Chapter: Medical Surgical Nursing: Management of Patients With Dysrhythmias and Conduction Problems
Pacemaker Therapy - Adjunctive Modalities and Management
PACEMAKER THERAPY
A
pacemaker is an electronic device that provides electrical stimuli to the heart
muscle. Pacemakers are usually used when a patient has a slower-than-normal
impulse formation or a conduction dis-turbance that causes symptoms. They may
also be used to control some tachydysrhythmias that do not respond to
medication ther-apy. Biventricular (both ventricles) pacing may be used to
treat ad-vanced heart failure that does not respond to medication therapy.
Pacemakers
can be permanent or temporary. Permanent pace-makers are used most commonly for
irreversible complete heart block. Temporary pacemakers are used (eg, after MI,
after open heart surgery) to support patients until they improve or receive a
permanent pacemaker.
Pacemaker Design and Types
Pacemakers
consist of two components: an electronic pulse gen-erator and pacemaker
electrodes, which are located on leads or wires. The generator contains the
circuitry and batteries that gen-erate the rate (measured in beats per minute)
and the strength (measured in milliamperes [mA]) of the electrical stimulus
deliv-ered to the heart. The pacemaker electrodes convey the heart’s
elec-trical activity through a lead to the generator; the generator’s
electrical response to the information received is then transmit-ted to the
heart.
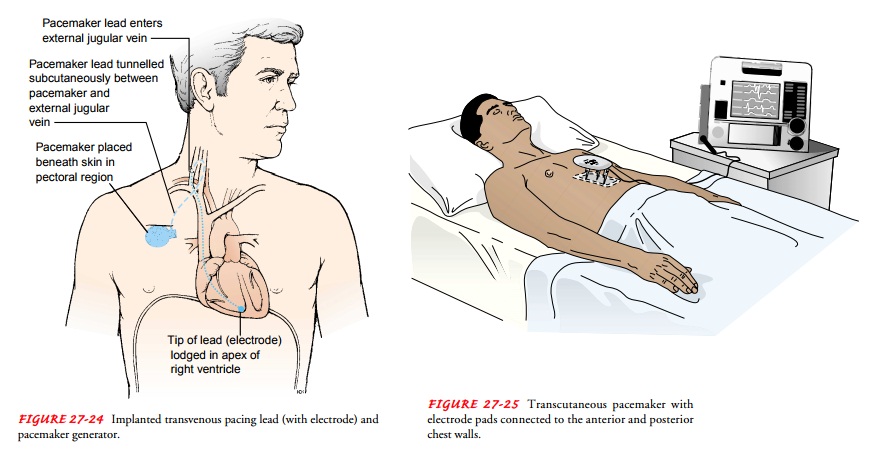
Leads
can be threaded through a major vein into the right ven-tricle (endocardial
leads), or they can be lightly sutured onto the outside of the heart and
brought through the chest wall during open heart surgery (epicardial wires).
The epicardial wires are al-ways temporary and are removed by a gentle tug
within a few days after surgery. The endocardial leads may be temporarily
placed with catheters through the femoral, antecubital, brachial, or jugu-lar
vein (transvenous wires), usually guided by fluoroscopy. The endocardial and
epicardial wires are connected to a temporary generator, which is about the
size of a small paperback book. The energy source for a temporary generator is
a common household battery; monitoring for pacemaker malfunctioning and battery
failure is a nursing responsibility. This type of pacemaker therapy necessitates
hospitalization of the patient.
The
endocardial leads also may be placed permanently, usu-ally through the external
jugular vein, and connected to a per-manent generator, which is usually
implanted underneath the skin in a subcutaneous pocket in the pectoral region
or below the clavicle (Fig. 27-24). Sometimes an abdominal site is selected.
This procedure is usually performed in a cardiac catheterization laboratory
with the patient receiving a local anesthetic. Perma-nent pacemaker generators
are insulated to protect against body moisture and warmth. There are several
different energy sources for permanent generators: mercury-zinc batteries
(which last 3 to 4 years), lithium cell units (up to 10 years), and
nuclear-powered sources such as plutonium 238 (up to 20 years). Some of the
bat-teries are rechargeable. If the battery is not rechargeable and fail-ure is
impending, the old generator is removed and the new one is connected to the
existing leads and reimplanted in the already existing subcutaneous pocket.
This procedure is usually performed with the patient receiving a local
anesthetic. Hospitalization of the patient is needed for implantation or
battery replacement.
