Chapter: Modern Medical Toxicology: Food Poisons: Food Poisoning
Clinical Features - Clostridium Microbial Food Poisoning
![]() Clinical
Features
Clinical
Features
Food-borne botulism:
·
This is usually caused in humans by types A, B, E, and
rarely F. The initial phase of the disease is often so subtle as to go
unnoticed or misdiagnosed. Type A botulism generally causes a more severe
illness, and is more likely to require intubation than either type B or E
botulism. In general, the earlier the onset of symptoms, the more serious the
disease and the more protracted the course. Even a small taste of contaminated
food may result in illness.
·
Nausea, vomiting, thirst, abdominal pain. Abdominal cramps
may be an early symptom of foodborne botu-lism. Marked abdominal distension
with absent bowel sounds may be present due to paralytic ileus.
·
Constipation; refusal to feed and diarrhoea have been
reported in a few cases of paediatric botulism.
·
Ptosis, difficulty with visual accommodation, photo-phobia,
mydriasis, and diplopia (due to ocular paresis). Strabismus and nystagmus have
also been reported. The triad of extraocular muscle palsy, pupillary
dysfunction, and ptosis is said to be predictive of illness severity (i.e. the
development of respiratory failure). Early onset of neurological symptoms,
particularly ocular, generally indicates a more severe infection and worse
prognosis.
·
Dizziness: Postural dizziness is a relatively frequent
symptom resulting from cholinergic blockade.
·
Dry mouth,* soreness of throat due to drying of pharynx,
dryness of lacrimal secretions.
·
Dysphonia, dysarthria, dysphagia.
·
Bilaterally symmetrical descending motor paralysis,
beginning with abducens (VI) or oculomotor (III) nerve palsy, and progressing
to respiratory insufficiency. The risk of ventilatory failure is greatest
within the first two days of hospitalisation. Respiratory arrest may develop
suddenly in patients with apparently adequate respira-tory reserve; absent
signs and symptoms of respiratory insufficiency are not necessarily indicative
of normal lung function. Respiratory failure can also develop insid-iously, and
may be difficult to diagnose. Many patients experience dyspnoea of varying
degree for a year or more after recovery from botulism, despite essentially
normal pulmonary function. The cause of dyspnoea may be a residual defect of
respiratory muscles.
·
Urinary retention (especially in Type E botulism): due to
cholinergic blockade.
·
Mental status, sensory examination, reflexes, body
temperature, and pulse are all usually normal.
·
Cardiac arrest may occur in patients with respiratory
failure. It is not known whether arrest is secondary to ![]() hypoxia or due to a direct effect of
botulinum toxin on the myocardium.
hypoxia or due to a direct effect of
botulinum toxin on the myocardium.
·
A syndrome of inappropriate secretion of antidiuretic
hormone has been reported in some cases of botulism. Most of these patients
were on a ventilator when this occurred.
·
Toxicoinfectious Botulism: There are a few reports
ofgastrointestinal colonisation by C.
botulinum spores in adults resulting in cases of adult infectious botulism
(the in vivo toxin that is produced is similar to that of infant botulism).
Several factors are associated with this form of botulism: GIT abnormalities
(e.g. achlorhydria), antibiotic therapy disrupting the normal GI flora, a
history of abdominal surgery (e.g. gastrectomy), etc.
·
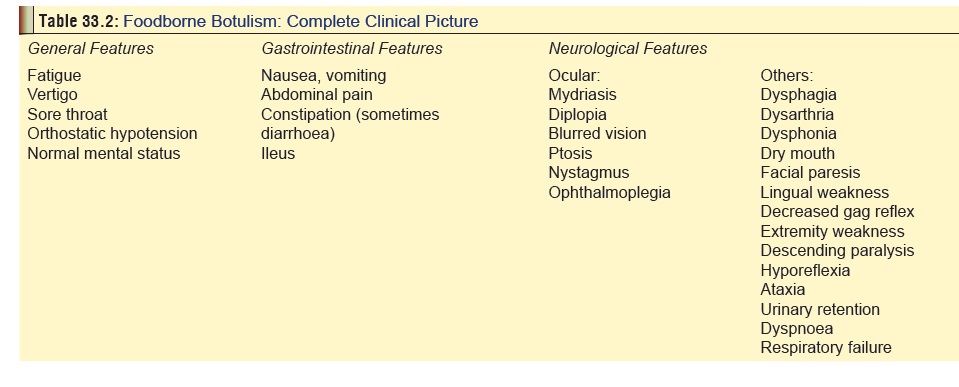
A detailed list of symptoms and signs is mentioned in Table 33.2. Mortality is estimated to
be less than 10%with symptomatic and supportive care.
