Chapter: Basic & Clinical Pharmacology : Adrenoceptor Antagonist Drugs
Clinical Pharmacology of the Beta Receptor Blocking Drugs
CLINICAL
PHARMACOLOGY OF THE BETA RECEPTOR BLOCKING DRUGS
Hypertension
The
β-adrenoceptor–blocking
drugs have proved to be effective and well tolerated in hypertension. Although
many hypertensive patients respond to a β blocker used alone, the drug is often used
with either a diuretic or a vasodilator. In spite of the short half-life of
many β
antagonists, these drugs may be administered once or twice daily and still have
an adequate therapeutic effect. Labetalol, a competitive α and β antagonist, is
effective in hypertension, though its ultimate role is yet to be determined.
Use of these agents is discussed in greater detail earily. There is some
evidence that drugs in this class may be less effective in the elderly and in
individuals of African ancestry. However, these differences are relatively
small and may not apply to an individual patient. Indeed, since effects on
blood pressure are easily measured, the therapeutic outcome for this indication
can be readily detected in any patient.
Ischemic Heart Disease
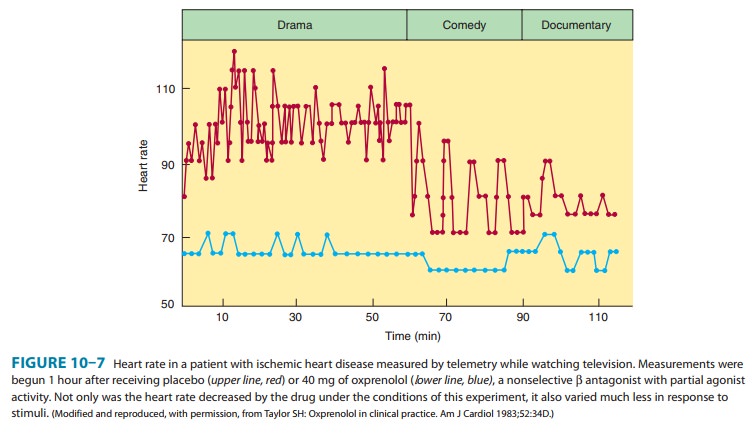
Beta-adrenoceptor
blockers reduce the frequency of anginal epi-sodes and improve exercise
tolerance in many patients with angina . These actions relate to the blockade
of cardiac β
receptors, resulting in decreased cardiac work and reduction in oxy-gen demand.
Slowing and regularization of the heart rate may contribute to clinical
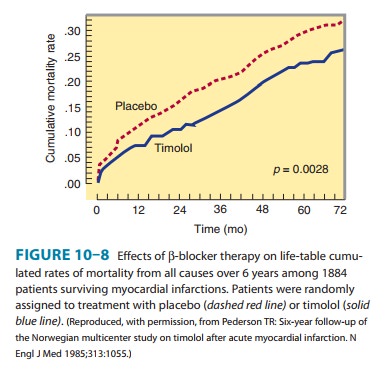
benefits (Figure 10–7). Multiple large-scale prospective studies indicate that
the long-term use of timolol,
pro-pranolol, or metoprolol in
patients who have had a myocardialinfarction prolongs survival (Figure 10–8).
At the present time, data are less compelling for the use of other than the
three mentioned β-adrenoceptor
antagonists for this indication. It is significant thatsurveys in many
populations have indicated that β-receptor antago-nists are underused, leading
to unnecessary morbidity and mortal-ity. In addition, β-adrenoceptor antagonists are strongly
indicated in the acute phase of a myocardial infarction. In this setting,
relative contraindications include bradycardia, hypotension, moderate or severe
left ventricular failure, shock, heart block, and active airways disease. It
has been suggested that certain polymorphisms in β2-adrenoceptor genes may influence survival
among patients receiving antagonists after acute coronary syndromes.
Cardiac Arrhythmias
Beta
antagonists are often effective in the treatment of both supraventricular and
ventricular arrhythmias . It has been suggested that the improved survival
following myocardial infarction in patients using β antagonists (Figure 10–8) is due to
suppression of arrhythmias, but this has not been proved. By increasing the
atrioventricular nodal refractory period, β antagonists slow ventricular response rates
in atrial flutter and fibrillation. These drugs can also reduce ventricular
ectopic beats, particularly if the ectopic activity has been precipitated by
catecholamines. Sotalol has antiarrhythmic effects involving ion channel
blockade in addition to its β-blocking action;.
