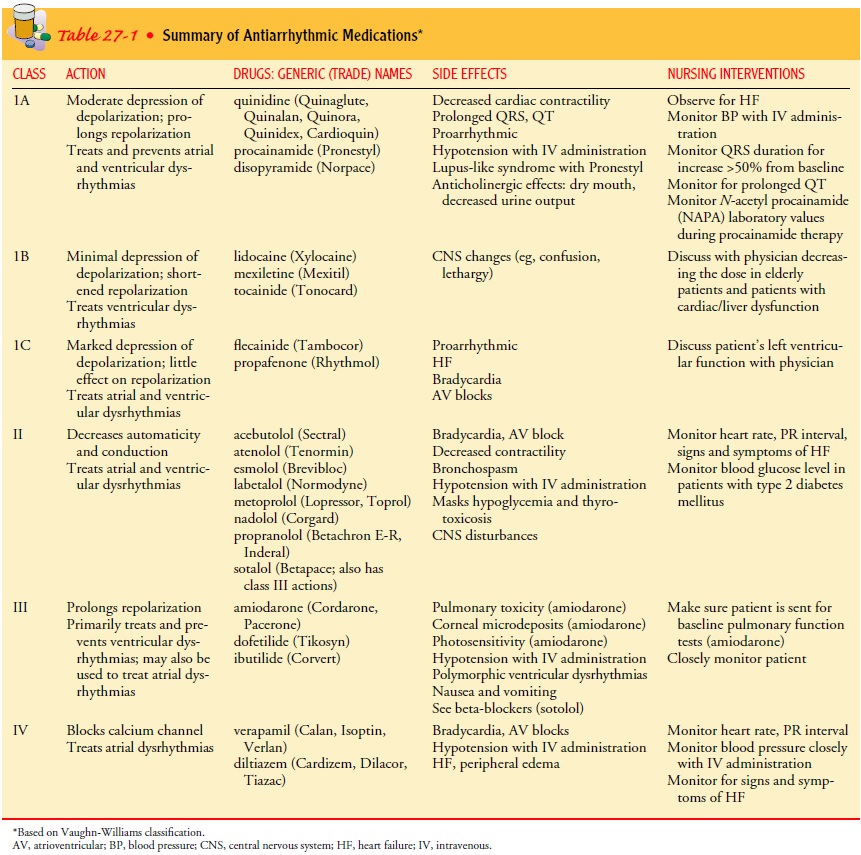
Chapter: Medical Surgical Nursing: Management of Patients With Dysrhythmias and Conduction Problems
Dysrhythmias: Analyzing the Electrocardiogram Rhythm Strip
ANALYZING THE ELECTROCARDIOGRAM RHYTHM STRIP
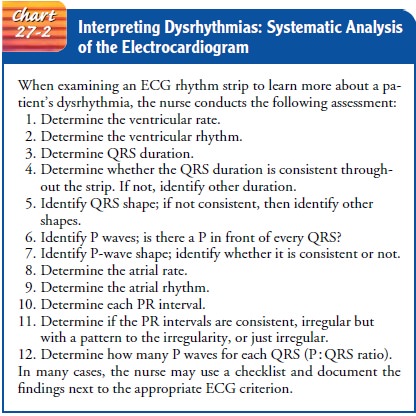
The
ECG must be analyzed in a systematic manner to determine the patient’s cardiac
rhythm and to detect dysrhythmias and con-duction disorders, as well as
evidence of myocardial ischemia, in-jury, and infarction. Chart 27-2 is an
example of a method that can be used to analyze the patient’s rhythm.
Once
the rhythm has been analyzed, the findings are com-pared with and matched to
the ECG criteria for dysrhythmias to determine a diagnosis. It is important for
the nurse to assess the patient to determine the physiologic effect of the
dysrhythmia and to identify possible causes. Treatment of dysrhythmias is based
on the etiology and the effect of the dysrhythmia, not on its presence alone.
Normal Sinus Rhythm
Normal sinus rhythm occurs
when the electrical impulse startsat a regular rate and rhythm in the sinus
node and travels through the normal conduction pathway. The following are the
ECG cri-teria for normal sinus rhythm (Fig. 27-5):
Ventricular and atrial rate: 60
to 100 in the adult
Ventricular and atrial rhythm: Regular
QRS shape and duration: Usually
normal, but may be regularlyabnormal
P wave: Normal and
consistent shape; always in front of the QRS
PR interval: Consistent
interval between 0.12 and 0.20 seconds
P: QRS ratio: 1
1
Types of Dysrhythmias
Dysrhythmias include sinus node, atrial, junctional, and ventric-ular dysrhythmias and their various subcategories.
SINUS NODE DYSRHYTHMIAS
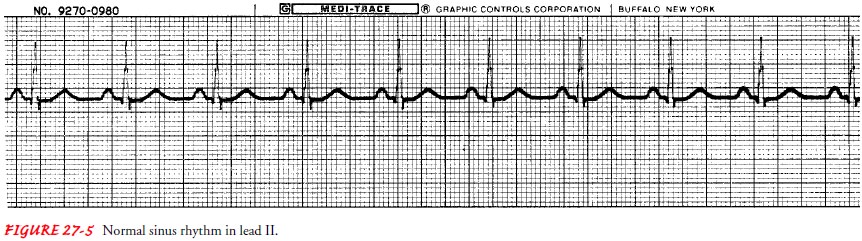
Sinus Bradycardia.