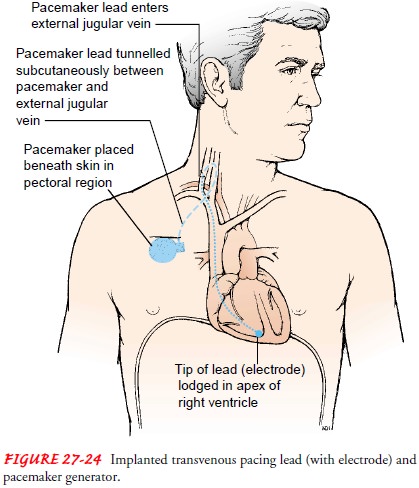
If a patient suddenly develops a bradycardia, emergency pac-ing may be started with transcutaneous pacing, which most de-fibrillators are now equipped to perform. AEDs are not able to do transcutaneous pacing (see later discussion). Large pacing ECG electrodes (sometimes the same conductive pads that are used for cardioversion and defibrillation) are placed on the patient’s chest and back.
The electrodes
are connected to the defibrillator, which is the temporary pacemaker generator
(Fig. 27-25). Because the impulse must travel through the patient’s skin and
tissue before reaching the heart, transcutaneous pacing can cause significant
dis-comfort and is intended to be used only in emergencies. This type of pacing
necessitates hospitalization. If the patient is alert, the use of sedation and
analgesia should be discussed with the physician.
Pacemaker Generator Functions
Because
of the sophistication and wide use of pacemakers, a uni-versal code has been
adopted to provide a means of safe commu-nication about their function. The
coding is referred to as the NASPE-BPEG code because it is sanctioned by the
North Amer-ican Society of Pacing and Electrophysiology and the British Pac-ing
and Electrophysiology Group. The complete code consists of five letters, but
only the first three are commonly used.
The
first letter of the code identifies the chamber or chambers being paced—that
is, the chamber containing a pacing electrode. The letter characters for this
code are A (atrium), V (ventricle), or D (dual, meaning both A and V).
The
second letter describes the chamber or chambers being sensed by the pacemaker
generator. Information from the elec-trode within the chamber is sent to the
generator for interpreta-tion and action by the generator. The possible letter
characters are A (atrium), V (ventricle), D (dual), and O (indicating that the
sensing function is turned off).
The third letter of the code describes the type of response by the pacemaker to what is sensed. The possible letter characters used to describe this response are I (inhibited), T (triggered), D (dual, inhibited and triggered), and O (none). Inhibited response means that the response of the pacemaker is controlled by the ac-tivity of the patient’s heart; that is, the pacemaker will not function when the patient’s heart beats but will pace if no beat is sensed. In contrast, triggered response means that the pacemaker will provide a response (pace the heart) when it senses intrinsic heart activity.
The
fourth and fifth letters are used only with permanent pace-maker generators.
The fourth letter of the code is related to a per-manent generator’s ability to
be programmed or reset. The possible letters are O (none), P (simple
programmability), M (multi-programmability; ability to change at least three
factors, such as the rate at which pacing is initiated, the rate of pacing, and
the amount of energy delivered), C (communicative or telemetry ability;
information about the generator may be obtained [read or interrogated] with a
hand-held device placed above the chest), and R (rate responsive capabilities;
the ability of the pacemaker to change the rate from moment to moment based on
parameters such as physical activity, acid-base changes, temperature, rate and
depth of respirations, and oxygen saturation). A pacemaker with rate responsive
ability will be capable of improving cardiac output during times of increased
cardiac demand, such as with exercise.
The
fifth letter of the code indicates that the permanent gen-erator has
antitachycardia and/or defibrillation capability. The possible letters are P
(antitachycardia pacing), S (shock; defibrilla-tion), D (dual—antitachycardia
pacing and shock), and O (none). Antitachycardia pacing is used to terminate
tachycardias caused by a conduction disturbance called reentry, which is
repetitive restimulation of the heart by the same impulse. An impulse or series
of impulses is delivered to the heart by the pacemaker at a fast rate to
collide with and stop the heart’s reentry conduction impulses, and therefore to
stop the tachycardia.
An
example of a NASPE-BPEG code is DVI:
D:Both
the atrium and the ventricle have a pacing electrode in place.
V:The
pacemaker is sensing the activity of the ventricle only.
I:The
pacemaker’s stimulating effect is inhibited by ventric-ular activity—in other
words, it does not create an impulse when the patient’s ventricle is active.
The pacemaker paces the atrium and then the ventricle when no ventricular
ac-tivity is sensed for a period of time (the time is individually programmed
into the pacemaker for each patient).
