared for the procedure.
PROMOTING ADEQUATE GAS EXCHANGE
To
ensure adequate gas exchange, the nurse assesses and main-tains the patency of
the endotracheal tube. The patient is suc-tioned when wheezes, coarse crackles,
or rhonchi are present. Suctioning may be performed with an in-line suction
catheter; the nurse and respiratory therapist determine if the ventilator’s
fractional inspired oxygen (FIO2)
should be increased for three or more breaths before the patient is suctioned.
Alternatively, 100% oxygen is delivered to the patient by a manual
resuscitation bag (eg, Ambu-Bag) before and after suctioning to minimize the
risk of hypoxia that can result from the suctioning procedure. Arterial blood
gas determinations are compared with baseline data, and changes are reported to
the physician promptly.
Because
a patent airway is essential for oxygen and carbon diox-ide exchange, the
endotracheal tube must be secured to prevent it from slipping into the right
mainstem bronchus and occluding the left bronchus. When the patient’s condition
stabilizes, body posi-tion is changed every 1 to 2 hours. Frequent changes of
patient po-sition provide for optimal pulmonary ventilation and perfusion by
allowing the lungs to expand more fully. The nurse assesses breath sounds to
detect crackles, wheezes, and fluid in the lungs.
The
patient is usually weaned from the ventilator and extu-bated within 24 hours of
CABG. Physical assessment and arterial blood gas results guide the process.
Before being extubated, the patient should have cough and gag reflexes and
stable vital signs; be able to lift the head off the bed or give firm hand
grasps; have adequate vital capacity, negative inspiratory force, and minute
volume appropriate for body size; and have acceptable arterial blood gas levels
while breathing warmed humidified oxygen with-out the assistance of the
ventilator.
Extubation
has been performed within these parameters with-out any adverse effects on the
patient’s condition or prognosis.
During
this time, the nurse assists with the weaning process and eventually with
removal of the endotracheal tube. Deep breath-ing and forced expiration
technique (FET, huffing) or coughing are encouraged at least every 1 to 2 hours
after extubation to open the alveolar sacs and provide for increased perfusion.
FET is the rapid exhalation of a deep breath using the diaphragm and ab-dominal
muscles to force air out through an open mouth and glottis (the glottis is not
held closed then suddenly opened, as in a cough). Patients may experience less
pain with FET than coughing, which may increase the frequency with which a
patient performs the exercises. The patient should be taught and assisted to
splint the chest incision before and during FET or coughing to minimize
discomfort.
MAINTAINING FLUID AND ELECTROLYTE BALANCE
To
promote fluid and electrolyte balance, the nurse carefully assesses intake and
output. Flow sheets are used to determine pos-itive or negative fluid balance.
All fluid intake is recorded, includ-ing intravenous, nasogastric tube, and oral
fluids. All output is recorded, including urine, nasogastric drainage, and
chest drainage.
Hemodynamic
parameters (ie, blood pressure, pulmonary wedge and left atrial pressures, and
CVP) are correlated with in-take, output, and weight to determine the adequacy
of hydra-tion and cardiac output. Serum electrolytes are monitored, and the
patient is observed for signs of potassium, magnesium, sodium, or calcium
imbalance (ie, hypokalemia, hyperkalemia, hypomagnesemia, hyponatremia, or
hypocalcemia).
Any
indications of dehydration, fluid overload, or electrolyte imbalance are
reported promptly, and the physician and nurse work collaboratively to restore
fluid and electrolyte balance. The patient’s response is monitored.