Sinus
bradycardia occurs when the sinus nodecreates an impulse at a
slower-than-normal rate. Causes include lower metabolic needs (eg, sleep,
athletic training, hypothermia, hypothyroidism), vagal stimulation (eg, from
vomiting, suctioning, severe pain, extreme emotions), medications (eg, calcium
channel blockers, amiodarone, beta-blockers), increased intracranial pres-sure,
and myocardial infarction (MI), especially of the inferior wall. The following
are characteristics of sinus bradycardia (Fig. 27-6):
Ventricular and atrial rate: Less
than 60 in the adult
Ventricular and atrial rhythm: Regular
QRS shape and duration: Usually
normal, but may be regularlyabnormal
P wave: Normal and
consistent shape; always in front of the QRS
PR interval: Consistent
interval between 0.12 and 0.20 seconds
P: QRS ratio: 1
1
All
characteristics of sinus bradycardia are the same as those of normal sinus
rhythm, except for the rate. The patient is assessed to determine the
hemodynamic effect and the possible cause of the dysrhythmia. If the decrease
in heart rate results from stimu-lation of the vagus nerve, such as with
bearing down during defe-cation or vomiting, attempts are made to prevent
further vagal stimulation. If the bradycardia is from a medication such as a beta-blocker,
the medication may be withheld. If the slow heart rate causes significant
hemodynamic changes, resulting in short-ness of breath, decreased level of
consciousness, angina, hypoten-sion, ST-segment changes, or premature
ventricular complexes, treatment is directed toward increasing the heart rate.
Atropine,
0.5 to 1.0 mg given rapidly as an intravenous (IV) bolus, is the medication of
choice in treating sinus bradycardia. It blocks vagal stimulation, thus
allowing a normal rate to occur. Rarely, catecholamines and emergency
transcutaneous pacing also may be implemented.
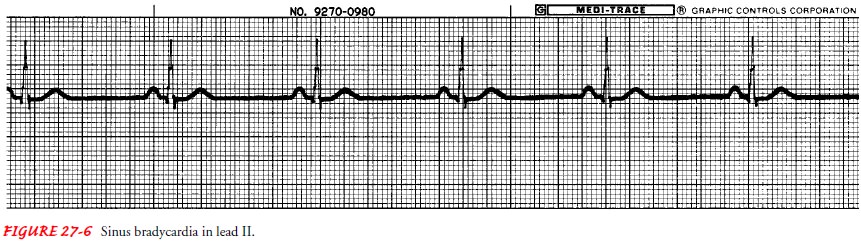
Sinus Tachycardia.
Sinus
tachycardia occurs when the sinus nodecreates an impulse at a
faster-than-normal rate. It may be caused by acute blood loss, anemia, shock,
hypervolemia, hypovolemia, congestive heart failure, pain, hypermetabolic
states, fever, exer-cise, anxiety, or sympathomimetic medications. The ECG
crite-ria for sinus tachycardia follow (Fig. 27-7):
Ventricular and atrial rate: Greater
than 100 in the adult
Ventricular and atrial rhythm: Regular
QRS shape and duration: Usually
normal, but may be regularlyabnormal
P wave: Normal and
consistent shape; always in front of theQRS, but may be buried in the preceding
T wave
PR interval: Consistent
interval between 0.12 and 0.20 seconds
P: QRS ratio: 1
1
All
aspects of sinus tachycardia are the same as those of nor-mal sinus rhythm,
except for the rate. As the heart rate increases, the diastolic filling time
decreases, possibly resulting in reduced cardiac output and subsequent symptoms
of syncope and low blood pressure. If the rapid rate persists and the heart
cannot compensate for the decreased ventricular filling, the patient may
develop acute pulmonary edema.
Treatment
of sinus tachycardia is usually directed at abolishing its cause. Calcium
channel blockers and beta-blockers (Table 27-1) may be used to reduce the heart
rate quickly.
Sinus Arrhythmia.
Sinus
arrhythmia occurs when the sinus nodecreates an impulse at an irregular rhythm;
the rate usually in-creases with inspiration and decreases with expiration.
Nonrespi-ratory causes include heart disease and valvular disease, but these
are rarely seen. The ECG criteria for sinus arrhythmia follow (Fig. 27-8):
Ventricular and atrial rate: 60
to 100 in the adult
Ventricular and atrial rhythm: Irregular
QRS shape and duration: Usually normal, but may be regularlyabnormal
P wave: Normal and
consistent shape; always in front of the QRS
PR interval: Consistent
interval between 0.12 and 0.20 seconds
P: QRS ratio: 1
1
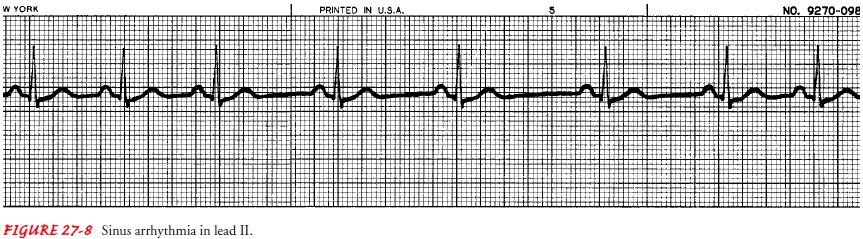
Sinus
arrhythmia does not cause any significant hemodynamic effect and usually is not
treated.
ATRIAL DYSRHYTHMIAS
Premature Atrial Complex.
A premature atrial complex (PAC) isa single ECG complex that
occurs when an electrical impulse starts in the atrium before the next normal
impulse of the sinus node. The PAC may be caused by caffeine, alcohol,
nicotine, stretched atrial myocardium (as in hypervolemia), anxiety,
hypokalemia (low potassium level), hypermetabolic states, or atrial ischemia,
injury, or infarction. PACs are often seen with sinus tachycardia. PACs have
the following characteristics (Fig. 27-9):
Ventricular and atrial rate: Depends
on the underlying rhythm(eg, sinus tachycardia)
Ventricular and atrial rhythm: Irregular
due to early P waves,creating a PP interval that is shorter than the others.
This is sometimes followed by a longer-than-normal PP inter-val, but one that
is less than twice the normal PP interval. This type of interval is called a
noncompensatory pause.
QRS shape and duration: The
QRS that follows the early P waveis usually normal, but it may be abnormal
(aberrantly con-ducted PAC). It may even be absent (blocked PAC).
P wave: An early
and different P wave may be seen or maybe hidden in the T wave; other P waves
in the strip are consistent.
