Chapter: Case Study in Obstetrics and Gynaecology: Early Pregnancy
Case Study Reports: Bleeding in Early Pregnancy
BLEEDING IN EARLY PREGNANCY
History
A
41-year-old woman is seen in the early
pregnancy unit because
of vaginal bleeding. She is gravida 4 para 2 having had two previous
normal vaginal deliveries followed by a miscarriage. She has a regular 28-day
menstrual cycle and her last period started
9 weeks ago. She
had slight vaginal
bleeding two weeks
ago and on ultrasound scan
an early intrauterine pregnancy had been visualized with gestational sac of 18 × 12 × 22 mm
diameter and a yolk sac visualized of 4 × 5 × 5 mm. No fetus
was visualized. She was
given an appointment for a repeat ultrasound.
Four days ago her
bleeding became very
heavy and she
passed large clots
which she described as ‘like liver’. She
developed severe abdominal pain which lasted
for about 4 h,
and since then the bleeding
has become very light and she is now pain free.
She
has normal appetite
and no nausea or vomiting.
She has no urinary
or bowel symptoms.
Examination
She
appears well and
is apyrexial. There
are no signs
of anaemia. The
heart rate is 82/min
and blood pressure is 132/78
mmHg. The abdomen
is soft and mildly tender
suprapubi- cally. Speculum shows
the cervix is closed with a small
amount of old blood in the vagina. There is slight uterine
tenderness on bimanual palpation and the
uterus feels normal
size, anteverted and mobile,
with no adnexal
tenderness or cervical
excitation.
Questions
·
What is the diagnosis?
·
What further management is indicated?
Answer:
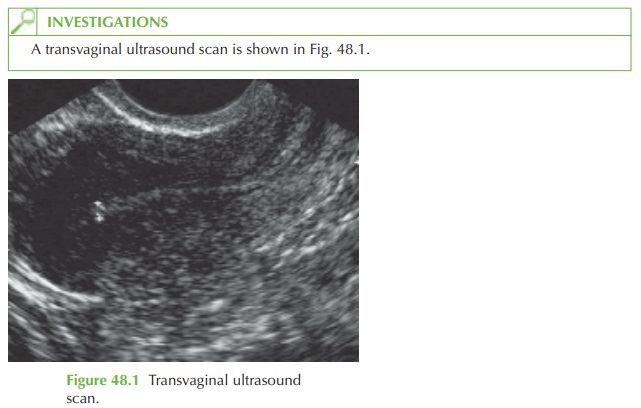
The
ultrasound image shows
a longitudinal view of the uterus with a thin homogenous
endometrium and no evidence of a gestation sac or retained
products of conception. As we know from the previous
report that there
was previously an intrauterine pregnancy, we can conclude that this is a complete
miscarriage. If a previous ultrasound had not been available we would need
to treat the
case as a pregnancy of unknown location and moni- tor
serial serum HCG.
No
further management is needed as the miscarriage is complete and
there are no signs of retained products of conception, or any suggestion of sepsis. Anti-D
is not needed
even if the woman
is Rhesus negative
as the pregnancy is less than 12 weeks’ gestation.
Counselling is the most
important part of this consultation, as explained in case 45.
There is no clear
evidence that a longer interpregnancy interval improves the
outcome in future pregnancies, and the couple should be informed that they may try and conceive
whenever they choose. However, it may be advisable to wait until
after the next menstrual
period (usually 4–6
weeks after a miscarriage) in order to date the
pregnancy.
Reassurance scans are helpful
in future pregnancies and may improve
outcome. In view of
the two consecutive losses, reassurance ultrasound at 7 weeks
and then at intervals
until the 11–14-week scan would be ideal.
Related Topics