Chapter: Medical Surgical Nursing: Management of Patients With Dysrhythmias and Conduction Problems
Nursing Process: The Patient With a Pacemaker
NURSING PROCESS: THE PATIENT WITH A PACEMAKER
Assessment
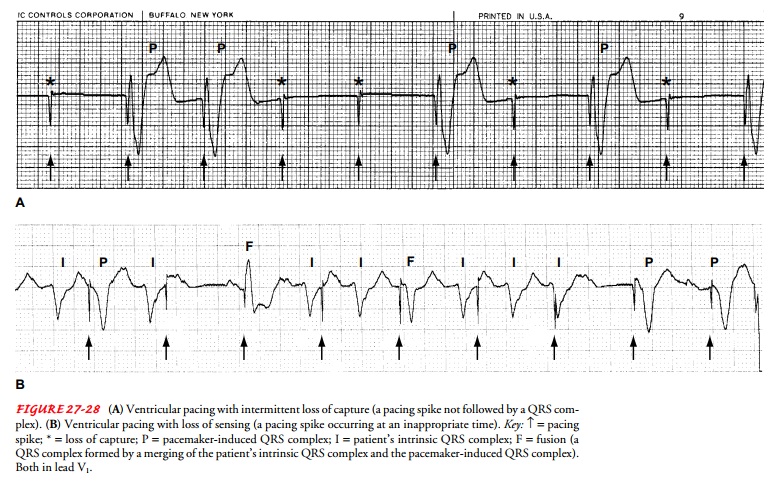
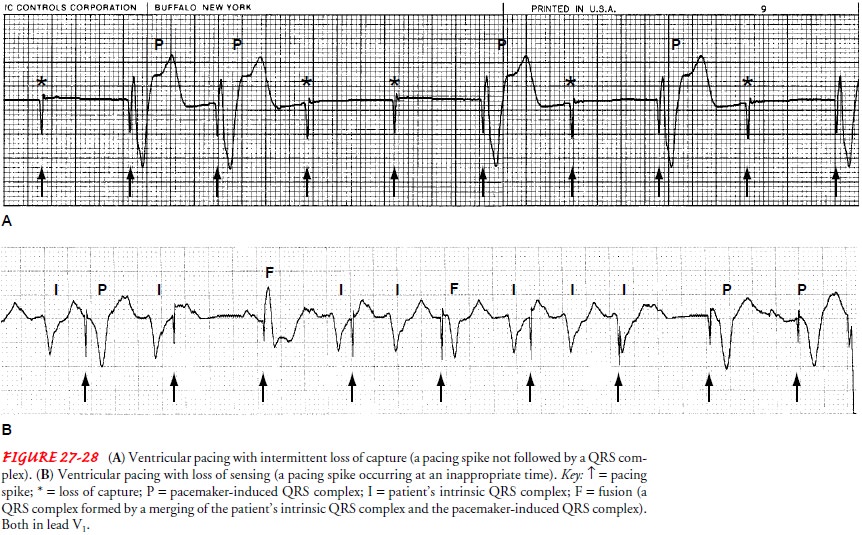
After
a temporary or a permanent pacemaker is inserted, the pa-tient’s heart rate and
rhythm are monitored by ECG. The pace-maker’s settings are noted and compared
with the ECG recordings to assess pacemaker function. Pacemaker malfunction is
detected by examining the pacemaker spike and its relationship to the surrounding
ECG complexes (Fig. 27-28). In addition, cardiac output and hemodynamic
stability are assessed to identify the pa-tient’s response to pacing and the
adequacy of pacing. The appearance or increasing frequency of dysrhythmia is
observed and reported to the physician.
The
incision site where the pulse generator was implanted (or the entry site for
the pacing electrode, if the pacemaker is a tempo-rary transvenous pacemaker)
is observed for bleeding, hematoma formation, or infection, which may be evidenced
by swelling, un-usual tenderness, unusual drainage, and increased heat. The
patient may complain of continuous throbbing or pain. These symptoms are
reported to the physician.
The
patient with a temporary pacemaker is also assessed for electrical interference
and the development of microshock. The nurse observes for potential sources of
electrical hazards. All elec-trical equipment used in the vicinity of the
patient should be grounded. Improperly grounded equipment can generate leakage
of current capable of producing ventricular fibrillation. Exposed wires must be
carefully covered with nonconductive material to prevent accidental ventricular
fibrillation from stray currents. The nurse, working with a biomedical engineer
or electrician, should make certain that the patient is in an electrically safe
environment.
Patients,
especially those receiving a permanent pacemaker, should be assessed for
anxiety. In addition, for those receiving permanent pacemakers, the level of
knowledge and learning needs of the patient and the family and the history of
adherence to the therapeutic regimen should be identified.