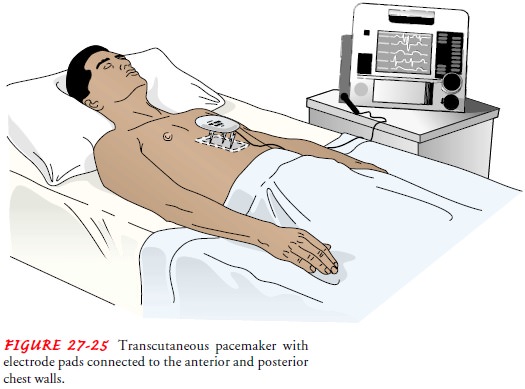
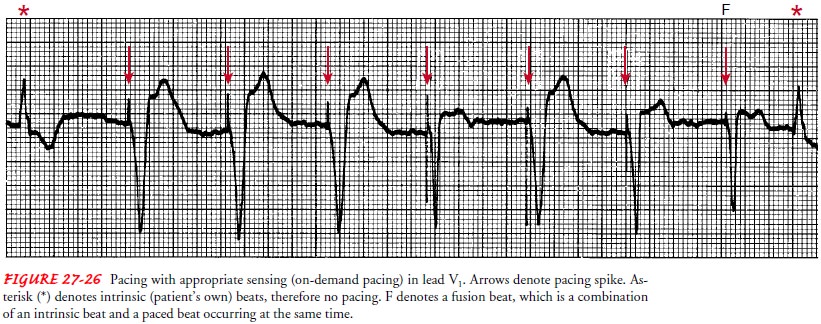
The
type of generator and its selected settings depend on the patient’s
dysrhythmia, underlying cardiac function, and age. A straight vertical line
usually can be seen on the ECG when pac-ing is initiated. The line that
represents pacing is called a pacemaker spike. The appropriate ECG complex
should immediately follow the pacing spike; therefore, a P wave should follow
an atrial pacing spike and a QRS complex should follow a ventricular pac-ing
spike. Because the impulse starts in a different place than the patient’s
normal rhythm, the QRS complex or P wave that re-sponds to pacing looks
different from the patient’s normal ECG complex. Capture is a term used to denote that the appropriate complex
followed the pacing spike.
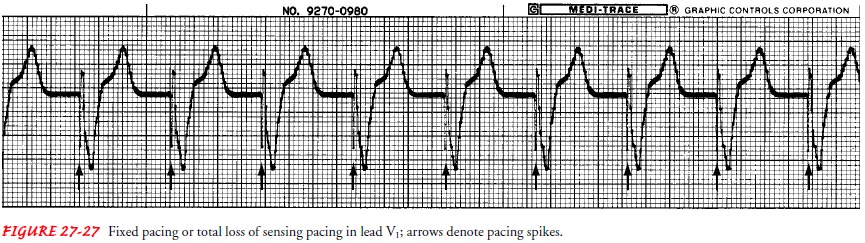
Pacemakers
are generally set to sense and respond to intrinsic activity, which is called
on-demand pacing (Fig. 27-26). If the pacemaker is set to pace but not to
sense, it is called a fixed or asynchronous pacemaker (Fig. 27-27); this is
written in code as AOO or VOO. The pacemaker will pace at a constant rate,
inde-pendent of the patient’s intrinsic rhythm. Because AOO pacing stimulates
only the atrium, it may be used in a patient who has undergone open heart
surgery and develops sinus bradycardia. AOO pacing ensures synchrony between
atrial stimulation and ventricular stimulation (and therefore contraction), as
long as the patient has no conduction disturbances in the AV node. VOO is rare
because of the risk that the pacemaker may deliver an impulse during the vulnerable
repolarization phase, leading to VT.
Complications of Pacemaker Use
Complications
associated with pacemakers relate to their pres-ence within the body, and
improper functioning. The following complications may arise from a pacemaker:
·
Local infection at the entry site of
the leads for temporary pacing, or at the subcutaneous site for permanent
generator placement
·
Bleeding and hematoma at the lead
entry sites for tem-porary pacing, or at the subcutaneous site for permanent
generator placement
·
Hemothorax from puncture of the
subclavian vein or inter-nal mammary artery
·
Ventricular ectopy and tachycardia
from irritation of the ventricular wall by the endocardial electrode
·
Movement or dislocation of the lead
placed transvenously (perforation of the myocardium)
·
Phrenic nerve, diaphragmatic
(hiccuping may be a sign of this), or skeletal muscle stimulation if the lead
is dislocated or if the delivered energy (mA) is set high
·
Rarely, cardiac tamponade from
bleeding resulting from re-moval of epicardial wires used for temporary pacing
In
the initial hours after a temporary or permanent pacemaker is inserted, the
most common complication is dislodgment of the pacing electrode. Minimizing
patient activity can help to prevent this complication. If a temporary
electrode is in place, the ex-tremity through which the catheter has been
advanced is immo-bilized. With a permanent pacemaker, the patient is instructed
initially to restrict activity on the side of the implantation.