PR interval: The
early P wave has a shorter-than-normal PRinterval, but still between 0.12 and
0.20 seconds.
P: QRS ratio: usually
1 1
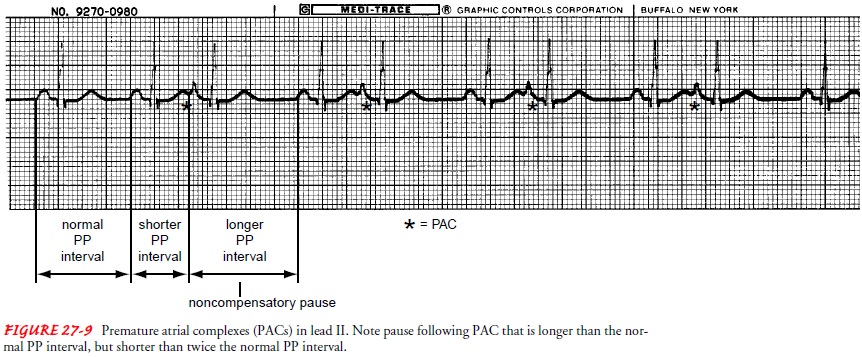
PACs
are common in normal hearts. The patient may say, “My heart skipped a beat.” A
pulse deficit (a difference between the apical and radial pulse rate) may
exist.
If
PACs are infrequent, no treatment is necessary. If they are frequent (more than
6 per minute), this may herald a worsening disease state or the onset of more
serious dysrhythmias, such as atrial fibrillation. Treatment is directed toward
the cause.
Atrial Flutter.
Atrial
flutter occurs in the atrium and creates im-pulses at an atrial rate between
250 and 400 times per minute. Because the atrial rate is faster than the AV
node can conduct, not all atrial impulses are conducted into the ventricle,
causing a ther-apeutic block at the AV node. This is an important feature of
this dysrhythmia. If all atrial impulses were conducted to the ventri-cle, the
ventricular rate would also be 250 to 400, which would result in ventricular
fibrillation, a life-threatening dysrhythmia. Causes are similar to that of
atrial fibrillation. Atrial flutter is characterized by the following (Fig. 27-10):
Ventricular and atrial rate: Atrial
rate ranges between 250 and400; ventricular rate usually ranges between 75 and
150.
Ventricular and atrial rhythm: The
atrial rhythm is regular; theventricular rhythm is usually regular but may be
irregular because of a change in the AV conduction.
QRS shape and duration: Usually
normal, but may be abnor-mal or may be absent
P wave: Saw-toothed
shape. These waves are referred to asF waves.
PR interval: Multiple
F waves may make it difficult to deter-mine the PR interval.
P:QRS ratio: 2
1, 3 1, or 4 1
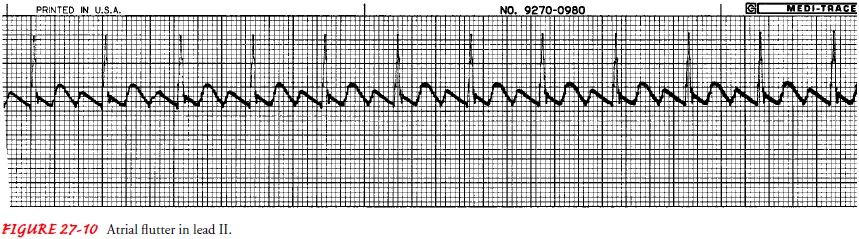
Atrial flutter can cause serious signs and symptoms, such as chest pain, shortness of breath, and low blood pressure. If the patient
is unstable, electrical cardioversion (discussed later) is usu-ally indicated.
If the patient is stable, diltiazem (eg, Cardizem), verapamil (eg, Calan,
Isoptin), beta-blockers, or digitalis may be administered intravenously to slow
the ventricular rate. These medications can slow conduction through the AV
node. Flecainide (Tambocor), ibutilide (Corvert), dofetilide (Tikosyn),
quini-dine (eg, Cardioquin, Quinaglute), disopyramide (Norpace), or amiodarone
(Cordarone, Pacerone) may be given to promote con-version to sinus rhythm (see
Table 27-1). If medication therapy is unsuccessful, electrical cardioversion is
often successful. Once conversion has occurred, quinidine, disopyramide,
flecainide, pro-pafenone (Rhythmol), amiodarone, or sotalol (Betapace) may be
given to maintain sinus rhythm (see Table 27-1).
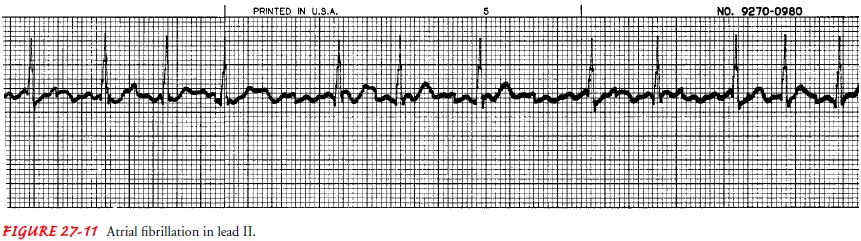
Atrial Fibrillation.
