Chapter: Medical Surgical Nursing: Management of Patients With Dysrhythmias and Conduction Problems
Cardiac Conduction Surgery - Adjunctive Modalities and Management
CARDIAC CONDUCTION SURGERY
Atrial
tachycardias and ventricular tachycardias that do not re-spond to medications
and are not suitable for antitachycardia pacing may be treated by methods other
than medications and devices. Such methods include endocardial isolation,
endocardial resection, and ablation. An ICD may be used with these surgical
interventions.
Endocardial Isolation
Endocardial
isolation involves making an incision into the endo-cardium that separates the
area where the dysrhythmia originates from the surrounding endocardium. The
edges of the incision are then sutured together. The incision and its resulting
scar tissue prevent the dysrhythmia from affecting the whole heart.
Endocardial Resection
In
endocardial resection, the origin of the dysrhythmia is identi-fied, and that
area of the endocardium is peeled away. No recon-struction or repair is
necessary.
Catheter Ablation Therapy
Catheter
ablation destroys specific cells that are the cause or cen-tral conduction
method of a tachydysrhythmia. It is performed with or after an EP study. Usual
indications for ablation are AV nodal reentry tachycardia, atrial fibrillation,
or VT unresponsive to previous therapy (or for which the therapy produced
signifi-cant side effects).
Ablation
is also indicated to eliminate accessory AV pathways or bypass tracts that
exist in the hearts of patients with preexcita-tion syndromes such as
Wolff-Parkinson-White (WPW) syn-drome. During normal embryonic development, all
connections between the atrium and ventricles disappear, except for that
be-tween the AV node and the bundle of His. In some people, em-bryonic
connections of normal heart muscle between the atrium and ventricles remain,
providing an accessory pathway or a tract through which the electrical impulse
can bypass the AV node. These pathways can be located in several different
areas. If the pa-tient develops atrial fibrillation, the impulse may be
conducted into the ventricle at a rate of 300 times per minute or more, which
can lead to ventricular fibrillation and sudden cardiac death. Pre-excitation
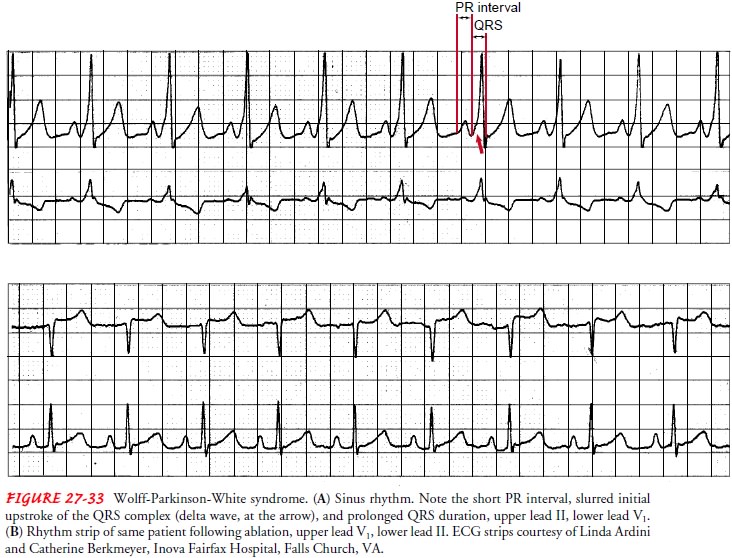
syndromes are identified by specific ECG findings. For example, in WPW syndrome
there is a shortened PR interval, slurring (called a delta wave) of the initial
QRS deflection, and prolonged QRS duration (Fig. 27-33).
Ablation
may be accomplished by three different methods: radiofrequency ablation,
cryoablation, or electrical ablation. The most often used method is radiofrequency,
which involves plac-ing a special catheter at or near the origin of the
dysrhythmia. High-frequency, low-energy sound waves are passed through the
catheter, causing thermal injury and cellular changes that result in localized
destruction and scarring. The tissue damage is more specific to the dysrhythmic
tissue, with less trauma to the sur-rounding cardiac tissue than occurs with
cryoablation or electri-cal ablation.
Cryoablation
involves placing a special probe, cooled to a tem-perature of −60°C
(−76°F), on the endocardium at the site of the dysrhythmia’s
origin for 2 minutes. The tissue freezes and is later replaced by scar tissue,
eliminating the origin of the dysrhythmia.
In
electrical ablation, a catheter is placed at or near the origin of the
dysrhythmia, and one to four shocks of 100 to 300 joules are administered
through the catheter directly to the endocardium and surrounding tissue. The
cardiac tissue burns and scars, thus eliminating the source of the dysrhythmia.
During
the ablation procedure, defibrillation pads, an auto-matic blood pressure cuff,
and a pulse oximeter are used on the patient, and an indwelling urinary
catheter is inserted. The patient is given light sedation. An EP study is
performed and attempts to induce the dysrhythmia are made. The ablation
catheter is placed at the origin of the dysrhythmia, and the ablation procedure
is performed. Multiple ablations may be necessary. Successful abla-tion is
achieved when the dysrhythmia can no longer be induced. The patient is monitored
for another 30 to 60 minutes and then retested to ensure that the dysrhythmia
will not recur.
Postprocedural care is similar to that for an EP study, except that the patient is monitored more closely, depending on the time needed for recovery from sedation.
Related Topics