MINIMIZING SENSORY-PERCEPTION IMBALANCE
A
large number of patients experience abnormal behaviors that occur with varying
intensity and duration. In the early years of cardiac surgery, this phenomenon
occurred more frequently than it does today. At that time, it was attributed to
inadequate cere-bral perfusion during surgery, microemboli, and the length of
time that the patient remained on the CPB machine. Advances in surgical
techniques have significantly decreased these factors. Today, when it occurs,
it is thought to be caused by anxiety, sleep deprivation, increased sensory
input, and disorientation to night and day when the patient loses track of time
(Arrowsmith et al., 1999; Braunwald et al., 2001; Fuster et al., 2001). An
important finding is that patients who do not or cannot express anxiety be-fore
surgery and those who are not able to sleep postoperatively are more prone to
develop psychosis in the postoperative period. Psychosis may appear after a 2-
to 5-day lucid interval.
Basic
comfort measures used in conjunction with prescribed analgesics potentiate the
effects of the analgesics and promote rest. The patient is assisted in changing
positions every 1 to 2 hours and is positioned in such a way to avoid strain on
incisions and chest tubes. Nursing care is scheduled as much as possible to
provide undisturbed periods of rest. As the patient’s condition stabilizes and
the patient is disturbed less frequently for monitoring and therapeutic
procedures, rest periods can be extended. As much uninterrupted sleep as
possible is provided, especially during the patient’s normal hours of sleep.
The
nurse monitors the patient for signs of denial and provides an opportunity for
emotional expression during the preoperative period. Careful explanations of
all procedures and of the need for cooperation help to keep the patient
oriented throughout the postoperative course. Continuity of care is desirable;
a familiar face and a nursing staff with a consistent approach promote the
deliv-ery of quality nursing care. A well-designed and individualized plan of
nursing care can assist the nursing team in coordinating their efforts for the
emotional well-being of the patient.
RELIEVING PAIN
Deep
pain may not be reflected in the immediate area of injury but occur in a
broader, more diffuse area. Patients who have had cardiac surgery experience
pain caused by the interruption of in-tercostal nerves along the incision route
and irritation of the pleura by the chest catheters. Incisional pain may also
be experi-enced from peripheral vein or artery graft harvest sites.
It
is essential to observe and listen to the patient for verbal and nonverbal
clues about pain. The nurse accurately records the na-ture, type, location, and
duration of the pain. (Chest incisional pain must be differentiated from
anginal pain.) The patient is en-couraged to use patient-controlled analgesia
or accept medication as often as it is prescribed to reduce the amount of pain.
Physical support of the incision during deep breathing and FET (or cough-ing)
also helps to minimize pain. The patient should then be able to participate in
respiratory exercises and to increase self-care progressively.
Pain
produces tension, which may stimulate the central ner-vous system to release
adrenaline, which results in constriction of the arterioles and increased heart
rate. This can cause increased afterload and decreased cardiac output. Opioids
alleviate anxiety and pain and induce sleep, which reduces the metabolic rate
and oxygen demands. After the administration of opioids, any obser-vations
indicating relief of apprehension and pain are docu-mented in the patient’s
record. The patient is observed for any respiratory depressant effects of the
analgesic. If respiratory de-pression occurs, an opioid antagonist (eg,
naloxone [Narcan]) is used to counteract the effect.
MAINTAINING ADEQUATE TISSUE PERFUSION
Peripheral
pulses (eg, pedal, tibial, popliteal, femoral, radial, brachial) are routinely
palpated to assess for arterial obstruction. If a pulse is absent in any
extremity, the cause may be prior catheterization of that extremity. The newly
identified absence of any pulse is immediately reported to the physician.