Atrial
fibrillation causes a rapid, disorganized,and uncoordinated twitching of atrial
musculature. It is the most common dysrhythmia that causes patients to seek
medical atten-tion. It may start and stop suddenly. Atrial fibrillation may
occur for a very short time (paroxysmal),
or it may be chronic. Atrial fibrillation is usually associated with advanced
age, valvular heart disease, coronary artery disease, hypertension,
cardiomyopathy, hyperthyroidism, pulmonary disease, acute moderate to heavy
in-gestion of alcohol (“holiday heart” syndrome), or the aftermath of open
heart surgery. Sometimes it occurs in people without any underlying
pathophysiology (termed lone atrial fibrillation). Atrial fibrillation is
characterized by the following (Fig. 27-11):
Ventricular and atrial rate: Atrial
rate is 300 to 600. Ventricu-lar rate is usually 120 to 200 in untreated atrial
fibrillation
Ventricular and atrial rhythm: Highly
irregular
QRS shape and duration: Usually
normal, but may be abnormal
P wave: No
discernible P waves; irregular undulating waves areseen and are referred to as
fibrillatory or f waves
PR interval: Cannot
be measured
P: QRS ratio: many
1
A
rapid ventricular response reduces the time for ventricular filling, resulting
in a smaller stroke volume. Because this rhythm causes the atria and ventricles
to contract at different times, the atrial kick (the last part of diastole and
ventricular filling, which accounts for 25% to 30% of the cardiac output) is
also lost. This leads to symptoms of irregular palpitations, fatigue, and
malaise. There is usually a pulse deficit, a numerical difference between
apical and radial pulse rates. The shorter time in diastole reduces the time
available for coronary artery perfusion, thereby increas-ing the risk for
myocardial ischemia. The erratic atrial contraction promotes the formation of a
thrombus within the atria, increas-ing the risk for an embolic event. There is
a two- to five-fold increase in the risk of stroke (brain attack).
Treatment of atrial fibrillation depends on its cause and dura-tion and the patient’s symptoms, age, and comorbidities. In many patients, atrial fibrillation converts to sinus rhythm within 24 hours and without treatment.
Both stable and unstable atrial fibrillation of
short duration are treated the same as stable and unstable atrial flutter.
Cardioversion may be indicated for atrial fibrillation that has been present
for less than 48 hours, a condition termed acute-onset atrial fibrillation.
Cardioversion of atrial fibrillation that has lasted longer than 48 hours
should be avoided unless the patient has received anticoagulants, due to the
high risk for embolization of atrial thrombi.
For
atrial fibrillation of acute onset, the medications quini-dine, ibutilide,
flecainide, dofetilide, propafenone, procainamide (Pronestyl), disopyramide, or
amiodarone (see Table 27-1) may be given to achieve conversion to sinus rhythm
(McNamara et al., 2001). Intravenous adenosine (Adenocard, Adenoscan) has also
been used for conversion, as well as to assist in the diagnosis. To prevent
recurrence and to maintain sinus rhythm, quinidine, diso-pyramide, flecainide,
propafenone, sotalol, or amiodarone may be prescribed. Calcium-channel blockers
[diltiazem (Cardizem, Dilacor, Tiazac) and verapamil (Calan, Isoptin, Verelan)]
and beta blockers (see Table 27-1) are effective in controlling the ventricular
rate in atrial fibrillation, especially during exercise (McNamara, et al.,
2001). Use of digoxin is recommended to con-trol the ventricular rate in those
patients with poor cardiac function (ejection fraction less than 40%) (Hauptman
& Kelly, 1999). In addition, warfarin is indicated if the patient is at
higher risk for a stroke (ie, is elderly or has hypertension, heart failure, or
a history of stroke). Aspirin may be substituted for warfarin for those with
contraindications to warfarin and those who are at lower risk of stroke. The
choice of antithrombotic medication can be guided by transesophageal
echocardiography. Pacemaker implantation or surgery is sometimes indicated for
patients who are unresponsive to medications.
JUNCTIONAL DYSRHYTHMIAS
Premature Junctional Complex. A premature junctional complexis an impulse that starts in the AV
nodal area before the next normal sinus impulse reaches the AV node. Premature
junctional complexes are less common than PACs. Causes of premature junctional
complex include digitalis toxicity, congestive heart fail-ure, and coronary
artery disease. The ECG criteria for premature junctional complex are the same
as for PACs, except for the P wave and the PR interval. The P wave may be
absent, may follow the QRS, or may occur before the QRS but with a PR interval
of less than 0.12 seconds. Premature junctional complexes rarely pro-duce
significant symptoms. Treatment for frequent premature junctional complexes is
the same as for frequent PACs.
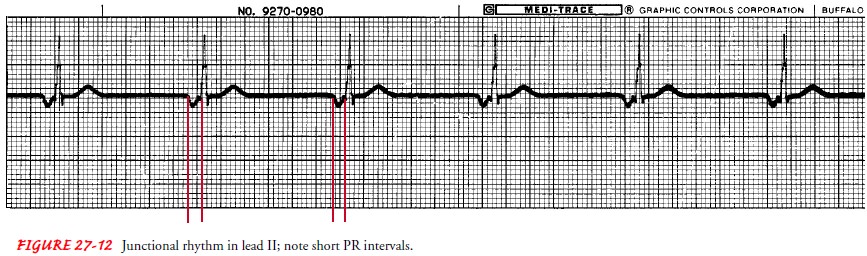
Junctional Rhythm.
Junctional
or idionodal rhythm occurs whenthe AV node, instead of the sinus node, becomes
the pacemaker of the heart. When the sinus node slows (eg, from increased vagal
tone) or when the impulse cannot be conducted through the AV node (eg, because
of complete heart block), the AV node auto-matically discharges an impulse. The
following are the ECG cri-teria for junctional rhythm not caused by complete
heart block (Fig. 27-12):
Ventricular and atrial rate: Ventricular
rate 40 to 60; atrial ratealso 40 to 60 if P waves are discernible
Ventricular and atrial rhythm: Regular
QRS shape and duration: Usually
normal, but may be abnormal
P wave: May be absent, after the QRS complex, or before theQRS; may be inverted, especially in lead II
PR interval: If
P wave is in front of the QRS, PR interval is lessthan 0.12 second.
P:QRS ratio: 1
1 or 0 1
Junctional
rhythm may produce signs and symptoms of re-duced cardiac output. If so, the
treatment is the same as for sinus bradycardia. Emergency pacing may be needed.
