Chapter: Medical Surgical Nursing: Management of Patients With Dysrhythmias and Conduction Problems
Cardioversion and Defibrillation - Adjunctive Modalities and Management
CARDIOVERSION AND DEFIBRILLATION
Cardioversion
and defibrillation are treatments for tachydysrhythmias. They are used to
deliver an electrical current to depolarize a critical mass of myocardial
cells. When the cells repolarize, the sinus node is usually able to recapture
its role as the heart’s pacemaker. One major difference between cardioversion
and defibrillation has to do with the timing of the delivery of electrical
current.Another major difference concerns the circumstance: defibrillation is
usually performed as an emergency treatment, whereas cardioversion is usually,
but not always, a planned procedure.
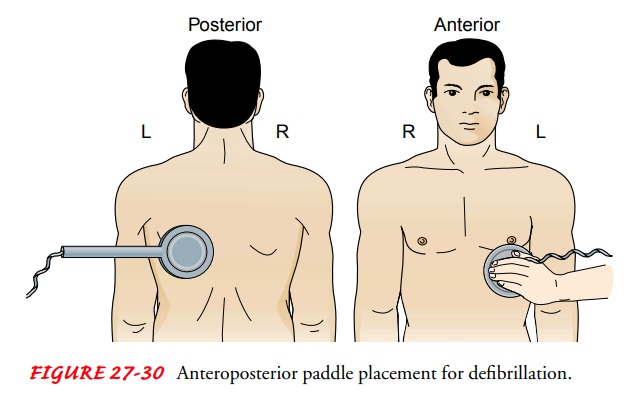
Electrical
current may be delivered through paddles or conductor pads. Both paddles may be
placed on the front of the chest (Fig. 27-29), which is the standard paddle
placement, or one paddle may be placed on the front of the chest and the other
connected to an adapter with a long handle and placed under the patient’s back,
which is called an anteroposterior placement (Fig. 27-30).

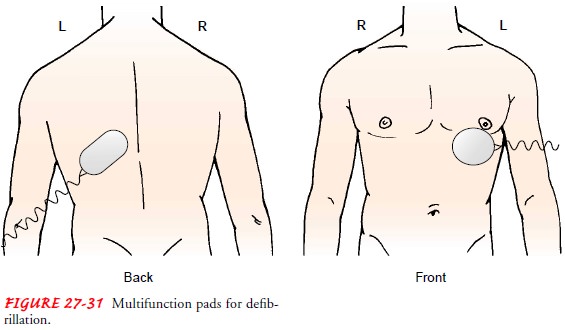
Instead
of paddles, defibrillator multifunction conductor pads may be used (Fig.
27-31). The pads, which contain a conductive medium, are placed in the same
position as the paddles. They are connected to the defibrillator and allow for
hands-off defibrilla-tion. This method reduces the risks of touching the
patient dur-ing the procedure and increases electrical safety. AEDs use this
type of delivery for the electrical current.
Whether
using pads or paddles, the nurse must observe two safety measures. First,
maintain good contact between the pads or paddles (with a conductive medium)
and the patient’s skin to prevent electrical current from leaking into the air
(arcing) when the defibrillator is discharged. Second, ensure that no one is in
contact with the patient or with anything that is touching the pa-tient when
the defibrillator is discharged, to minimize the chance that electrical current
will be conducted to anyone other than the patient.
When
performing defibrillation or cardioversion, the nurse should remember these key
points:
·
Use multifunction conductor pads or
paddles with a con-ducting agent between the paddles and the skin (the
con-ducting agent is available as a sheet, gel, or paste).
·
Place paddles or pads so that they
do not touch the patient’s clothing or bed linen and are not near medication
patches or direct oxygen flow.
·
If cardioverting, ensure that the
monitor leads are attached to the patient and that the defibrillator is in sync
mode. If defibrillating, ensure that the defibrillator is not in sync mode
(most machines default to the “not-sync” mode).
·
Do not charge the device until ready
to shock; then keep thumbs and fingers off the discharge buttons until paddles
or pads are on the chest and ready to deliver the electrical charge.
·
Exert 20 to 25 pounds of pressure on
the paddles to ensure good skin contact.