Thrombus
formation and resulting embolus formation also can result from injury to the
intima of the blood vessels, dislodg-ing a clot from a damaged valve, loosening
of mural thrombi, and coagulation problems. Air embolism may occur as a result
of CPB or central venous cannulation. Symptoms of embolization vary according
to site. The usual embolic sites are the lungs, coronary arteries, mesentery, spleen,
extremities, kidneys, and brain. The patient is observed for:
·
Chest pain and respiratory distress
with pulmonary embo-lus or MI
·
Midabdominal or midback pain
·
Pain, cessation of pulses,
blanching, numbness, or coldness in an extremity
·
Decreased urine output
·
One-sided weakness and pupillary
changes, as occur in CVAs (brain attacks, strokes)
All
such symptoms are promptly reported to the physician. After surgery, the
following measures are taken to prevent venous stasis, which can cause thrombus
formation and subsequent embolization:
·
Applying elastic compression
stockings or elastic bandage wrap and pneumatic antiembolic stockings
·
Discouraging crossing of legs
·
Avoiding use of the knee gatch on
the bed
·
Omitting pillows in the popliteal
space
·
Instituting passive exercises
followed by active exercises to promote circulation and prevent loss of muscle
tone (pa-tients need to ambulate as early as possible)
Inadequate
renal perfusion can occur as a complication of car-diac surgery. One possible
cause is low cardiac output. Trauma to blood cells during CPB can cause
hemolysis of red blood cells, which then occlude the renal glomeruli. Use of
vasopressor agents to increase blood pressure may constrict the renal
arterioles and reduce blood flow to the kidneys.
Nursing
management includes accurate measurement of urine output. An output of less
than 25 mL/hr may indicate hypo-volemia. Urine specific gravity can be
monitored to determine the kidneys’ ability to concentrate urine in the renal
tubules. Rapid-acting diuretics or inotropic medications (eg, digoxin
[Lanoxin], isoproterenol [Isuprel]) may be prescribed to increase cardiac
out-put and renal blood flow. The nurse should be aware of the pa-tient’s blood
urea nitrogen, serum creatinine, and urine and serum electrolyte levels.
Abnormal levels are reported promptly because it may be necessary to adjust
fluids and the dose or type of med-ication administered. If efforts to maintain
renal perfusion are not effective, the patient may require dialysis or continuous
renal re-placement therapy.
MAINTAINING NORMAL BODY TEMPERATURE
Patients
are usually hypothermic when admitted to the critical care unit from the
cardiac surgical procedure. The patient must be gradually warmed to a normal
temperature. This is accom-plished partially by the patient’s own basal
metabolic processes and often with the assistance of warmed ventilator air,
warm air or warm cotton blankets, or heat lamps. While the patient is
hy-pothermic, the clotting process is less efficient, the heart is prone to
dysrhythmias, and oxygen does not readily transfer from the hemoglobin to the
tissues. Because anesthesia and hypothermia suppress the basal metabolism,
oxygen supply usually meets the cellular demand.
After
cardiac surgery, the patient is at risk for developing ele-vated body
temperature caused by infection or postpericardiotomy syndrome. The resultant
increase in metabolic rate increases tissue oxygen demands and increases
cardiac workload. Measures are taken to prevent this sequence of events or to
halt it as soon as it is recognized.
Sites
of infection include the lungs, urinary tract, incisions, and intravascular
catheters. Meticulous care is used to prevent contamination at the sites of
catheter and tube insertions. Asep-tic technique is used when changing
dressings and when provid-ing endotracheal tube and catheter care. Clearance of
pulmonary secretions is accomplished by frequent repositioning of the patient,
suctioning, and chest physical therapy, as well as teach-ing and encouraging
the patient to breathe deeply and use FET (or cough). Closed systems are used
to maintain all intravenous and arterial lines. All invasive equipment is
discontinued as soon as possible after surgery.
Postpericardiotomy
syndrome occurs in approximately 10% to 40% of patients who undergo cardiac
surgery. Although the pre-cise cause is unknown, a common factor appears to be
trauma, with residual blood in the pericardial sac after surgery. The syn-drome
is characterized by fever, pericardial pain, pleural pain, dyspnea, pericardial
effusion, pericardial friction rub, and arthral-gia. There may be a combination
of these signs and symptoms.
Leukocytosis
occurs, along with elevation of the erythrocyte sedi-mentation rate. These
symptoms frequently appear after the pa-tient is discharged from the hospital.