The
ECG is monitored very carefully to detect pacemaker mal-function. Improper
pacemaker function, which can arise from failure in one or more components of
the pacing system, is out-lined in Table 27-2. The following data should be
noted on the patient’s record: model of pacemaker, type of generator, date and
time of insertion, location of pulse generator, stimulation thresh-old, pacer
settings (eg, rate, energy output [mA], and duration between atrial and
ventricular impulses [AV delay]). This infor-mation is important for
identifying normal pacemaker function and diagnosing pacemaker malfunction.
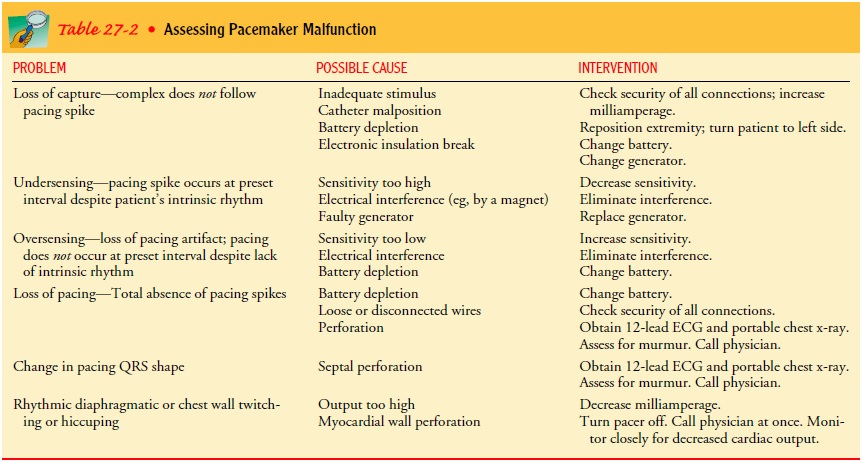
A
patient experiencing pacemaker malfunction may develop signs and symptoms of
decreased cardiac output. The degree to which these symptoms become apparent
depends on the severity of the malfunction, the patient’s level of dependency
on the pace-maker, and the patient’s underlying condition. Pacemaker
mal-function is diagnosed by analyzing the ECG. Manipulating the electrodes,
changing the generator’s settings, or replacing the pace-maker generator or
leads (or both) may be necessary.
Inhibition of permanent pacemakers
can occur with exposure to strong electromagnetic fields (electromagnetic
interference). However, recent pacemaker technology allows patients to safely
use most household electronic appliances and devices (eg, microwave ovens,
electric tools) as long as they are not held close to the pace-maker generator.
Gas-powered engines should be turned off before working on them. Objects that
contain magnets (eg, the earpiece of a standard phone; large stereo
speakers; magnet therapy prod-ucts such as mattresses, jewelry, and wraps)
should not be near the generator for longer than a few seconds. Patients are
advised to use digital cellular phones on the side opposite the pacemaker
gen-erator. Large electromagnetic fields, such as those produced by magnetic
resonance imaging (MRI), radio and TV transmitter tow-ers and lines,
transmission power lines (these are different from the distribution lines that
bring electricity into a home), and electrical substations may cause
electromagnetic interference. Patients should be cautioned to avoid such
situations or to simply move farther away from the area if they experience
dizziness or a feeling of rapid or irregular heartbeats (palpitations). Welding
and use of a chain saw should be avoided. If such tools are used, precautionary
steps such as limiting the welding current to a 60- to 130-ampere range or
using electric rather than gasoline-powered chain saws are advised.
The metal of the pacemaker generator may trigger some store and airport security alarms, but these alarm systems will not inter-fere with the pacemaker function. However, the handheld screen-ing devices used in airports may interfere with the pacemaker. Patients should be advised to request a hand search instead of the handheld screening device. Patients also should be instructed to wear or carry medical identification to alert personnel to the pres-ence of the pacemaker.
Pacemaker Surveillance
Pacemaker
clinics have been established to monitor patients and to test pulse generators
for impending pacemaker battery failure. Several other factors, such as lead
fracture, muscle inhibition, and insulation disruption, are assessed depending
on the type of pace-maker and the equipment available. If indicated, the
pacemaker is turned off for a few seconds, using a magnet or a programmer,
while the ECG is recorded to assess the patient’s underlying car-diac rhythm.
Another
follow-up method is transtelephonic transmission of the generator’s pulse rate.
Special equipment is used to transmit information about the patient’s pacemaker
over the telephone to a receiving system at a pacemaker clinic. The information
is con-verted into tones, which equipment at the clinic converts to an
electronic signal and records on an ECG strip. The pacemaker rate and other
data concerning pacemaker function are obtained and evaluated by a
cardiologist. This simplifies the diagnosis of a failing generator, reassures
the patient, and improves manage-ment when the patient is physically remote
from pacemaker testing facilities.
Related Topics