·
Before pressing the discharge
button, call “Clear!” three times: As “Clear” is called the first time, ensure
that you are not touching the patient, bed or equipment; as “Clear” is called
the second time, ensure that no one is touching the bed, the patient, or
equipment, including the endotracheal tube or adjuncts; and as “Clear” is
called the third time, per-form a final visual check to ensure you and everyone
else are clear of the patient and anything touching the patient.
·
Record the delivered energy and the
results (cardiac rhythm, pulse).
·
After the event is complete, inspect
the skin under the pads or paddles for burns; if any are detected, consult with
the physician or a wound care nurse about treatment.
Cardioversion
Cardioversion involves
the delivery of a “timed” electrical cur-rent to terminate a tachydysrhythmia.
In cardioversion, the de-fibrillator is set to synchronize with the ECG on a
cardiac monitor so that the electrical impulse discharges during ventricular
depo-larization (QRS complex). Because there may be a short delay until
recognition of the QRS, the discharge buttons must be held down until the shock
has been delivered. The synchronization prevents the discharge from occurring
during the vulnerable pe-riod of repolarization (T wave), which could result in
VT or ven-tricular fibrillation. When the synchronizer is on, no electrical
current will be delivered if the defibrillator does not discern a QRS complex.
Sometimes the lead and the electrodes must be changed for the monitor to
recognize the patient’s QRS complex.
If
the cardioversion is elective, anticoagulation for a few weeks before
cardioversion may be indicated. Digoxin is usually with-held for 48 hours
before cardioversion to ensure the resumption of sinus rhythm with normal
conduction. The patient is in-structed not to eat or drink for at least 8 hours
before the proce-dure. Gel-covered paddles or conductor pads are positioned
front and back (anteroposteriorly) for cardioversion. Before cardioversion, the
patient receives intravenous sedation as well as an analgesic medication or
anesthesia. Respiration is then supported with supplemental oxygen delivered by
a bag-mask-valve device with suction equipment readily available. Although
patients rarely require intubation, equipment is nearby if it is needed. The
amount of voltage used varies from 25 to 360 joules, depending on the
defibrillator’s technology and the type of dysrhythmia. If ventricular fibrillation
occurs after cardioversion, the defibrillator is used to defibrillate the
patient (sync mode is not used).
Indications
of a successful response are conversion to sinus rhythm, adequate peripheral
pulses, and adequate blood pressure. Because of the sedation, airway patency
must be maintained and the patient’s state of consciousness assessed. Vital
signs and oxy-gen saturation are monitored and recorded until the patient is
stable and recovered from sedation and the effects of analgesic medications or
anesthesia. ECG monitoring is required during and after cardioversion.
Defibrillation
Defibrillation is
used in emergency situations as the treatmentof choice for ventricular
fibrillation and pulseless VT. Defibrilla-tion depolarizes a critical mass of
myocardial cells at once; when they repolarize, the sinus node usually
recaptures its role as the pacemaker. The electrical voltage required to
defibrillate the heart is usually greater than that required for cardioversion.
If three de-fibrillations of increasing voltage have been unsuccessful,
cardio-pulmonary resuscitation is initiated and advanced life support
treatments are begun.