·
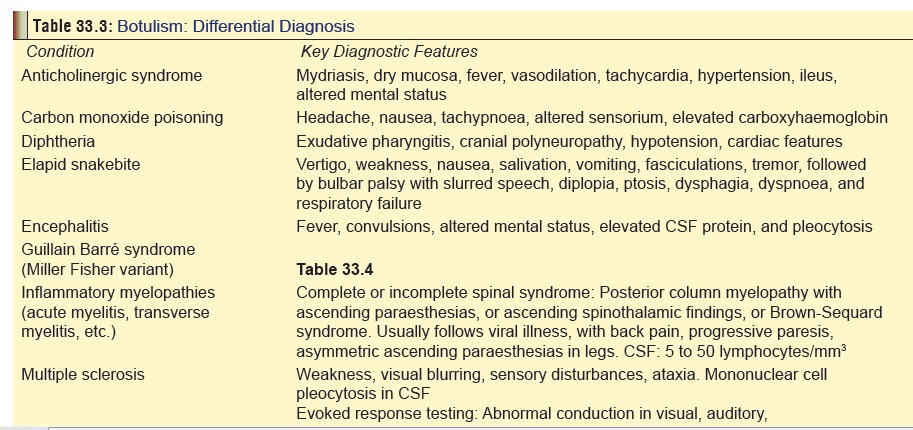
Differential Diagnosis: The common conditionsconfused with
botulism are presented in Table 33.3,
along with clues to help resolve a given case that may appear perplexing. The
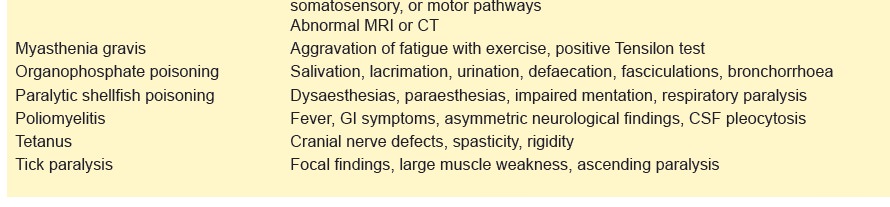
condition that is most often confounding is Guillain Barre´ syndrome,
especially the Miller Fisher variant (Table
33.4).
· Treatment: Supportive measures.
Wound botulism
This
is a rare, life-threatening complication of trauma which occurs after spores of
Cl. botulinum have germinated in a
wound and produced botulinum toxin resulting in flaccid paralysis. It can also
result from intravenous drug abuse. Of late, cocaine and heroin (especially
“black tar heroin” which is often injected subcutaneously) have been
increasingly associated with cases of wound botulism. Deep wounds, crush
injury, or compound fracture treated with open reduction are invariably the
type of trauma predisposing to wound botulism. Incubation period varies from 4
to 18 days.
Clinical Features:
––
Fever (usually associated with sinusitis, abscess, or tissue infection
which acts as the focus of infection).
––
Absence of GI manifestations.
–– Cranial nerve palsies resulting
in ptosis, diplopia, poor accommodation, ophthalmoplegia,
dysphagia, dysphonia, and dysarthria.
––
Other neurological features such as descending flaccid paralysis, shortness of
breath, and respira-tory failure.
Infant botulism
·
Infant botulism is said to be the commonest form of
botulism. Since 1976, when the first case was reported till 2005, more than
2000 hospitalisations have been documented. Of these, 95% occurred in the USA,
and 99% were due to botulinum neurotoxin type A or B. Most cases involved
infants of 1 to 3 months age (range 1 month to 1 year).
·
It is postulated that infant botulism is the result of
inges-tion of Cl. botulinum organisms
with subsequent in vivo production of
toxin, followed by gut absorption. Some investigators suggest that bacterial
growth associated with breastfeeding may favour Bifibobacterium devel-opment, instead of bacteria known to inhibit Cl. botu-linum (i.e., Coliforme, Enterococcus, and Bacteroides species). Of all the food
items associated with infant botulism, honey is said to be the commonest food
source contaminated with Cl. botulinum
spores.
Clinical features of infant botulism
include constipation, feeding difficulty, feeble crying, and a “floppy” baby
with decreased muscle tone, particularly of the neck and limbs. Loss of facial
grimacing, ophthalmoplegia, diminished gag reflex, dysphagia, poor anal
sphincter tone, and respiratory failure have also been reported.
Related Topics