Heart Failure
Clinical
trials have demonstrated that at least three β antagonists— metoprolol, bisoprolol, and
carvedilol—are effective in reducing mortality in selected patients with
chronic heart failure. Although administration of these drugs may worsen acute
congestive heart failure, cautious long-term use with gradual dose increments
in patients who tolerate them may prolong life. Although mecha-nisms are
uncertain, there appear to be beneficial effects on myocardial remodeling and in
decreasing the risk of sudden death .
Other Cardiovascular Disorders
Beta-receptor
antagonists have been found to increase stroke vol-ume in some patients with
obstructive cardiomyopathy. This beneficial effect is thought to result from
the slowing of ventricu-lar ejection and decreased outflow resistance. Beta
antagonists are useful in dissecting aortic aneurysm to decrease the rate of
devel-opment of systolic pressure. Beta antagonists are also useful in selected
at-risk patients in the prevention of adverse cardiovascular outcomes resulting
from noncardiac surgery.
Glaucoma (See Box: The Treatment of Glaucoma)
Systemic
administration of β-blocking
drugs for other indications was found serendipitously to reduce intraocular
pressure in patients with glaucoma. Subsequently, it was found that topical
administration also reduces intraocular pressure. The mechanism appears to
involve reduced production of aqueous humor by the ciliary body, which is
physiologically activated by cAMP. Timolol and related β antagonists are suitable for local use in the
eye because they lack local anesthetic properties. Beta antagonists appear to
have an efficacy comparable to that of epinephrine or pilocarpine in open-angle
glaucoma and are far better tolerated by most patients. While the maximal daily
dose applied locally (1 mg) is small compared with the systemic doses commonly
used in the treatment of hypertension or angina (10–60 mg), sufficient timolol
may be absorbed from the eye to cause serious adverse effects on the heart and
airways in susceptible individuals. Topical timolol may interact with orally
administered verapamil and increase the risk of heart block.
Betaxolol,
carteolol, levobunolol, and metipranolol are also approved for the treatment of
glaucoma. Betaxolol has the poten-tial advantage of being β1-selective; to what
extent this potential advantage might diminish systemic adverse effects remains
to be determined. The drug apparently has caused worsening of pulmo-nary
symptoms in some patients.
Hyperthyroidism
Excessive
catecholamine action is an important aspect of the pathophysiology of
hyperthyroidism, especially in relation to the heart . The β antagonists are
beneficial in this condition. The effects presumably relate to blockade of
adreno-ceptors and perhaps in part to the inhibition of peripheral conver-sion
of thyroxine to triiodothyronine. The latter action may vary from one β antagonist to another.
Propranolol has been used extensively in patients with thyroid storm (severe
hyperthyroid-ism); it is used cautiously in patients with this condition to
control supraventricular tachycardias that often precipitate heart failure.
Neurologic Diseases
Propranolol
reduces the frequency and intensity of migraineheadache.
Otherβ-receptor
antagonists with preventive efficacyinclude metoprolol and probably also
atenolol, timolol, and nadolol. The mechanism is not known. Since sympathetic
activ-ity may enhance skeletal muscle tremor, it is not surprising that
antagonists have been found to reduce certain tremors . The somatic manifestations of anxiety may respond
dramatically to low doses of propranolol, particularly when taken
prophylactically. For example, benefit has been found in musicians with performance anxiety (“stage fright”).
Propranolol may contribute to the symptomatic treatment of alcohol withdrawal
in some patients.
Miscellaneous
Beta-receptor
antagonists have been found to diminish portal vein pressure in patients with
cirrhosis. There is evidence that both propranolol and nadolol decrease the
incidence of the first episode of bleeding from esophageal varices and decrease
the mortality rate associated with bleeding in patients with cirrhosis. Nadolol
in combination with isosorbide mononitrate appears to be more efficacious than
sclerotherapy in preventing rebleeding in patients who have previously bled
from esophageal varices. Variceal band ligation in combination with a β antagonist may be
more efficacious.
Related Topics