The
use of epinephrine or vasopressin may make it easier to convert the dysrhythmia
to a normal rhythm with defibrillation. These drugs may also increase cerebral
and coronary artery blood flow. After the medication is administered and 1
minute of cardio-pulmonary resuscitation is performed, defibrillation is again
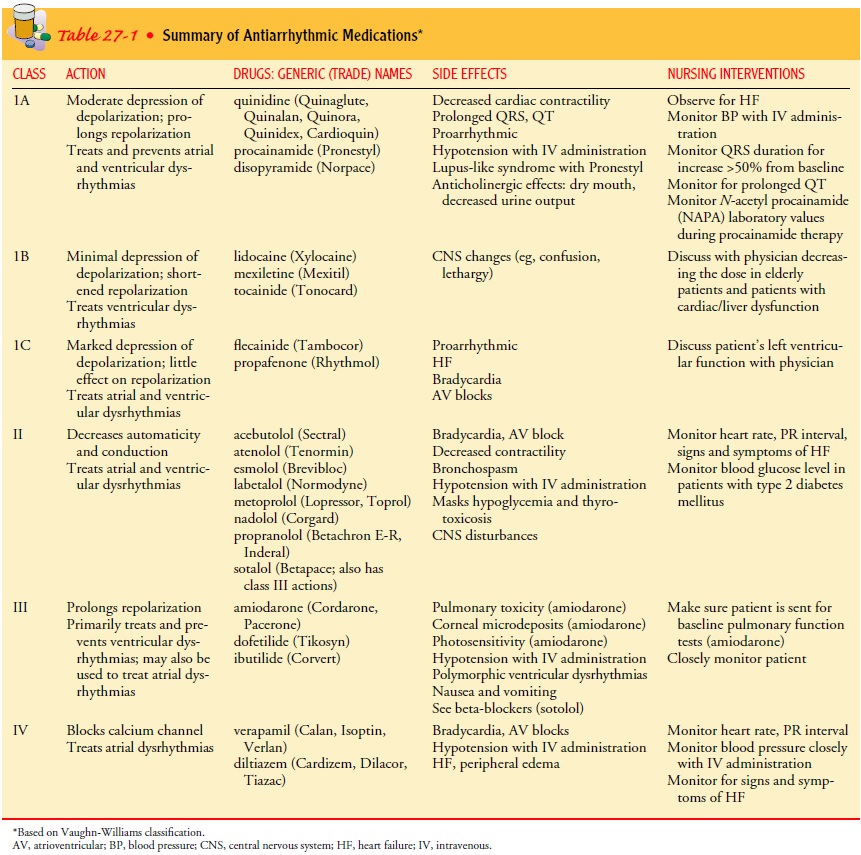
administered. Antiarrhythmic medications such as amiodarone (Cordarone,
Pacerone), lidocaine (Xylocaine), magnesium, or pro-cainamide (Pronestyl) are
given if ventricular dysrhythmia persists (see Table 27-1). This treatment
continues until a stable rhythm resumes or until it is determined that the
patient cannot be revived.
IMPLANTABLE CARDIOVERTER DEFIBRILLATOR
The
implantable cardioverter defibrillator
(ICD) is a device that detects and terminates life-threatening episodes of
VT or ventricular fibrillation in high-risk patients. Patients at high risk are
those who have survived sudden cardiac death syndrome, usu-ally caused by
ventricular fibrillation, or have experienced symp-tomatic VT (syncope
secondary to VT). In addition, an ICD may be indicated for patients who have
survived an MI but are at high risk for cardiac arrest.
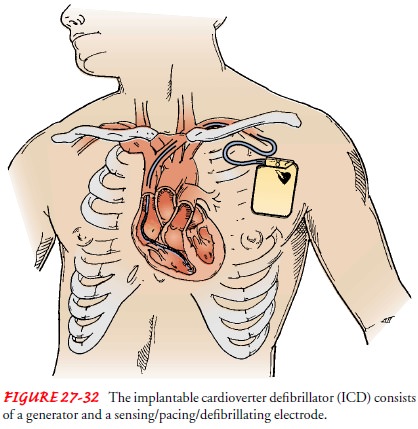
An
ICD consists of a generator and at least one lead that can sense intrinsic
electrical activity and deliver an electrical impulse. The device is usually
implanted much like a pacemaker (Fig. 27-32). ICDs are designed to respond to
two criteria: a rate that exceeds a predetermined level, and a change in the
isoelectric line seg-ments. When a dysrhythmia occurs, rate sensors take 5 to
10 sec-onds to sense the dysrhythmia. Then the device takes several seconds to
charge and deliver the programmed charge through the lead to the heart. Battery
life is about 5 years but varies de-pending on use of the ICD over time. The
battery is checked dur-ing follow-up visits.
Antiarrhythmic
medication usually is administered with this technology to minimize the
occurrence of the tachydysrhythmia and to reduce the frequency of ICD
discharge.
The
first defibrillator, which was implanted in 1980 at Johns Hopkins University,
simply defibrillated the heart. Today, how-ever, several devices are available,
and many are programmed for multiple treatments (Atlee & Bernstein, 2001).