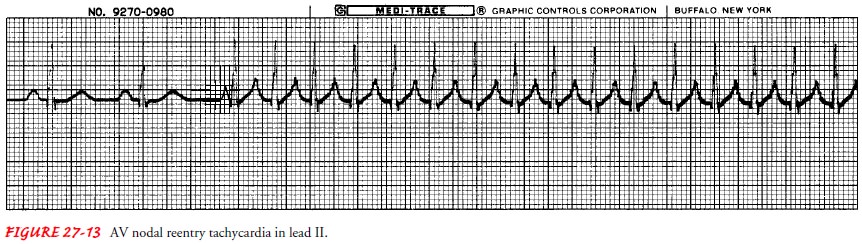
Atrioventricular Nodal Reentry Tachycardia.
AV nodal reentrytachycardia occurs when an impulse is conducted to
an area in the AV node that causes the impulse to be rerouted back into the
same area over and over again at a very fast rate. Each time the impulse is
conducted through this area, it is also conducted down into the ventricles,
causing a fast ventricular rate. AV nodal re-entry tachycardia that has an
abrupt onset and an abrupt cessa-tion with a QRS of normal duration had been
called paroxysmal atrial tachycardia (PAT). Factors associated with the
develop-ment of AV nodal reentry tachycardia include caffeine, nicotine,
hypoxemia, and stress. Underlying pathologies include coronary artery disease
and cardiomyopathy. The ECG criteria are as fol-lows (Fig. 27-13):
Ventricular and atrial rate: Atrial
rate usually ranges between150 to 250; ventricular rate usually ranges between
75 to 250 Ventricular and atrial rhythm: Regular;
sudden onset and ter-
mination
of the tachycardia
QRS shape and duration: Usually
normal, but may be abnormal
P wave: Usually
very difficult to discern
PR interval: If
P wave is in front of the QRS, PR interval is lessthan 0.12 seconds
P: QRS ratio: 1
1, 2 1
The
clinical symptoms vary with the rate and duration of the tachycardia and the
patient’s underlying condition. The tachycardia usually is of short duration,
resulting only in pal-pitations. A fast rate may also reduce cardiac output,
resulting in significant signs and symptoms such as restlessness, chest pain,
shortness of breath, pallor, hypotension, and loss of con-sciousness.
Treatment
is aimed at breaking the reentry of the impulse. Vagal maneuvers, such as
carotid sinus massage (Fig. 27-14), gag reflex, breath holding, and immersing
the face in ice water, increase parasympathetic stimulation, causing slower
conduc-tion through the AV node and blocking the reentry of the rerouted
impulse. Some patients have learned to use some of these methods to terminate
the episode on their own. Because of the risk of a cerebral embolic event,
carotid sinus massage is contraindicated in patients with carotid bruits. If
the vagal ma-neuvers are ineffective, the patient may then receive a bolus of
adenosine, verapamil, or diltiazem. Cardioversion is the treat-ment of choice
if the patient is unstable or does not respond to the medications.
If
P waves cannot be identified, the rhythm may be called supraventricular tachycardia (SVT), which indicates only thatit is
not ventricular tachycardia (VT).
SVT could be atrial fi-brillation, atrial flutter, or AV nodal reentry
tachycardia, among others. Vagal maneuvers and adenosine are used to slow
conduc-tion in the AV node to allow visualization of the P waves.
VENTRICULAR DYSRHYTHMIAS
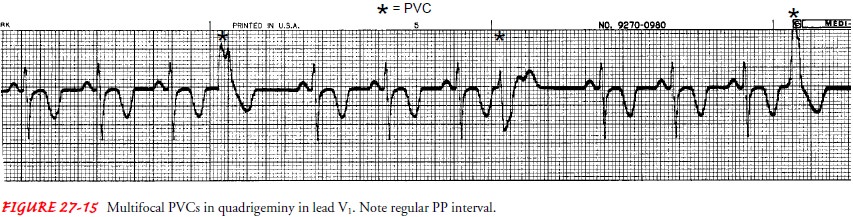
Premature Ventricular Complex.
Premature ventricular com-plex (PVC) is an impulse that starts in
a ventricle and is con-ducted through the ventricles before the next normal
sinus impulse. PVCs can occur in healthy people, especially with the use of
caffeine, nicotine, or alcohol. They are also caused by car-diac ischemia or
infarction, increased workload on the heart (eg, exercise, fever, hypervolemia,
heart failure, tachycardia), digitalis toxicity, hypoxia, acidosis, or
electrolyte imbalances, especially hypokalemia.
In
the absence of disease, PVCs are not serious. In the patient with an acute MI,
PVCs may indicate the need for more aggres-sive therapy. PVCs may indicate the
possibility of ensuing VT. However, PVCs that are (1) more frequent than 6 per
minute,multifocal or polymorphic (having different shapes), (3) occur two in a
row (pair), and (4) occur on the T wave (the vulnerable period of ventricular
depolarization) have not been found to be precursors of VT (Cardiac Arrhythmia
Suppression Trial Inves-tigators, 1989). These PVCs are no longer considered as
warning or complex PVCs.
In
a rhythm called bigeminy, every other complex is a PVC. Trigeminy is a rhythm
in which every third complex is a PVC, and quadrigeminy is a rhythm in which
every fourth complex is a PVC. PVCs have the following characteristics on the
ECG (Fig. 27-15):
Ventricular and atrial rate: Depends
on the underlying rhythm(eg, sinus rhythm)
Ventricular and atrial rhythm: Irregular
due to early QRS, cre-ating one RR interval that is shorter than the others. PP
in-terval may be regular, indicating that the PVC did not depolarize the sinus
node.
QRS shape and duration: Duration
is 0.12 seconds or longer;shape is bizarre and abnormal
P wave: Visibility
of P wave depends on the timing of thePVC; may be absent (hidden in the QRS or
T wave) or in front of the QRS. If the P wave follows the QRS, the shape of the
P wave may be different.
PR interval: If
the P wave is in front of the QRS, the PRinterval is less than 0.12 seconds.
P: QRS ratio: 0
1; 1 1
The
patient may feel nothing or may say that the heart “skipped a beat.” The effect
of a PVC depends on its timing in the cardiac cycle and how much blood was in
the ventricles when they contracted. Initial treatment is aimed at correcting
the cause, if possible. Lidocaine (Xylocaine) is the medication most com-monly
used for immediate, short-term therapy (see Table 27-1). Long-term
pharmacotherapy for only PVCs is not indicated.