The
syndrome must be differentiated from other postoperative complications (eg,
infection, incisional pain, MI, pulmonary em-bolus, bacterial endocarditis,
pneumonia, atelectasis). Treatment depends on the severity of the symptoms. Bed
rest and anti-inflammatory agents, such as salicylates and corticosteroids,
produce a dramatic improvement in symptoms.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Depending
on the type of surgery and postoperative progress, the patient may be
discharged from the hospital as early as 1 day after MIDCAB and 3 days after
other surgery. Although the patient may be anxious to return home, the patient
and family usually have apprehensions about this transition. The family members
often express the fear that they are not capable of caring for the patient at
home. They often are concerned that complications will occur that they are
unprepared to handle.
The
nurse helps the patient and family to set realistic, achievable goals. A
teaching plan that meets the patient’s individual needs is developed with the
patient and family. This is done before admission and reviewed each shift
through the hospitalization or with each home care and rehabilitation contact.
Specific instruc-tions are provided about incision care; signs and symptoms of
in-fection; diet; activity progression and exercise; deep breathing, FET (or
coughing), incentive spirometry; and smoking cessation; weight and temperature
monitoring; the medication regimen; and follow-up visits with home care nurses,
the rehabilitation per-sonnel, the surgeon, and the cardiologist or internist.
Some
patients may have difficulty learning and retaining infor-mation after cardiac
surgery. Studies have documented that many patients have difficulties in
cognitive function after cardiac surgery that do not occur after other types of
major surgery (Arrowsmith et al., 1999; Roach et al., 1996). The patient may
experience recent memory loss, short attention span, difficulty with simple
math, poor handwriting, and visual disturbances. Patients with these
dif-ficulties often become frustrated when they try to resume normal activities
and learn how to care for themselves at home. The patient and family are
reassured that the difficulty is temporary and will subside, usually in 6 to 8
weeks. In the meantime, instructions are given to the patient at a much slower
pace than normal, and a fam-ily member assumes responsibility for making sure
that the pre-scribed regimen is followed. All information is provided in
writing in the patient’s primary language.
Continuing Care
Arrangements are made for a home care nurse to provide care when appropriate. Since the length of time that the patient re-mains in the hospital is relatively short, it is particularly impor-tant for the nurse to assess the patient’s and family’s ability to manage care in the home. The education plan is continued by the home care nurse. Vital signs and incisions are monitored, the pa-tient is assessed for signs and symptoms of complications, and support for the patient and family is provided. Additional inter-ventions may include dressing changes, intravenous antibiotic ad-ministration, diet counseling, and tobacco use cessation strategies. Patients and families need to know that cardiac surgery did not cure the patient’s underlying heart disease. Lifestyle changes for risk factor reduction must be made, and medications taken pre-operatively may be prescribed postoperatively.
Patient
teaching does not end at the time of discharge from home health. The patient is
encouraged to maintain telephone contact with the surgeon, cardiologist, and
nurses. This provides the patient and family with reassurance that questions
can be an-swered and problems can be resolved if they arise. Many hospi-tals
provide family support sessions that help family members cope with their own
stress related to the patient’s home health care management. The patient is
expected to have a follow-up visit with the surgeon.
Many
patients and families benefit from supportive programs such as the postcardiac
surgery rehabilitation programs offered by many medical centers. These programs
provide exercise moni-toring; instructions about diet and stress reduction; information
about resuming exercise, work, driving, and sexual activity; assis-tance with
tobacco use cessation; and support groups for pa-tients and families. The
American Heart Association sponsors the Mended Hearts Club, which provides
information as well as an opportunity for families to share experiences.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include the following:
·
Maintains adequate cardiac output
·
Maintains adequate gas exchange
·
Maintains fluid (and electrolyte)
balance
·
Experiences decreased symptoms of
sensory-perception disturbances
·
Experiences relief of pain
·
Maintains adequate tissue perfusion
·
Maintains normal body temperature
·
Performs self-care activities
A
typical plan of postoperative nursing care and more-detailed expected outcomes
for the cardiac surgery patient are presented in the Plan of Nursing Care.
Related Topics