Each device of-fers a different delivery sequence, but all are capable of
delivering high-energy (high-intensity) defibrillation to treat a tachycardia
(atrial or ventricular). The device may deliver up to six shocks if necessary.
Some ICDs can respond with antitachycardia pacing, in which the device delivers
electrical impulses at a fast rate in an attempt to disrupt the tachycardia, by
low-energy (low-intensity) cardioversion, by defibrillation, or all three
(Atlee & Bernstein, 2001). Some also have pacemaker capability if the
patient devel-ops bradycardia, which sometimes occurs after treatment of the
tachycardia. Usually the mode is VVI (V, paces the ventricle; V, senses
ventricular activity; I, paces only if the ventricles do not de-polarize)
(Atlee & Bernstein, 2001). Some ICDs also deliver low-energy cardioversion,
and some also treat atrial fibrillation (Bubien & Sanchez, 2001; Daoud et
al., 2000). Which device is used and how it is programmed depends on the
patient’s dysrhythmia.
Complications
are similar to those associated with pacemaker insertion. The primary
complication associated with the ICD is surgery-related infection. There are a
few complications associ-ated with the technical aspects of the equipment, such
as prema-ture battery depletion and dislodged or fractured leads. Despite the
possible complications, the consensus among clinicians is that the benefits of
ICD therapy exceed the risks.
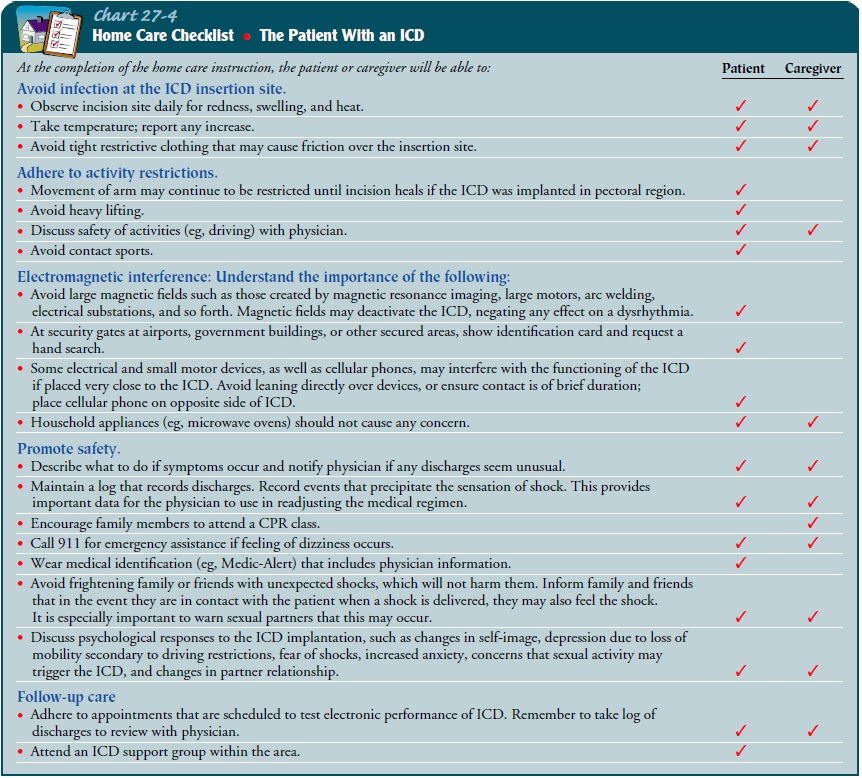
Nursing
interventions for the patient with an ICD are pro-vided throughout the
preoperative, perioperative, and postoper-ative phases. In addition to
providing the patient and family with explanations regarding implantation of
the ICD in the preoper-ative phase, the nurse may need to manage acute episodes
of life-threatening dysrhythmias. In the perioperative and postoperative
phases, the nurse carefully observes the patient’s responses to the ICD and
provides the patient and family with further teaching as needed (White, 2000)
(Chart 27-4). The nurse can also assist the patient and family in making
lifestyle changes necessitated by the dysrhythmia and resulting ICD
implantation (Dougherty, Benoliel, & Bellin, 2000).
Related Topics