Diagnosis
NURSING DIAGNOSES
Based
on assessment data, major nursing diagnoses of the patient may include the
following:
·
Risk for infection related to
pacemaker lead or generator in-sertion
·
Risk for ineffective coping
· Deficient knowledge regarding self-care program
COLLABORATIVE PROBLEMS/ POTENTIAL COMPLICATIONS
Based
on the assessment findings, potential complications that may develop include
decreased cardiac output related to pace-maker malfunction.
Planning and Goals
The
major goals for the patient may include absence of infection, adherence to a
self-care program, effective coping, and mainte-nance of pacemaker function.
Nursing Interventions
PREVENTING INFECTION
The
nurse changes the dressing regularly and inspects the insertion site for
redness, swelling, soreness, or any unusual drainage. An in-crease in
temperature should be reported to the physician. Changes in wound appearance
are also reported to the physician.
PROMOTING EFFECTIVE COPING
The
patient treated with a pacemaker experiences not only lifestyle and physical
changes but also emotional changes. At different times during the healing
process, the patient may feel angry, depressed, fearful, anxious, or a
combination of these emotions. Although each patient uses individual coping
strategies (eg, humor, prayer, communication with a significant other) to
manage emotional dis-tress, some strategies may work better than others. Signs
that may indicate ineffective coping include social isolation, increased or
prolonged irritability or depression, and difficulty in relationships.
To
promote effective coping strategies, the nurse must recog-nize the patient’s
emotional state and assist the patient to explore his or her feelings. The
nurse may help the patient to identify perceived changes (eg, loss of ability
to participate in contact sports), the emotional response to the change (eg,
anger), and how the pa-tient responded to that emotion (eg, quickly became
angry when talking with spouse). The nurse reassures the patient that the
re-sponses are normal, then assists the patient to identify realistic goals
(eg, develop interest in another activity) and to develop a plan to attain
those goals. The nurse may also teach the patient easy-to-use stress reduction
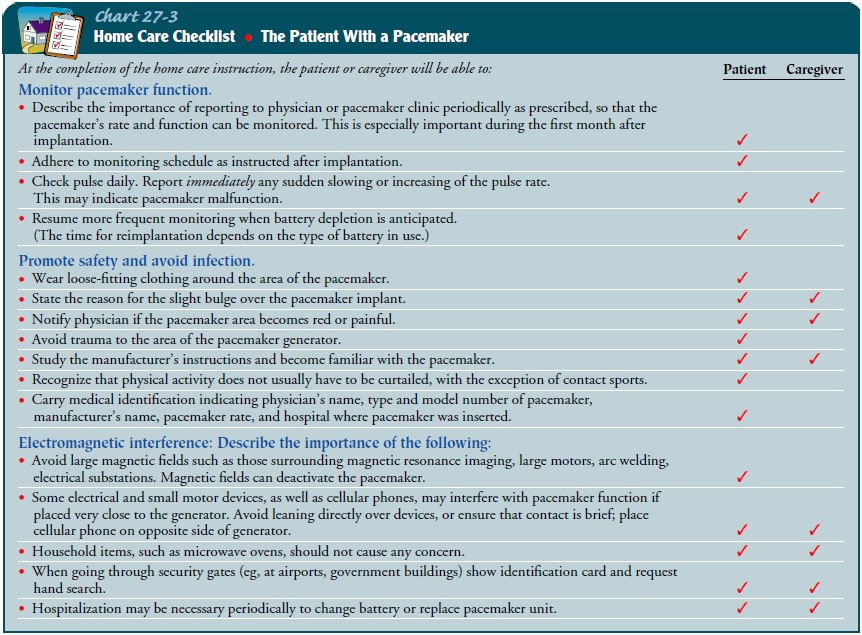
techniques (eg, deep-breathing exer-cises) to facilitate coping. Education
(Chart 27-3) may assist a pa-tient to cope with changes that occur with
pacemaker treatment.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
After
pacemaker insertion, the patient’s hospital stay may be less than 1 day, and
follow-up in an outpatient clinic or office is com-mon. The patient’s anxiety
and feelings of vulnerability may in-terfere with the ability to learn
information provided. Nurses often need to include home caregivers in the
teaching and pro-vide printed materials for use by the patient and caregiver.
Prior-ities for learning are established with the patient and caregiver.
Teaching may include the importance of periodic pacemaker monitoring, promoting
safety, avoiding infection, and sources of electromagnetic interference (see
Chart 27-3).
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1)
Remains free of infection
a)
Has normal temperature
b) Has white blood cell count within normal range (5,000 to 10,000/mm3)
c) Exhibits no redness or swelling of
pacemaker insertion site
2)
Adheres to a self-care program
a)
Responds appropriately when queried
about the signs and symptoms of infection
b)
Identifies when to seek medical
attention (as demon-strated in responses to signs and symptoms)
c)
Adheres to monitoring schedule
d)
Describes appropriate methods to
avoid electromag-netic interference
3)
Maintains pacemaker function (see
Chart 27-3)
a)
Measures and records pulse rate at
regular intervals
b)
Experiences no abrupt changes in
pulse rate or rhythm
Related Topics