Chapter: Case Study in Obstetrics and Gynaecology: Early Pregnancy
Case Study Reports: Pain and Bleeding in Early Pregnancy
PAIN AND BLEEDING IN EARLY PREGNANCY
History
A
30-year-old woman is referred from her general
practitioner. She is 11 weeks and 2 days gestation and has noticed
dark spotting and mild period-like pains for the last 4 days. Her last
period was 4 months ago but she has a history of polycystic ovarian
syndrome and has an irregular cycle
bleeding for 4–7
days every 5–6
weeks. She had
a positive home pregnancy test because she noticed breast
tenderness, and came for a dating ultrasound scan 4 weeks ago that confirmed
a viable single intrauterine pregnancy. Since then she has
had a booking visit with
the midwife and
all routine blood
tests are normal.
She is gravida 2 para 0. Her last pregnancy 9 months ago ended in a complete
miscarriage at 7 weeks.
There is no other medical
or gynaecological history
of significance.
Examination
She
is apyrexial with normal heart
rate and blood
pressure. The abdomen
is soft and non-
tender. Speculum examination shows a small
cervical ectropion but this is not bleeding. The cervix is closed
and no blood
or abnormal discharge is seen. Bimanual examination reveals an 8–10-week-sized anteverted mobile uterus
with no cervical
excitation, adnexal masses or tenderness.
Questions
·
What is the diagnosis?
·
How
would you investigate and manage this patient?
ANSWER
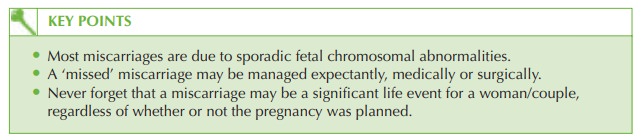
The
diagnosis is of a missed
miscarriage. The alternative terminology for this condition is delayed miscarriage, silent miscarriage or early fetal
demise.
The diagnosis can be made for two reasons. First the fetal heart beat has been seen previously
and is no longer visible.
Second, where the crown–rump length
exceeds 6 mm, a fetal heart beat should be visible on transvaginal ultrasound in all cases
of a viable pregnancy.
Thus the diagnosis could have been made even if the previous
scan result was not known.
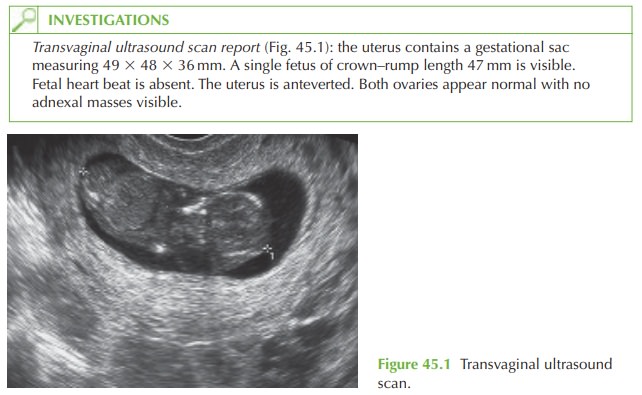
The term ‘empty sac’ (blighted ovum or anembyonic pregnancy) is used where the pregnancy has failed at a much earlier
stage, such that the embryo did not become large enough to be
visualized, but a sac is still seen.
The diagnosis of an empty
gestational sac can
be made when the
mean sac diameter exceeds 20 mm with no visible fetal
pole (fetus). This
is illus- trated in Fig. 45.2.
The management of missed miscarriage and empty sac
is the same.
Management
The
woman needs to discuss how to proceed
now and also what has happened and what
she might expect for future pregnancies. The management of miscarriage is expectant,
medical or surgical. The choice
should be given
with the potential advantages and disad- vantages of each:
·
expectant (‘wait and see’ approach):
·
avoids medical intervention and can be managed completely at home
·
may involve significant pain and bleeding
·
unpredictable time frame – miscarriage may even take several weeks
·
more successful for incomplete miscarriage than for
missed miscarriage
·
medical (oral mifepristone followed
48h later by misoprostol intravaginal tablets):
·
avoids surgical intervention and general anaesthetic
·
the
woman may retain
some feeling of being in control
·
equivalent infection and bleeding
rate as for surgical management (2–3 per cent)
·
surgical evacuation may be indicated if medical management fails
·
surgical (evacuation of retained
products of conception):
·
can
be arranged within
a few days and avoids
prolonged follow-up
·
very low rate of failure (retained
products of conception)
·
small risk of uterine
perforation or anaesthetic complication.
Success rates for missed
miscarriage are generally greater for medical
or surgical manage- ment, whereas expectant management is very successful for incomplete miscarriage.
Further investigation into recurrent miscarriage is usually
reserved for those
with three or more
consecutive losses, because
miscarriage is extremely common and those
couples with two miscarriages are extremely unlikely
to have any underlying cause of miscarriage.
Related Topics