Chapter: Basic & Clinical Pharmacology : Adrenoceptor Antagonist Drugs
Clinical Toxicity Of The Beta-Receptor Antagonist Drugs
CLINICAL TOXICITY OF THE
BETA-RECEPTOR ANTAGONIST DRUGS
Many
adverse effects have been reported for propranolol but most are minor.
Bradycardia is the most common adverse cardiac effect of β-blocking drugs.
Sometimes patients note coolness of hands and feet in winter. Central nervous
system effects include mild sedation, vivid dreams, and rarely, depression.
Discontinuing the use of β blockers in any patient who develops
psychiatric depression should be seriously considered if clinically feasible. It
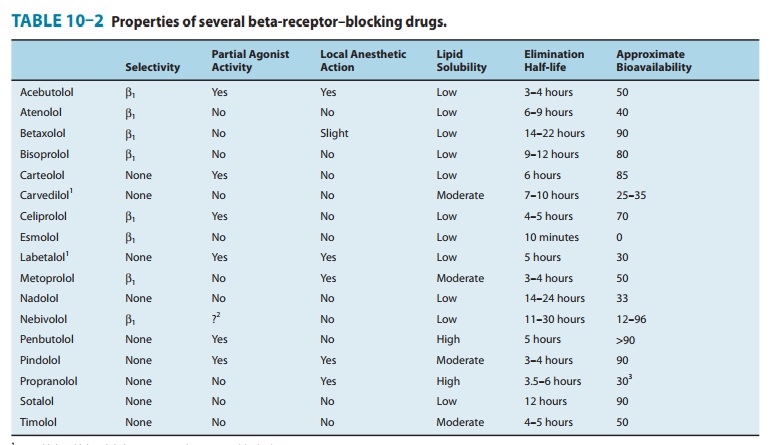
has been claimed that β-receptor antagonist drugs with low lipid
solubility are associated with a lower incidence of central nervous system
adverse effects than compounds with higher lipid solubil-ity (Table 10–2).
Further studies designed to compare the central nervous system adverse effects
of various drugs are required before specific recommendations can be made,
though it seems reason-able to try the hydrophilic drugs nadolol or atenolol in
a patient who experiences unpleasant central nervous system effects with other β blockers.
The
major adverse effects of β-receptor antagonist drugs relate to the
predictable consequences of β blockade. Beta2-receptor blockade
associated with the use of nonselective agents commonly causes worsening of
preexisting asthma and other forms of airway obstruction without having these
consequences in normal indi-viduals. Indeed, relatively trivial asthma may
become severe afterblockade. However, because of their lifesaving potential in
car-diovascular disease, strong consideration should be given to
indi-vidualized therapeutic trials in some classes of patients, eg, thosewith
chronic obstructive pulmonary disease who have appropriate indications for β blockers. While β1-selective drugs may
have less effect on airways than nonselective β antagonists, they must be used very
cautiously in patients with reactive airway disease. Beta1-selective
antagonists are generally well tolerated in patients with mild to moderate
peripheral vascular disease, but caution is required in patients with severe
peripheral vascular disease or vasospastic disorders.
Beta-receptor
blockade depresses myocardial contractility and excitability. In patients with
abnormal myocardial function, cardiac output may be dependent on sympathetic
drive. If this stimulus is removed by β blockade, cardiac decompensation may ensue.
Thus, caution must be exercised in starting a β-receptor antagonist in patients with compensated
heart failure even though long-term use of these drugs in these patients may
prolong life. A life-threatening adverse cardiac effect of a β antagonist may be
overcome directly with isoproterenol or with glucagon (glucagon stimulates the
heart via glucagon receptors, which are not blocked by β antagonists), but neither of these methods is
without hazard. A very small dose of a β antagonist (eg, 10 mg of propranolol) may
provoke severe cardiac failure in a susceptible individual. Beta blockers may
interact with the calcium antagonist verapamil; severe hypotension,
bradycardia, heart failure, and cardiac con-duction abnormalities have all been
described. These adverse effects may even arise in susceptible patients taking
a topical (oph-thalmic) β blocker and oral verapamil.
Patients
with ischemic heart disease or renovascular hyperten-sion may be at increased
risk if β
blockade is suddenly interrupted. The mechanism of this effect might involve
up-regulation of the number of β receptors. Until better evidence is available
regarding the magnitude of the risk, prudence dictates the gradual tapering
rather than abrupt cessation of dosage when these drugs are dis-continued,
especially drugs with short half-lives, such as propra-nolol and metoprolol.
The incidence of hypoglycemic episodes exacerbated by β-blocking agents in diabetics is unknown. Nevertheless, it isinadvisable to use β antagonists in insulin-dependent diabetic patients who are subject to frequent hypoglycemic reactions if alternative therapies are available. Beta1-selective antagonists offer some advantage in these patients, since the rate of recovery from hypoglycemia may be faster compared with that in diabetics receiving nonselective β-adrenoceptor antagonists. There is con-siderable potential benefit from these drugs in diabetics after a myocardial infarction, so the balance of risk versus benefit must be evaluated in individual patients.
Related Topics