Chapter: Basic & Clinical Pharmacology : Adrenoceptor Antagonist Drugs
Pharmacodynamics of the Beta-Receptor Antagonist Drugs
Pharmacodynamics of the
Beta-Receptor Antagonist Drugs
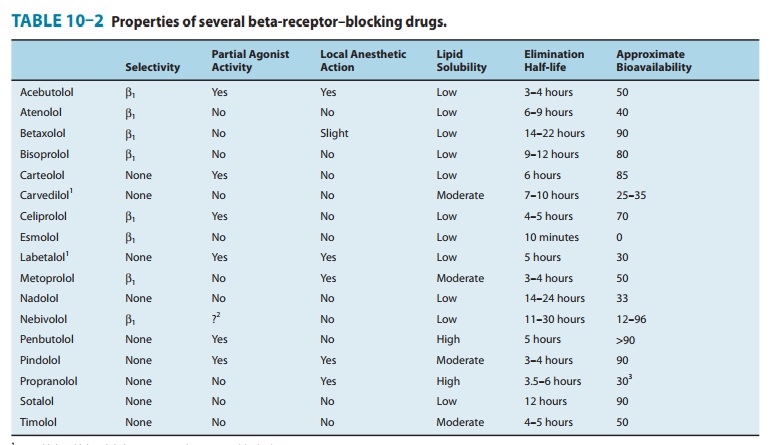
Most
of the effects of these drugs are due to occupation and blockade of β receptors. However,
some actions may be due to other effects, including partial agonist activity at
β
receptors and local anesthetic action, which differ among the β blockers (Table
10–2).
A. Effects on the Cardiovascular System
Beta-blocking
drugs given chronically lower blood pressure in patients with hypertension .
The mechanisms involved are not fully understood but probably include
suppres-sion of renin release and effects in the central nervous system. These
drugs do not usually cause
hypotension in healthy individu-als with normal blood pressure.
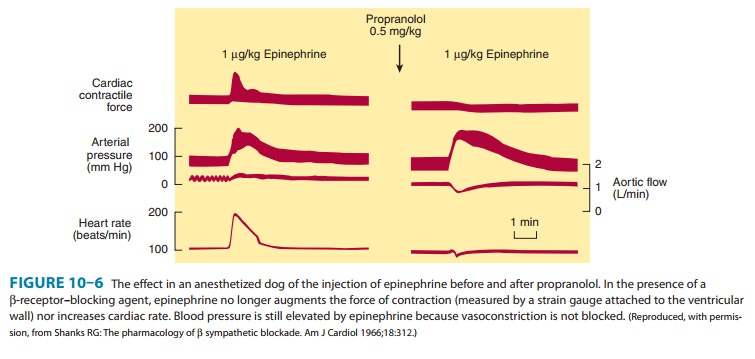
Beta-receptor
antagonists have prominent effects on the heart (Figure 10–6) and are very
valuable in the treatment of angina and
chronic heart failure and fol-lowing
myocardial infarction . The negative ino-tropic and chronotropic effects
reflect the role of adrenoceptors in regulating these functions. Slowed
atrioventricular conduction with an increased PR interval is a related result
of adrenoceptor blockade in the atrioventricular node. In the vascular system, β-receptor blockade
opposes β2-mediated vasodilation. This mayacutely lead to a rise in
peripheral resistance from unopposed α-receptor–mediated effects as the sympathetic
nervous systemdischarges in response to lowered blood pressure due to the fall
in cardiac output. Nonselective and β1-blocking drugs antagonize the release of
renin caused by the sympathetic nervous system. Overall, although the acute
effects of these drugs may include a rise in peripheral resistance, chronic
drug administration leads to a fall in peripheral resistance in patients with
hypertension.
B. Effects on the Respiratory Tract
Blockade of the β2 receptors in bronchial smooth muscle may lead to an increase in airway resistance, particularly in patients with asthma. Beta1-receptor antagonists such as metoprolol and atenolol may have some advantage over nonselective β antagonists when blockade of β1 receptors in the heart is desired and β2-receptor blockade is undesirable. However, no currently available β1-selective antagonist is sufficiently specific to completely avoid interactions with β2 adrenoceptors. Consequently, these drugs should generally be avoided in patients with asthma. On the other hand, many patients with chronic obstructive pulmonary disease (COPD) may tolerate these drugs quite well and the benefits, for example in patients with concomitant ischemic heart disease, may outweigh the risks.
C. Effects on the Eye
Beta-blocking
agents reduce intraocular pressure, especially in glaucoma. The mechanism
usually reported is decreased aqueous humor production. (See Clinical
Pharmacology and Box: The Treatment of Glaucoma.)
D. Metabolic and Endocrine Effects
Beta-receptor
antagonists such as propranolol inhibit sympathetic nervous system stimulation
of lipolysis. The effects on carbohy-drate metabolism are less clear, though
glycogenolysis in the human liver is at least partially inhibited after β2-receptor block-ade.
Glucagon is the primary hormone used to combat hypogly-cemia; it is unclear to
what extent β
antagonists impair recovery from hypoglycemia, but they should be used with
caution in insulin-dependent diabetic patients. This may be particularly
important in diabetic patients with inadequate glucagon reserve and in
pancreatectomized patients since catecholamines may be the major factors in
stimulating glucose release from the liver in response to hypoglycemia. Beta1-receptor–selective
drugs may be less prone to inhibit recovery from hypoglycemia. Beta-receptor
antagonists are much safer in those type 2 diabetic patients who do not have
hypoglycemic episodes.