Ventricular Tachycardia.
Ventricular tachycardia (VT) is de-fined as three or more PVCs in
a row, occurring at a rate exceed-ing 100 beats per minute. The causes are
similar to those for PVC. VT is usually associated with coronary artery disease
and may precede ventricular fibrillation. VT is an emergency because the
patient is usually (although not always) unresponsive and pulseless. VT has the
following characteristics (Fig. 27-16):
Ventricular and atrial rate: Ventricular
rate is 100 to 200 beatsper minute; atrial rate depends on the underlying
rhythm (eg, sinus rhythm)
Ventricular and atrial rhythm: Usually
regular; atrial rhythmmay also be regular.
QRS shape and duration: Duration
is 0.12 seconds or more;bizarre, abnormal shape
P wave: Very
difficult to detect, so atrial rate and rhythm maybe indeterminable
PR interval: Very
irregular, if P waves seen.
P:QRS ratio: Difficult
to determine, but if P waves are appar-ent, there are usually more QRS complexes
than P waves.
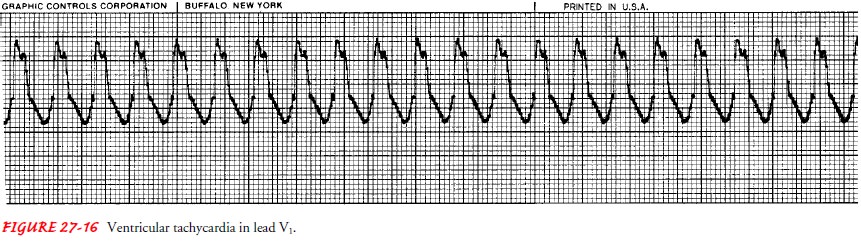
The
patient’s tolerance or lack of tolerance for this rapid rhythm depends on the
ventricular rate and underlying disease. If the patient is stable, continuing
the assessment, especially ob-taining a 12-lead ECG, may be the only action
necessary. Cardio-version may be the treatment of choice, especially if the
patient is unstable. Several factors determine the initial medication used for
treatment, including the following: identifying the rhythm as monomorphic
(having a consistent QRS shape and rate) or poly-morphic (having varying QRS
shapes and rates); determining the existence of a prolonged QT interval before
the initiation of VT; and ascertaining the patient’s heart function (normal or
decreased). VT in a patient who is unconscious and without a pulse is treated
in the same manner as ventricular fibrillation: immediate defi-brillation is the action of choice.
Ventricular Fibrillation.
Ventricular fibrillation is a rapid but dis-organized ventricular
rhythm that causes ineffective quivering of the ventricles. There is no atrial
activity seen on the ECG. Causes of ventricular fibrillation are the same as
for VT; it may also re-sult from untreated or unsuccessfully treated VT. Other
causes include electrical shock and Brugada syndrome, in which the pa-tient
(frequently of Asian descent) has a structurally normal heart, few or no risk
factors for coronary artery disease, and a family his-tory of sudden cardiac
death. Ventricular fibrillation has the fol-lowing characteristics (Fig. 27-17):
Ventricular rate: Greater
than 300 per minute
Ventricular rhythm: Extremely
irregular, without specificpattern
QRS shape and duration: Irregular,
undulating waves withoutrecognizable QRS complexes
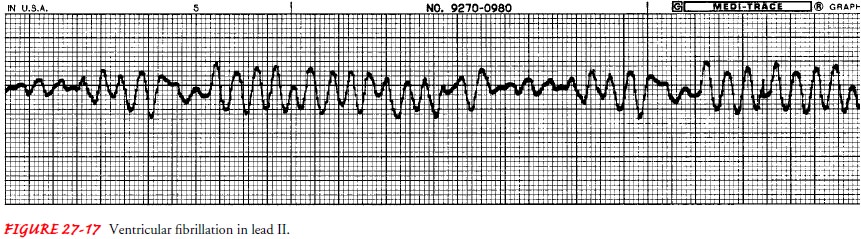
This dysrhythmia is always characterized by the absence of an audible heartbeat, a palpable pulse, and respirations. Because there is no coordinated cardiac activity, cardiac arrest and death are im-minent if ventricular fibrillation is not corrected. Treatment of choice is immediate defibrillation and activation of emergency services. The importance of defibrillation is evident in one of the recent changes in basic life support (American Heart Association, 2000): placing a call for emergency assistance and calling for a de-fibrillator takes precedence over initiating cardiopulmonary re-suscitation in the adult victim. Also, application of an automatic external defibrillator (AED) is included in basic life support classes. After defibrillation, eradicating causes and administering vaso-active and antiarrhythmic medications alternating with defibrillation are treatments used to try to convert the rhythm to normal sinus rhythm.
Idioventricular Rhythm.
Idioventricular rhythm, also called ven-tricular escape rhythm,
occurs when the impulse starts in the con-duction system below the AV node.
When the sinus node fails to create an impulse (eg, from increased vagal tone),
or when the im-pulse is created but cannot be conducted through the AV node
(eg, due to complete AV block), the Purkinje fibers automatically discharge an
impulse. The following are the ECG criteria when idioventricular rhythm is not
caused by AV block (Fig. 27-18):
Ventricular rate: Ranges
between 20 and 40; if the rate exceeds40, the rhythm is known as accelerated
idioventricular rhythm (AIVR).
