Chapter: Case Study in Obstetrics and Gynaecology: Early Pregnancy
Case Study Reports: Bleeding in Early Pregnancy
BLEEDING IN EARLY PREGNANCY
History
A
36-year-old woman presents
with vaginal bleeding
at 8 weeks 3 days’ gestation. She has
never been pregnant
before. Bright red ‘spotting’ commenced 7 days ago, which she thought was normal in early pregnancy. However since then the bleeding
is now almost as heavy as a period.
There are no clots. She
has no abdominal pain. Systemically she
has felt nausea for 3 weeks
and has vomited
occasionally. She had large-loop excision
of the transformation zone
(LLETZ) treatment after
an abnormal smear
6 years ago.
Since then all smears
have been normal.
There is no other significant gynaecological history. She
has regular periods bleeding for 5 days
every 28 days,
and has never
had any known
sexually transmitted infections. In the past she used condoms for contraception.
Examination
The
heart rate is 68/min and blood pressure
is 108/70 mmHg. The abdomen is soft and non-tender. Speculum reveals a normal closed
cervix with a small amount
of fresh blood coming from the cervical canal. Bimanually the
uterus feels bulky
and soft, approximately 10 weeks in size. There
is no cervical excitation or adnexal tenderness.
Questions
·
What is the likely diagnosis and differential diagnosis?
·
What would one expect
to see at scan in this woman
if the pregnancy was normal?
·
How would you manage the patient?
ANSWER
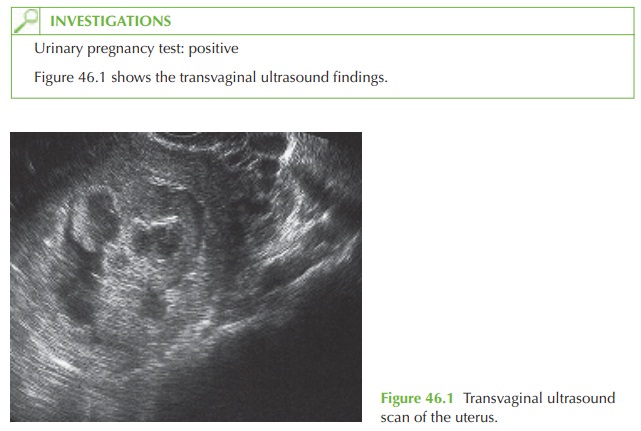
The
ultrasound scan shows a mixed echogenicity appearance in the uterus,
typical of a complete hydatidiform mole (molar
pregnancy, part of the spectrum
of gestational tro- phoblastic disease). There is no recognizable gestational sac or fetus.
This appearance may also be seen occasionally in pregnancies where early fetal demise
has occurred but the sac has not been expelled
(delayed miscarriage) resulting
in cystic degeneration of the placenta.
The incidence of hydatidiform mole
(also known as gestational trophoblastic disease) is approximately 1 in 714. It generally presents with painless
vaginal bleeding though
it may be diagnosed as an incidental finding when ultrasound is
performed for another indication. The classical associations with hyperemesis, thyrotoxicosis or pre-eclampsia are rarely seen in the developed world where diagnosis is generally made in the first
trimester.
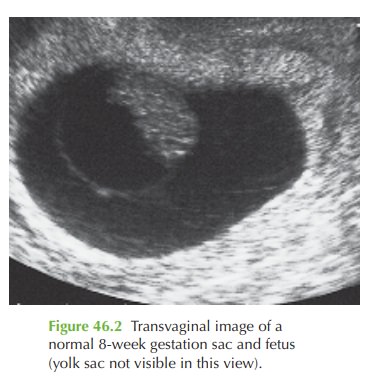
Normal findings at 8 weeks
The
normal findings at 8 weeks
would be a fetus of approximately 18 mm, with
a positive fetal heart
beat. The yolk
sac would still
be visible and
the amniotic sac
would also be seen. The fetus would
be beginning to develop visible
arm and limb
buds and fetal
move- ment may be seen.
Figure 46.2 shows a transvaginal image
of a normal 8-week gestation sac and fetus.
Further management
The
management for suspected molar pregnancy is always evacuation of retained prod- ucts of conception (ERPC),
with urgent histological examination of the
tissue.
Once diagnosis is confirmed by histology, any woman with a confirmed partial or com- plete mole should be referred to a specialist gestational trophoblastic disease
centre (in the UK
in Sheffield, Dundee and Charing
Cross Hospital) for follow-up of human chorionic gonadotrophin (HCG)
levels. Women with persistently raised HCG levels
are offered chemotherapy to destroy the persistent trophoblastic tissue and minimize
the chance of development of choriocarcinoma.
Most women however do not require
chemotherapy as the
HCG becomes negative within a short period
of time. These
women should be advised:
·
not
to become pregnant
again until 6 months after the HCG is normal
·
there is a 1 in 84 chance of a further
molar pregnancy
·
they should have HCG monitoring after
any subsequent pregnancy (whether live birth, fetal loss or termination)
·
the
combined oral contraceptive pill may safely be used once HCG has returned
to normal (previous advice
was to wait for 6 months).
Related Topics