The
chronic use of β-adrenoceptor
antagonists has been associ-ated with increased plasma concentrations of
very-low-density lipoproteins (VLDL) and decreased concentrations of HDL
choles-terol. Both of these changes are potentially unfavorable in terms of
risk of cardiovascular disease. Although low-density lipoprotein (LDL)
concentrations generally do not change, there is a variable decline in the HDL
cholesterol/LDL cholesterol ratio that may increase the risk of coronary artery
disease. These changes tend to occur with both selective and nonselective β blockers, though they
may be less likely to occur with β blockers possessing intrinsic
sym-pathomimetic activity (partial agonists). The mechanisms by which β-receptor antagonists
cause these changes are not understood,though changes in sensitivity to insulin
action may contribute.
E. Effects Not Related to Beta-Blockade
Partial
β-agonist
activity was significant in the first β-blocking drug synthesized,
dichloroisoproterenol. It has been suggested that retention of some intrinsic
sympathomimetic activity is desirable to prevent untoward effects such as
precipitation of asthma or excessive bradycardia. Pindolol and other partial
agonists are noted in Table 10–2. It is not yet clear to what extent partial
ago-nism is clinically valuable. Furthermore, these drugs may not be as
effective as the pure antagonists in secondary prevention of myo-cardial
infarction. However, they may be useful in patients who develop symptomatic
bradycardia or bronchoconstriction in response to pure antagonist β-adrenoceptor drugs,
but only if they are strongly indicated for a particular clinical indication.
Local
anesthetic action, also known as “membrane-stabilizing” action, is a prominent
effect of several β
blockers (Table 10–2). This action is the result of typical local anesthetic
blockade of sodium channels and can be
demonstrated experimentally in isolated neurons, heart muscle, and skeletal
muscle membrane. However, it is unlikely that this effect is important after
systemic administration of these drugs, since the concentration in plasma
usually achieved by these routes is too low for the anesthetic effects to be
evident. The membrane-stabilizing β blockers are not used topically on the eye,
because local anesthesia of the cornea would be highly undesirable. Sotalol is
a nonselective β-receptor
antagonist that lacks local anesthetic action but has marked class III
antiarrhythmic effects, reflecting potassium channel blockade .
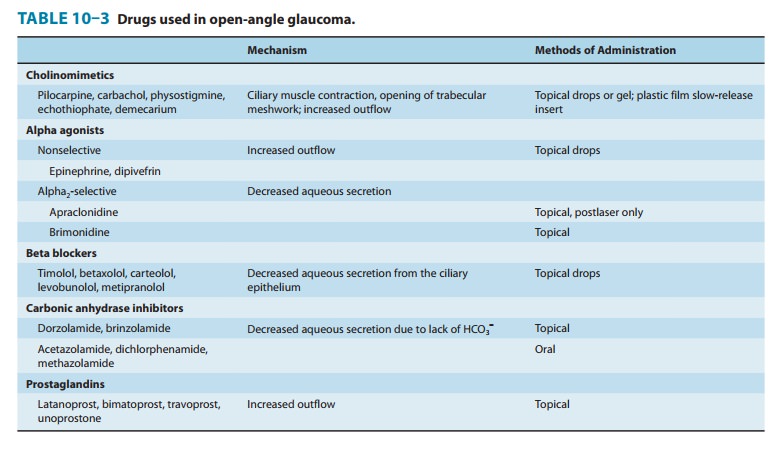
The Treatment of Glaucoma
Glaucoma is
a major cause of blindness and of great pharma-cologic interest because the
chronic form often responds to drug therapy. The primary manifestation is
increased intraoc-ular pressure not initially associated with symptoms. Without
treatment, increased intraocular pressure results in damage to the retina and
optic nerve, with restriction of visual fields and, eventually, blindness.
Intraocular pressure is easily mea-sured as part of the routine ophthalmologic
examination. Two major types of glaucoma are recognized: open-angle and
closed-angle (also called narrow-angle). The closed-angle form is associated
with a shallow anterior chamber, in which a dilated iris can occlude the
outflow drainage pathway at the angle between the cornea and the ciliary body
(see Figure 6–9). This form is associated with acute and painful increases of
pressure, which must be controlled on an emergency basis with drugs or
prevented by surgical removal of part of the iris (iridectomy). The open-angle
form of glaucoma is a chronic condition, and treatment is largely
pharmacologic. Because intraocular pressure is a function of the balance
between fluid input and drainage out of the globe, the strategies for the
treatment of open-angle glaucoma fall into two classes: reduction of aqueous
humor secretion and enhancement of aqueous outflow. Five general groups of
drugs—cholinomi-metics, α agonists, β blockers, prostaglandin F2α
analogs, and diuretics—have been found to be useful in reducing intraoc-ular
pressure and can be related to these strategies as shown in Table 10–3. Of the
five drug groups listed in Table 10–3, the prostaglandin analogs and the β
blockers are the most popu-lar. This popularity results from convenience (once-
or twice-daily dosing) and relative lack of adverse effects (except, in the
case of β blockers, in patients with asthma or cardiac pacemaker or conduction
pathway disease). Other drugs that have been reported to reduce intraocular
pressure include prostaglandin E2 and marijuana. The use of drugs in
acute closed-angle glaucoma is limited to cholinomimetics, aceta-zolamide, and
osmotic agents preceding surgery. The onset of action of the other agents is
too slow in this situation.
Related Topics