Ventricular rhythm: Regular
QRS shape and duration: Bizarre,
abnormal shape; duration is0.12 seconds or more
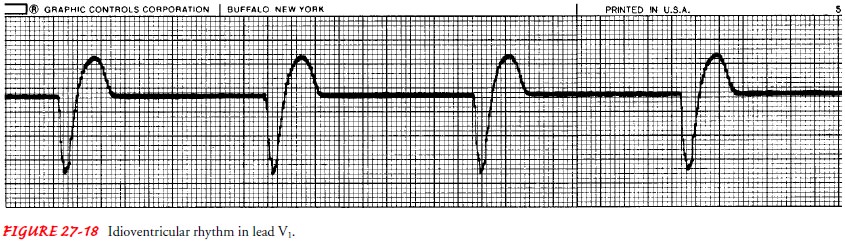
Idioventricular
rhythm commonly causes the patient to lose consciousness and experience other
signs and symptoms of re-duced cardiac output. In such cases, the treatment is
the same as for pulseless electrical activity if the patient is in cardiac
arrest or for bradycardia if the patient is not in cardiac arrest.
Interven-tions may include identifying the underlying cause, administer-ing
intravenous atropine and vasopressor medications, and initiating emergency
transcutaneous pacing. In some cases, idio-ventricular rhythm may cause no
symptoms of reduced cardiac output. However, bed rest is prescribed so as not
to increase the cardiac workload.
Ventricular Asystole.
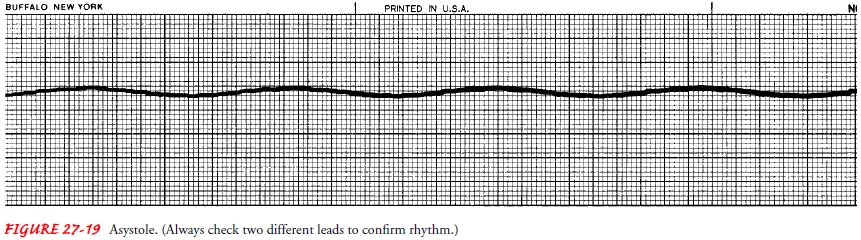
Commonly
called flatline, ventricular asys-tole (Fig. 27-19) is characterized by absent
QRS complexes, al-though P waves may be apparent for a short duration in two different
leads. There is no heartbeat, no palpable pulse, and no respiration. Without
immediate treatment, ventricular asystole is fatal. Cardiopulmonary
resuscitation and emergency services are necessary to keep the patient alive.
The guidelines for advanced cardiac life support (American Heart Association,
2000) state that the key to successful treatment is rapid assessment to
identify a possible cause, which may be hypoxia, acidosis, severe electro-lyte
imbalance, drug overdose, or hypothermia. Intubation and establishment of
intravenous access are the first recommended ac-tions. Transcutaneous pacing
may be attempted. A bolus of intra-venous epinephrine should be administered
and repeated at 3- to 5-minute intervals, followed by 1-mg boluses of atropine
at 3- to 5-minute intervals. Because of the poor prognosis associated with
asystole, if the patient does not respond to these actions and others aimed at
correcting underlying causes, resuscitation efforts are usually ended (“the
code is called”) unless special circumstances (eg, hypothermia) exist.
CONDUCTION ABNORMALITIES
When
assessing the rhythm strip, the nurse takes care first to identify the
underlying rhythm (eg, sinus rhythm, sinus arrhyth-mia). Then the PR interval
is assessed for the possibility of an AV block. AV blocks occur when the
conduction of the impulse through the AV nodal area is decreased or stopped.
These blocks can be caused by medications (eg, digitalis, calcium channel
blockers, beta-blockers), myocardial ischemia and infarction, valvular disorders,
or myocarditis. If the AV block is caused by increased vagal tone (eg,
suctioning, pressure above the eyes or on large vessels, anal stimulation), it
is commonly accompanied by sinus bradycardia.
The clinical signs and symptoms of a heart block vary with the resulting ventricular rate and the severity of any underlying disease processes.
Whereas first-degree AV block rarely causes any hemodynamic effect,
the other blocks may result in decreased heart rate, causing a decrease in
perfusion to vital organs, such as the brain, heart, kidneys, lungs, and skin.
A patient with third-degree AV block caused by digitalis toxicity may be
stable; another pa-tient with the same rhythm caused by acute MI may be
unstable. Health care providers must always keep in mind the need to treat the
patient, not the rhythm. The treatment is based on the hemo-dynamic effect of
the rhythm.
First-Degree Atrioventricular Block.
First-degree heart block oc-curs when all the atrial impulses are
conducted through the AV node into the ventricles at a rate slower than normal.
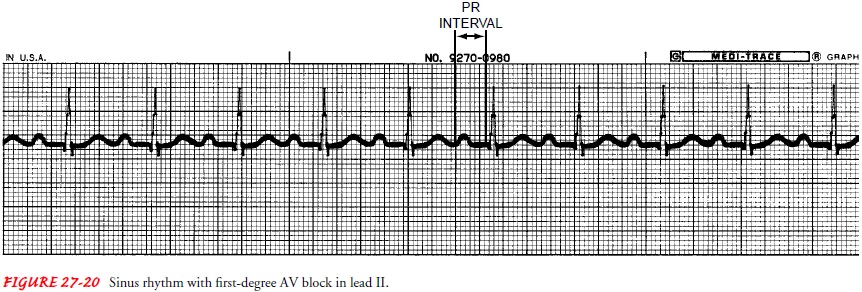
This con-duction disorder has the following characteristics (Fig. 27-20):
Ventricular and atrial rate: Depends
on the underlying rhythm
Ventricular and atrial rhythm: Depends
on the underlyingrhythm
QRS shape and duration: Usually
normal, but may be abnormal
P wave: In front
of the QRS complex; shows sinus rhythm,regular shape
PR interval: Greater
than 0.20 seconds; PR interval measure-ment is constant.
P: QRS ratio: 1
1
Second-Degree Atrioventricular Block, Type I.
