Chapter: Case Study in Obstetrics and Gynaecology: Early Pregnancy
Case Study Reports: Bleeding in Early Pregnancy
BLEEDING IN EARLY PREGNANCY
History
A
23-year-old woman is referred by her general
practitioner with vaginal
bleeding. She noticed that there was blood on the toilet
paper 2 days ago, and following this she has had
bright red spotting intermittently. She has no pain and there are no urinary
or bowel symptoms.
Her
last menstrual period
started 9 weeks
and 6 days ago and she has a regular
31-day cycle. She had a positive
home urine pregnancy test 3 weeks
ago after she realized she had
missed a period and was feeling very tired. This is her first pregnancy. She had been using
condoms but with poor compliance, so the pregnancy was unplanned but
she is now happy about it.
She
is generally well,
only having been admitted to hospital once in the past for an append- ectomy at the age of 17 years. She takes no medication, does not smoke
and drinks min- imal alcohol. She denies
any use of recreational drugs.
Examination
The
woman is apyrexial. The blood pressure
is 120/65 mmHg
and heart rate 78/min. The abdomen is soft and
non-tender with no palpable uterus
or other masses.
Questions
·
How
would you interpret the ultrasound result?
·
What further examination, investigations or management would
you like to perform or request?
ANSWER
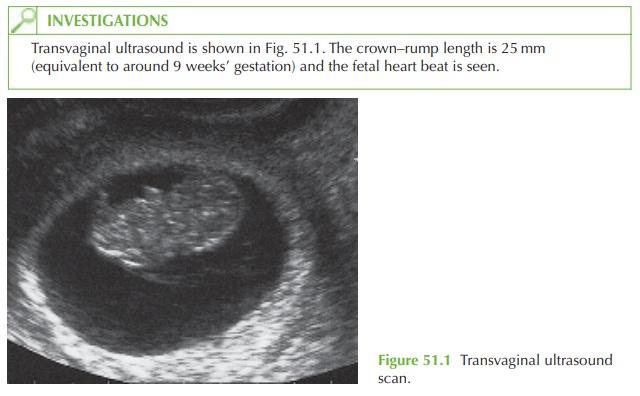
The ultrasound scan shows a viable
single intrauterine pregnancy. The crown–rump length is compatible with
the gestational age
by menstrual dates,
especially as the
woman reports a long menstrual cycle
(3 days longer
than normal, therefore gestational age
would be 3 days less
than the ‘normal’). Where there is a significant discrepancy with
menstrual and ultrasound gestational age estimation (e.g. more than
7 days), one
should consider the possibility of inaccurate reporting of the last
menstrual period date,
irregular cycles leading to inaccurate estimated ovulation date, or of a possible growth-retarded fetus which may possibly
be destined to miscarry.
In
this case, as the ultrasound is reassuring the diagnosis would
be of a ‘threatened miscarriage’.
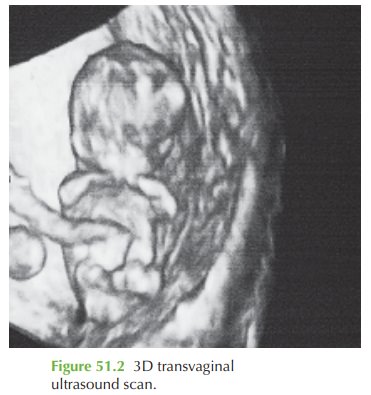
Figure 51.2 shows
a three-dimensional image
of the fetus, demonstrating the developing
limbs and the physiological midgut
herniation which occur
at this developmental stage.
Further management
A speculum examination should be
performed. The possible findings may be:
·
normal appearance
·
cervical ectropion (often associated with postcoital bleeding)
·
cervicitis (common with chlamydia)
·
cervical polyp
·
cervical malignancy (rare but should not be missed)
·
open cervix possibly with products or clots in the os.
No
further investigations are
necessary at this
stage – the
amount of bleeding is unlikely to have caused anaemia.
Rhesus status is irrelevant as anti-D immunoglobulin is only recommended with
bleeding after 12 weeks’ gestation, where the uterus
is instrumented or where an ectopic
pregnancy is treated
surgically.
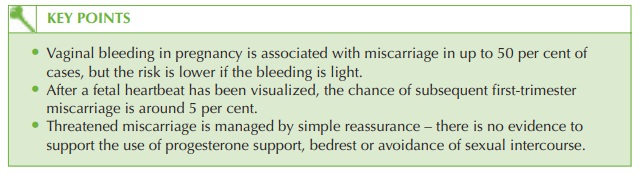
Management in this case is simple
reassurance. Available evidence
suggests that the preg-
nancy is at less than 5 per cent risk of miscarriage if the fetal
heartbeat is normal
and the
bleeding resolves. There is no evidence
for progesterone, bedrest
or avoidance of sexual
intercourse with threatened miscarriage. Further assessment should be offered
if the bleeding becomes heavier
or recurs. Otherwise the woman’s next
appointments are likely to be the antenatal midwife-booking visit and the 11–14-week ultrasound scan.
Related Topics