Second-degree,type I heart block occurs when all but one of the
atrial impulses are conducted through the AV node into the ventricles. Each
atrial impulse takes a longer time for conduction than the one be-fore, until
one impulse is fully blocked. Because the AV node is not
depolarized by the blocked atrial impulse, the AV node has time to fully
repolarize, so that the next atrial impulse can be con-ducted within the
shortest amount of time. Second-degree AV block, type I has the following
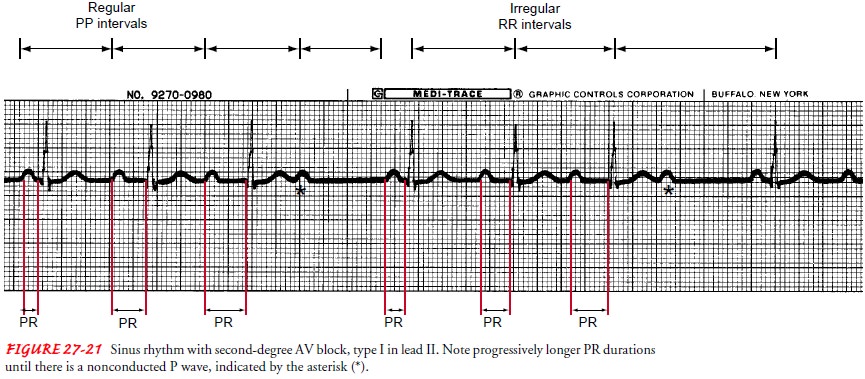
characteristics (Fig. 27-21):
Ventricular and atrial rate: Depends
on the underlying rhythm
Ventricular and atrial rhythm: The
PP interval is regular if thepatient has an underlying normal sinus rhythm; the
RR in-terval characteristically reflects a pattern of change. Start-ing from
the RR that is the longest, the RR interval gradually shortens until there is
another long RR interval.
QRS shape and duration: Usually
normal, but may be abnormal
P wave: In front
of the QRS complex; shape depends on un-derlying rhythm
PR interval: PR
interval becomes longer with each succeedingECG complex until there is a P wave
not followed by a QRS. The changes in the PR interval are repeated between each
“dropped” QRS, creating a pattern in the irregular PR interval measurements.
P:QRS ratio: 3
2, 4 3, 5 4, and so forth
Second-Degree Atrioventricular Block, Type II.
Second-degree,type II heart block occurs when
only some of the atrial impulses are conducted through the AV node into the
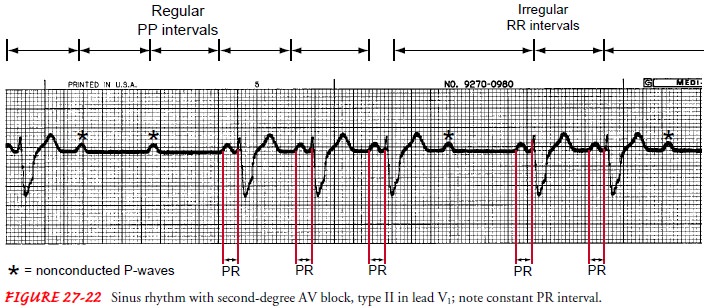
ventricles. Second-degree AV block, type II has the following characteristics
(Fig. 27-22):
Ventricular and atrial rate: Depends
on the underlying rhythm
Ventricular and atrial rhythm: The PP interval is regular if thepatient has an underlying normal sinus rhythm. The RR
interval
is usually regular but may be irregular, depending on the P QRS ratio.
QRS shape and duration: Usually
abnormal, but may be normal
P wave: In front
of the QRS complex; shape depends onunderlying rhythm.
PR interval: PR
interval is constant for those P waves justbefore QRS complexes.
P:QRS ratio: 2
1, 3 1, 4 1, 5 1, and so forth
Third-Degree Atrioventricular Block.
Third-degree heart blockoccurs when no atrial impulse is conducted
through the AV node into the ventricles. In third-degree heart block, two
impulses stimulate the heart: one stimulates the ventricles (eg, junctional or
ventricular escape rhythm), represented by the QRS complex, and one stimulates
the atria (eg, sinus rhythm, atrial fibrillation), represented by the P wave. P
waves may be seen, but the atrial electrical activity is not conducted down
into the ventricles to cause the QRS complex, the ventricular electrical
activity. This is called AV dissociation. Complete block (third-degree AV
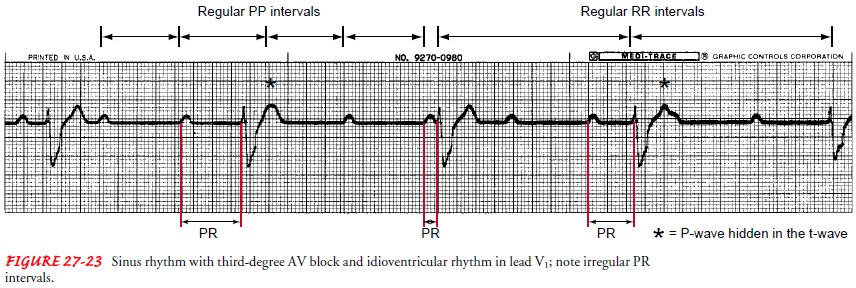
block) has the following characteristics (Fig. 27-23):
Ventricular and atrial rate: Depends
on the escape and under-lying atrial rhythm
Ventricular and atrial rhythm: The
PP interval is regular andthe RR interval is regular; however, the PP interval
is not equal to the RR interval.
QRS shape and duration: Depends
on the escape rhythm; injunctional escape, QRS shape and duration are usually
nor-mal, and in ventricular escape, QRS shape and duration are usually
abnormal.
P wave: Depends on
underlying rhythm
PR interval: Very
irregular
PQRS ratio: More
P waves than QRS complexes
Based
on the cause of the AV block and the stability of the pa-tient, treatment is
directed toward increasing the heart rate to maintain a normal cardiac output.
If the patient is stable and has no symptoms, no treatment is indicated other
than decreasing or eradicating the cause (eg, withholding the medication or
treat-ment). If the patient is short of breath, complains of chest pain or
lightheadedness, or has low blood pressure, an intravenous bolus of atropine is
the initial treatment of choice. If the patient does not respond to atropine or
has an acute MI, transcutaneous pacing should be started. A permanent pacemaker
may be neces-sary if the block persists.
Related Topics